Alcohol abuse
| Alcohol abuse | |
|---|---|
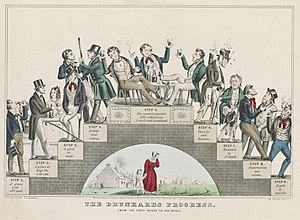 | |
| "The Drunkard’s Progress", 1846 | |
| Specialty | Psychiatry |
| Symptoms | Relationship difficulties, legal problems, problems at work or school, insomnia, irritability, chronic fatigue. |
| Complications | Alcoholic liver disease, Pancreatitis (acute or chronic) |
| Diagnostic method | Clinical history, DSM-5 criteria |
| Treatment | Contingency management, motivational interviewing, Alcoholics Anonymous meeting attendance |
Alcohol abuse encompasses a spectrum of unhealthy alcohol drinking behaviors, ranging from binge drinking to alcohol dependence, in extreme cases resulting in health problems for individuals and large scale social problems such as alcohol-related crimes.
Alcohol abuse was a psychiatric diagnosis in the DSM-IV, and has been merged with alcohol dependence into alcohol use disorder in the DSM-5.[1][2]
Globally, excessive alcohol consumption is the seventh leading risk factor for both death and the burden of disease and injury. In short, except for tobacco, alcohol accounts for a higher burden of disease than any other drug. Alcohol use is a major cause of preventable liver disease worldwide, and alcoholic liver disease is the main alcohol-related chronic medical illness.[3] Millions of men and women of all ages, from adolescents to the elderly, engage in unhealthy drinking in the United States. Alcohol use disorder can affect people from all walks of life. There are many factors that play a role in causing someone to obtain an Alcohol use disorder (AUD), genetics, psychiatric conditions, trauma, environments, even parental drinking habits. [4]
Definitions[]
Risky drinking (also called hazardous drinking) is defined by drinking above the recommended limits:
- greater than 14 standard drinks units per week or greater than 4 standard drinks on a single occasion in men
- greater than 7 standard drinks units per week or greater than 3 standard drinks on a single occasion in women
- any drinking in pregnant women or persons < 21 years old
Binge drinking is a pattern of alcohol consumption that brings blood alcohol concentration ≥ 0.08%, usually corresponds to
- ≥ 5 standard drinks on a single occasion in men
- ≥ 4 standard drinks on a single occasion in women
In the DSM-IV, alcohol abuse and alcohol dependence were defined as distinct disorders from 1994 to 2013. The DSM-5 combined those two disorders into alcohol use disorder with sub-classifications of severity. The DSM-IV definition is no longer used. There is no "alcoholism" diagnosis in medical care.
Alcohol misuse is a term used by United States Preventive Services Task Force to describe a spectrum of drinking behaviors that encompass risky drinking, alcohol abuse, and alcohol dependence (similar meaning to alcohol use disorder but not a term used in DSM).
Signs and symptoms[]
Individuals with an alcohol use disorder will often complain of difficulty with interpersonal relationships, problems at work or school, and legal problems. Additionally, people may complain of irritability and insomnia.[5] Alcohol abuse is also an important cause of chronic fatigue.[6] Signs of alcohol abuse are related to alcohol's effects on organ systems. However, while these findings are often present, they are not necessary to make a diagnosis of alcohol abuse. Signs of alcohol abuse show its drastic effects on the central nervous system, including inebriation and poor judgment; chronic anxiety, irritability, and insomnia. Alcohol's effects on the liver include elevated liver function tests (classically AST is at least twice as high as ALT). Prolonged use leads to cirrhosis and liver failure. With cirrhosis, patients develop an inability to process hormones and toxins. The skin of a patient with alcoholic cirrhosis can feature spider angiomas, palmar erythema and — in acute liver failure — jaundice and ascites. The derangements of the endocrine system lead to the enlargement of the male breasts. The inability to process toxins leads to liver disease, such as hepatic encephalopathy.
Alcohol abuse can result in brain damage which causes impairments in executive functioning such as impairments to working memory and visuospatial function, and can cause an abnormal personality as well as affective disorders to develop.[7][8] Binge drinking is associated with individuals reporting fair to poor health compared to non-binge drinking individuals and which may progressively worsen over time. Alcohol also causes impairment in a person's critical thinking. A person's ability to reason in stressful situations is compromised, and they seem very inattentive to what is going on around them.[9] Social skills are significantly impaired in people suffering from alcoholism due to the neurotoxic effects of alcohol on the brain, especially the prefrontal cortex area of the brain. The prefrontal cortex is responsible for cognitive functions such as working memory, impulse control and decision making. This region of the brain is vulnerable to chronic alcohol-induced oxidative DNA damage.[10] The social skills that are impaired by alcohol abuse include impairments in perceiving facial emotions, difficulty with perceiving vocal emotions and theory of mind deficits; the ability to understand humour is also impaired in alcohol abusers.[11] Adolescent binge drinkers are most sensitive to damaging neurocognitive functions especially executive functions and memory.[12] People who abuse alcohol are less likely to survive critical illness with a higher risk for having sepsis and were more likely to die during hospitalization.[13]
A smaller volume of consumed alcohol has a greater impact on the older adult than it does on a younger individual. As a result, the American Geriatrics Society recommends for an older adult with no known risk factors less than one drink a day or fewer than two drinks per occasion regardless of gender.[14][15][16][17][18][9][19][20][21]
Violence[]
Alcohol abuse is significantly associated with suicide and violence. Alcohol is the most significant health concern in Native American communities because of very high rates of alcohol dependence and abuse; up to 80 percent of suicides and 60 percent of violent acts are a result of alcohol abuse in Native American communities.[22][failed verification]
In the United States alcohol-related violence is related to more severe injuries and chronic cases.[23][citation needed]
Pregnancy[]

Alcohol abuse among pregnant women causes their baby to develop fetal alcohol syndrome. Fetal alcohol syndrome is the pattern of physical abnormalities and the impairment of mental development which is seen with increasing frequency among children with alcoholic mothers.[24] Alcohol exposure in a developing fetus can result in slowed development of the fetal brain, resulting in severe retardation or death. Surviving infants may suffer severe abnormalities such as abnormal eyes, fissures, lips and incomplete cerebella. Some infants may develop lung disease. It is even possible that the baby throughout pregnancy will develop heart defects such as ventricular septal defect or atrial septal defect.[25] Experts suggest that pregnant women take no more than one unit of alcohol per day. However, other organizations advise complete abstinence from alcohol while pregnant.[26]
Adolescence[]
Adolescence and the onset of puberty have both a physiological and social impact on a developing person. About half of grade 12 students have been drunk, and a third binge drink. About 3% drink every day.[27] One of these social impacts is the increase in risk-taking behaviors, such as the emergence of alcohol use.[28] Children aged 16 and under who consume alcohol heavily display symptoms of conduct disorder. Its symptoms include troublesome behaviour in school, constantly lying, learning disabilities and social impairments.[29]
Alcohol abuse during adolescence greatly increases the risk of developing an alcohol use disorder in adulthood due to changes to neurocircuitry that alcohol abuse causes in the vulnerable adolescent brain.[30] Younger ages of initial consumption among males in recent studies has shown to be associated with increased rates of alcohol abuse within the general population.[31]
Societal inequalities (among other factors) have influenced an adolescents decision to consume alcohol.[32][citation needed] One study suggests that girls were scrutinized for "drinking like men", whereas magazines that target the male population sent underlying messages to boys and or men that drinking alcohol was "masculine". (Bogren, 2010)[33]
Causes[]
The cause of alcohol abuse is complex. Alcohol abuse is related to economic and biological origins and is associated with adverse health consequences.[29] Peer pressure influences individuals to abuse alcohol; however, most of the influence of peers is due to inaccurate perceptions of the risks of alcohol abuse.[34] According to Gelder, Mayou and Geddes (2005) easy accessibility of alcohol is one of the reasons people engage in alcohol abuse as this substance is easily obtained in shops. Another influencing factor among adolescents and college students are the perceptions of social norms for drinking; people will often drink more to keep up with their peers, as they believe their peers drink more than they actually do. They might also expect to drink more given the context (e.g. sporting event, house party, etc.).[35][36] This perception of norms results in higher alcohol consumption than is normal. Alcohol abuse is also associated with acculturation, because social and cultural factors such as an ethnic group's norms and attitudes can influence alcohol abuse.[37]
Mental illness[]
A person misusing alcohol may be doing so because they find alcohol's effects provide relief from a psychological problem, such as anxiety or depression. Often both the alcohol misuse and psychological problems need to be treated at the same time.[citation needed]
The numbing effects of alcohol and narcotics can become a coping strategy for traumatized people who are unable to dissociate themselves from the trauma. However, the altered or intoxicated state of the abuser prevents the full consciousness necessary for healing.[38]
Puberty[]
Gender differences may affect drinking patterns and the risk for developing alcohol use disorders.[39] Sensation-seeking behaviors have been previously shown to be associated with advanced pubertal maturation, as well as the company of deviant peers.[28] Early pubertal maturation, as indicated by advanced morphological and hormonal development, has been linked to increased alcohol usage in both male and female individuals.[40] Additionally, when controlling for age, this association between advanced development and alcohol use still held true.[41]
Mechanisms[]
Excessive alcohol use causes neuroinflammation and leads to myelin disruptions and white matter loss. The developing adolescent brain is at increased risk of brain damage and other long-lasting alterations to the brain.[42] Adolescents with an alcohol use disorder damage the hippocampal, prefrontal cortex, and temporal lobes.[30] Chronic alcohol exposure can result in increased DNA damage in the brain, as well as reduced DNA repair and increased neuronal cell death.[43] Alcohol metabolism generates genotoxic acetaldehyde and reactive oxygen species.[44]
Until recently, the underlying mechanisms mediating the link between pubertal maturation and increased alcohol use in adolescence was poorly understood. Now research has suggested that sex steroid hormone levels may play a role in this interaction. When controlling for age, it was demonstrated that elevated estradiol and testosterone levels in male teenagers undergoing pubertal development was linked to increased alcohol consumption.[45] It has been suggested that sex hormones promote alcohol consumption behaviors in teens by stimulating areas in the male adolescent brain associated with reward processing. The same associations with hormone levels were not demonstrated in females undergoing pubertal development. It is hypothesized that sex steroid hormones, such as testosterone and estradiol, are stimulating areas in the male brain that function to promote sensation-seeking and status-seeking behaviors and result in increased alcohol usage.[45]
Additionally, the enzyme TTTan aromatase, which functions in the male brain to convert testosterone to estradiols, has been linked to addictive and reward-seeking behaviors. Therefore, the increased activity of the enzyme may be influencing male adolescent alcohol-usage behaviors during pubertal development.[46] The underlying mechanisms for female alcohol consumption and abuse is still under examination, but is believed to be largely influenced by morphological, rather than hormonal, changes during puberty as well as the presence of deviant peer groups.[40]
The brain goes through dynamic changes during adolescence as a result of advancing pubertal maturation, and alcohol can damage long- and short-term growth processes in teenagers.[47] The rapid effect of drugs releases the neurotransmitter dopamine which acts as reinforcement for the behavior.[48]
Diagnosis[]
DSM-IV[]
Alcohol abuse was defined in the DSM-IV as a maladaptive pattern of drinking. For its diagnosis, at least one of the following criteria had to be fulfilled in the last 12 months:
- Recurrent use of alcohol resulting in a failure to fulfill major role obligations at work, school, or home
- Recurrent alcohol use in situations in which it is physically hazardous
- Recurrent alcohol-related legal problems
- Continued alcohol use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of alcohol [49][50]
DSM-5[]
The alcohol abuse diagnosis is no longer used in the DSM-5 (released in 2013), it is now part of the alcohol use disorder diagnosis. Of the four alcohol abuse criteria, all except the one referring to alcohol-related legal problems are included in the alcohol use disorder criteria.
Screening[]
The Alcohol Use Disorders Identification Test (AUDIT) is considered the most accurate alcohol screening tool for identifying potential alcohol misuse, including dependence.[51] It was developed by the World Health Organisation, designed initially for use in primary healthcare settings with supporting guidance.[52]
Prevention[]

Preventing or reducing the harm has been called for via increased taxation of alcohol, stricter regulation of alcohol advertising and the provision of brief Interventions. Brief Interventions for alcohol abuse reduce the incidence of unsafe sex, sexual violence, unplanned pregnancy and, likely, STD transmission.[53] Information and education on social norms and the harms associated with alcohol abuse delivered via the internet or face-to-face has not been found to result in any meaningful benefit in changing harmful drinking behaviours in young people.[34]
According to European law, individuals who are suffering from alcohol abuse or other related problems cannot be given a driver's license, or if in possession of a license cannot get it renewed. This is a way to prevent individuals driving under the influence of alcohol, but does not prevent alcohol abuse per se.[54]
An individual's need for alcohol can depend on their family's alcohol use history. For instance, if it is discovered that their family history with alcohol has a strong pattern, there might be a need for education to be set in place to reduce the likelihood of reoccurrence (Powers, 2007).[55] However, studies have established that those with alcohol abuse tend to have family members who try to provide help. In many of these occasions the family members would try to help the individual to change or to help improve the individual's lifestyle.
Treatment[]
Youth treatment and intervention should focus on eliminating or reducing the effects of adverse childhood experiences, like childhood maltreatment, since these are common risk factors contributing to the early development of alcohol abuse.[56] Approaches like contingency management and motivational interviewing have shown to be effective means of treating substance use disorder in impulsive adolescents by focusing on positive rewards and redirecting them towards healthier goals.[57] Educating youth about what is considered heavy drinking along with helping them focus on their own drinking behaviors has been shown to effectively change their perceptions of drinking and could potentially help them to avoid alcohol abuse.[58] Completely stopping the use of alcohol, or "abstinence", is the ideal goal of treatment. The motivation required to achieve abstinence is dynamic; family, friends and health practitioners play a role in affecting this motivation.[59]
Some people who abuse alcohol may be able to reduce the amount they drink, also called "drinking in moderation". If this method does not work, the person may need to try abstinence. Abstinence has been regularly achieved by many alcoholics in Alcoholics Anonymous.[medical citation needed]
Mindfulness-based intervention programs (that encourage people to be aware of their own experiences in the present moment and of emotions that arise from thoughts) can reduce the consumption of alcohol.[60][61]
A major barrier to seeking treatment for those struggling with alcohol abuse is the stigma associated with alcohol abuse itself. Those who struggle with alcohol abuse are less likely to utilize substance (or alcohol) abuse treatment services when they perceived higher stigma with alcohol abuse.[62] The stigmatization of individuals who abuse alcohol has been linked to increased levels of depression, increased levels of anxiety, decreased levels of self-esteem, and poor sleeping habits.[63] While negative thoughts and views around the subject of alcohol abuse can keep those struggling with this issue from seeking the treatment they need, there have been several things that have been found to reduce this stigma. Social support can be an effective tool for counteracting the harmful effects of stigma and shame on those struggling with alcohol abuse.[63] Social support can help push those struggling with alcohol abuse to overcome the negative connotation associated with their struggle and finally seek the treatment that they need.
Epidemiology[]
Alcohol abuse is said to be most common in people aged between 15 and 24 years, according to Moreira 2009.[34] However, this particular study of 7275 college students in England collected no comparative data from other age groups or countries.
Causes of alcohol abuse are complex and are likely the combination of many factors, from coping with stress to childhood development. The US Department of Health & Human Services identifies several factors influencing adolescent alcohol use, such as risk-taking, expectancies, sensitivity and tolerance, personality and psychiatric comorbidity, hereditary factors, and environmental aspects.[64]
Studies show that child maltreatment such as neglect, physical, and/or sexual abuse,[56] as well as having parents with alcohol abuse problems,[65] increases the likelihood of that child developing alcohol use disorders later in life. According to Shin, Edwards, Heeren, & Amodeo (2009), underage drinking is more prevalent among teens that experienced multiple types of childhood maltreatment regardless of parental alcohol abuse, putting them at a greater risk for alcohol use disorders.[66] Genetic and environmental factors play a role in the development of alcohol use disorders, depending on age. The influence of genetic risk factors in developing alcohol use disorders increase with age[67] ranging from 28% in adolescence and 58% in adults.[68]
Prognosis[]
Alcohol abuse during adolescence, especially early adolescence (i.e. before age 15), may lead to long-term changes in the brain which leaves them at increased risk of alcoholism in later years; genetic factors also influence age of onset of alcohol abuse and risk of alcoholism.[69] For example, about 40 percent of those who begin drinking alcohol before age 15 develop alcohol dependence in later life, whereas only 10 percent of those who did not begin drinking until 20 years or older developed an alcohol problem in later life.[70] It is not entirely clear whether this association is causal, and some researchers have been known to disagree with this view.[71]
Alcohol use disorders often cause a wide range of cognitive impairments that result in significant impairment of the affected individual. If alcohol-induced neurotoxicity has occurred a period of abstinence for on average a year is required for the cognitive deficits of alcohol abuse to reverse.[72]
College/university students who are heavy binge drinkers (three or more times in the past two weeks) are 19 times more likely to be diagnosed with alcohol dependence, and 13 times more likely to be diagnosed with alcohol abuse compared to non-heavy episodic drinkers, though the direction of causality remains unclear. Occasional binge drinkers (one or two times in past two weeks), were found to be four times more likely to be diagnosed with alcohol abuse or dependence compared to non-heavy episodic drinkers.[9]
Societal and economic costs[]

Alcohol abuse is associated with many accidents, fights, and offences, including criminal. Alcohol is responsible in the world for 1.8 million deaths and results in disability in approximately 58.3 million people. Approximately 40 percent of the 58.3 million people disabled through alcohol abuse are disabled due to alcohol-related neuropsychiatric disorders.[73] Alcohol abuse is highly associated with adolescent suicide. Adolescents who abuse alcohol are 17 times more likely to commit suicide than adolescents who don't drink.[74] Additionally, alcohol abuse increases the risk of individuals either experiencing or perpetrating sexual violence.[53] Alcohol availability and consumption rates and alcohol rates are positively associated with violent crimes, through specifics differ between particular countries and cultures.[75]
By country[]
According to studies of present and former alcoholic drinkers in Canada, 20% of them are aware that their drinking has negatively impacted their lives in various vital areas including finances, work and relationships.[76]
Problems caused by cost about 3.7 billion euro in 2007.[77]
In South Africa, where HIV infection is epidemic, alcohol abusers exposed themselves to double the risk of this infection.[citation needed]
The introduction of alcopops, sweet and pleasantly flavoured alcoholic drinks, was responsible for half of the increase in alcohol abuse in 15- and 16-year-olds, according to one survey in Sweden. In the case of girls, the alcopops, which disguise the taste of alcohol, were responsible for two thirds of the increase. The introduction of alcopops to Sweden was a result of Sweden joining the European Union and adopting the entire European Union law.[78]
Alcohol misuse costs the United Kingdom's National Health Service £3 billion per year. The cost to employers is 6.4 billion pounds sterling per year. These figures do not include the crime and social problems associated with alcohol misuse. The number of women regularly drinking alcohol has almost caught up with men.[79]
In the United States, many people are arrested for drinking and driving. Also, people under the influence of alcohol commit a large portion of various violent crimes, including child abuse, homicide and suicide. In addition, people of minority groups are affected by alcohol-related problems disproportionately, with the exception of Asian Americans.[80] According to criminologist Hung‐En Sung "alcohol is the most widely abused psychoactive substance in the United States".[75]
See also[]
- 0-0-1-3 – a United States Air Force program for alcohol abuse prevention
References[]
- ^ Association, American Psychiatric (2013). Diagnostic and statistical manual of mental disorders : DSM-5 (Fifth ed.). p. 490. ISBN 978-0-89042-557-2.
- ^ "Alcohol Use Disorder: A Comparison Between DSM–IV and DSM–5". November 2013. Archived from the original on 18 May 2015. Retrieved 9 May 2015.
- ^ Fuster, Daniel; Samet, Jeffrey H. (2018-09-27). "Alcohol Use in Patients with Chronic Liver Disease". New England Journal of Medicine. 379 (13): 1251–1261. doi:10.1056/nejmra1715733. ISSN 0028-4793. PMID 30257164. S2CID 52842989.
- ^ "Understanding Alcohol Use Disorder | National Institute on Alcohol Abuse and Alcoholism (NIAAA)". www.niaaa.nih.gov. Retrieved 2021-05-01.
- ^ "Alcohol Alert". NIAA. Retrieved 10 January 2019.
- ^ Aichmüller C, Soyka M (April 2015). "[Fatigue in substance abuse disorders]". Rev Med Suisse (in French). 11 (471): 927–30. PMID 26072600.
- ^ Fitzpatrick LE, Jackson M, Crowe SF (2008). "The relationship between alcoholic cerebellar degeneration and cognitive and emotional functioning". Neurosci Biobehav Rev. 32 (3): 466–85. doi:10.1016/j.neubiorev.2007.08.004. PMID 17919727. S2CID 19875939.
- ^ van Holst RJ, Schilt T (March 2011). "Drug-related decrease in neuropsychological functions of abstinent drug users". Curr Drug Abuse Rev. 4 (1): 42–56. doi:10.2174/1874473711104010042. PMID 21466500.
- ^ Jump up to: a b c Courtney, Kelly E; Polich, John (January 2009). "Binge drinking in young adults: Data, definitions, and determinants". Psychological Bulletin. 135 (1): 142–56. doi:10.1037/a0014414. PMC 2748736. PMID 19210057.
- ^ Fowler AK, Thompson J, Chen L, Dagda M, Dertien J, Dossou KS, Moaddel R, Bergeson SE, Kruman II (2014). "Differential sensitivity of prefrontal cortex and hippocampus to alcohol-induced toxicity". PLOS ONE. 9 (9): e106945. Bibcode:2014PLoSO...9j6945F. doi:10.1371/journal.pone.0106945. PMC 4154772. PMID 25188266.
- ^ Uekermann J, Daum I (May 2008). "Social cognition in alcoholism: a link to prefrontal cortex dysfunction?". Addiction. 103 (5): 726–35. doi:10.1111/j.1360-0443.2008.02157.x. PMID 18412750.
- ^ Amrani, L; De Backer, L; Dom, G (2013). "Piekdrinken op jonge leeftijd: gevolgen voor neurocognitieve functies en genderverschillen" [Adolescent binge drinking: neurocognitive consequences and gender differences] (PDF). Tijdschr Psychiatr (in Dutch). 55 (9): 677–89. PMID 24046246. Archived (PDF) from the original on 2016-03-06.
- ^ "Alcohol Abuse". Juvenile Justice Digest. 35 (2): 7. 2007-01-31. ISSN 0094-2413.
- ^ Michaud, PA (Feb 2007). "Alkoholmissbrauch im Jugendalter – eine Herausforderung für Hausärzte" [Alcohol misuse in adolescents – a challenge for general practitioners]. Therapeutische Umschau (in German). 64 (2): 121–6. doi:10.1024/0040-5930.64.2.121. PMID 17245680.
- ^ Dufour, MC; Archer, L; Gordis, E (1992). "Alcohol and the elderly". Clinics in Geriatric Medicine. 8 (1): 127–41. doi:10.1016/S0749-0690(18)30502-0. PMID 1576571.
- ^ Moos, RH; Schutte, KK; Brennan, PL; Moos, BS (2009). "Older adults' alcohol consumption and late-life drinking problems: A 20-year perspective". Addiction. 104 (8): 1293–1302. doi:10.1111/j.1360-0443.2009.02604.x. PMC 2714873. PMID 19438836.
- ^ Wilson, SR; Fink, A; Verghese, S; Beck, JC; Nguyen, K; Lavori, P (2007). "Adding an alcohol-related risk score to an existing categorical risk classification for older adults: Sensitivity to group differences". Journal of the American Geriatrics Society. 55 (3): 445–50. doi:10.1111/j.1532-5415.2007.01072.x. PMID 17341250. S2CID 22634737.
- ^ Wallace, C; Black, Damien J; Fothergill, Anne (2010). "Integrated assessment of older adults who misuse alcohol". Nursing Standard. 24 (33): 51–58. doi:10.7748/ns2010.04.24.33.51.c7718. PMID 20461924.
- ^ Phil Barker (7 October 2003). Psychiatric and mental health nursing: the craft of caring. London: Arnold. ISBN 978-0-340-81026-2. Archived from the original on 27 May 2013. Retrieved 17 December 2010.
- ^ "Alcoholism and alcohol abuse". PubMed Health. A.D.A.M., Inc. Archived from the original on 3 December 2012. Retrieved 3 December 2012.
- ^ Babor, TF.; Aguirre-Molina, M.; Marlatt, GA.; Clayton, R. (1999). "Managing alcohol problems and risky drinking". Am J Health Promot. 14 (2): 98–103. doi:10.4278/0890-1171-14.2.98. PMID 10724728. S2CID 3267149.
- ^ Jiwa, A.; Kelly, L.; Pierre-Hansen, N. (Jul 2008). "Healing the community to heal the individual: literature review of aboriginal community-based alcohol and substance abuse programs". Can Fam Physician. 54 (7): 1000–1000.e7. PMC 2464791. PMID 18625824.
- ^ Graham K, Livingston M (2011). "The Relationship between Alcohol and Violence – Population, Contextual and Individual Research Approaches". Drug and Alcohol Review. The Journal of Clinical Endocrinology & Metabolism. 30 (5): 453–457. doi:10.1111/j.1465-3362.2011.00340.x. PMC 3170096. PMID 21896066.
- ^ Landesman-Dwyer, S (1982). "Maternal drinking and pregnancy outcome". Applied Research in Mental Retardation. 3 (3): 241–63. doi:10.1016/0270-3092(82)90018-2. PMID 7149705.
- ^ Vorvick, Linda (August 15, 2011). "Fetal alcohol syndrome". PubMed Health. Archived from the original on 20 September 2012. Retrieved 9 April 2012.
- ^ Batra, S.; Wrigley, ECW (April 2005). "Alcohol: The teratogen". Obstetrics & Gynecology. 25 (3): 308–309. doi:10.1080/01443610500106751. PMID 16147750. S2CID 33214831.
- ^ Tripodi, SJ; Bender, K; Litschge, C; Vaughn, MG (January 2010). "Interventions for reducing adolescent alcohol abuse: a meta-analytic review". Archives of Pediatrics & Adolescent Medicine. 164 (1): 85–91. doi:10.1001/archpediatrics.2009.235. PMID 20048247.
- ^ Jump up to: a b Martin, C.; Kelly, T.; Rayens, M.; Brogli, B.; Brenzel, A.; Smith, J.; Omar, O. (December 2002). "Sensation Seeking, Puberty, and Nicotine, Alcohol, and Marijuana Use in Adolescence". Journal of the American Academy of Child & Adolescent Psychiatry. 41 (12): 1495–1502. doi:10.1097/00004583-200212000-00022. PMID 12447037.
- ^ Jump up to: a b McArdle, Paul (27 February 2008). "Alcohol abuse in adolescents". BMJ. 93 (6): 524–527. doi:10.1136/adc.2007.115840. PMID 18305075. S2CID 25568964.
- ^ Jump up to: a b Nixon, K.; McClain, JA. (May 2010). "Adolescence as a critical window for developing an alcohol use disorder: current findings in neuroscience". Current Opinion in Psychiatry. 23 (3): 227–32. doi:10.1097/YCO.0b013e32833864fe. PMC 3149806. PMID 20224404.
- ^ Stewart, S.H. (May 1996). "Alcohol Abuse in Individuals Exposed to Trauma: A Critical Review". Psychological Bulletin. 120 (1): 83–112. CiteSeerX 10.1.1.529.4342. doi:10.1037/0033-2909.120.1.83. PMID 8711018.
- ^ Goodman E, Huang B (May 2002). "Socioeconomic Status, Depressive Symptoms, and Adolescent Substance Use". Archives of Pediatrics & Adolescent Medicine. JAMA. 156 (5): 448–53. doi:10.1001/archpedi.156.5.448. PMID 11980549. Retrieved 22 May 2020.
- ^ Bogren, A (2011). "Gender and alcohol: The swedish press debate". Journal of Gender Studies. 20 (2): 155–169. doi:10.1080/09589236.2011.565196. S2CID 143735279.
- ^ Jump up to: a b c Foxcroft, David R.; Moreira, Maria Teresa; Almeida Santimano, Nerissa M. L.; Smith, Lesley A. (2015-12-29). "Social norms information for alcohol misuse in university and college students". The Cochrane Database of Systematic Reviews (12): CD006748. doi:10.1002/14651858.CD006748.pub4. hdl:10284/8115. ISSN 1469-493X. PMID 26711838.
- ^ Lewis, MA; Litt, DM; Blayney, JA; Lostutter, TW; Granato, H; Kilmer, JR; Lee, CM (2011). "They drink how much and where? Normative perceptions by drinking contexts and their association to college students' alcohol consumption". Journal of Studies on Alcohol and Drugs. 72 (5): 844–853. doi:10.15288/jsad.2011.72.844. PMC 3174028. PMID 21906511.
- ^ Nepomuceno, Thyago Celso C.; de Moura, Jadielson Alves; e Silva, Lúcio Câmara; Cabral Seixas Costa, Ana Paula (December 2017). "Alcohol and violent behavior among football spectators: An empirical assessment of Brazilian's criminalization". International Journal of Law, Crime and Justice. 51: 34–44. doi:10.1016/j.ijlcj.2017.05.001. ISSN 1756-0616.
- ^ Vélez-Mcevoy, M (2005). "Alcohol abuse and ethnicity". AAOHN Journal. 53 (4): 152–155. doi:10.1177/216507990505300402. PMID 15853289.
- ^ Herman, Judith (1997). Trauma and Recovery: The Aftermath of Violence – from domestic abuse to political terror. pp. 44–45. ISBN 978-0-465-08730-3.
- ^ Witt, E. (October 2007). "Puberty, Hormones & Sex Differences in Alcohol Use and Dependence". Neurotoxicology and Teratology. 29 (1): 81–95. doi:10.1016/j.ntt.2006.10.013. PMID 17174531.
- ^ Jump up to: a b Costello, E.; Sung, M.; Worthman, C.; Angold, A. (April 2007). "Pubertal Maturation and the Development of Alcohol Use and Abuse". Drug and Alcohol Dependence. 88: S50–S59. doi:10.1016/j.drugalcdep.2006.12.009. PMID 17275214.
- ^ Westling, E.; Andrews, J.; Hampson, S.; Peterson, M. (2008). "Pubertal timing and substance use: The effects of gender, parental monitoring and deviant peers". Journal of Adolescent Health. 42 (6): 555–563. doi:10.1016/j.jadohealth.2007.11.002. PMC 2435092. PMID 18486864.
- ^ Alfonso-Loeches, S.; Guerri, C. (2011). "Molecular and behavioral aspects of the actions of alcohol on the adult and developing brain". Crit Rev Clin Lab Sci. 48 (1): 19–47. doi:10.3109/10408363.2011.580567. PMID 21657944. S2CID 26880669.
- ^ Fowler AK, Hewetson A, Agrawal RG, Dagda M, Dagda R, Moaddel R, Balbo S, Sanghvi M, Chen Y, Hogue RJ, Bergeson SE, Henderson GI, Kruman II (December 2012). "Alcohol-induced one-carbon metabolism impairment promotes dysfunction of DNA base excision repair in adult brain". J. Biol. Chem. 287 (52): 43533–42. doi:10.1074/jbc.M112.401497. PMC 3527940. PMID 23118224.
- ^ Kruman II, Henderson GI, Bergeson SE (July 2012). "DNA damage and neurotoxicity of chronic alcohol abuse". Exp. Biol. Med. (Maywood). 237 (7): 740–7. doi:10.1258/ebm.2012.011421. PMC 3685494. PMID 22829701.
- ^ Jump up to: a b de Waters, E.; Braams, B.; Crone, E.; Peper, J. (2013). "Pubertal Maturation and Sex Steroids are Related to Alcohol use in Adolescence". Hormones and Behavior. 63 (2): 392–397. doi:10.1016/j.yhbeh.2012.11.018. PMID 23229027. S2CID 5031450.
- ^ Lenz, B.; Heberlein, A.; Bayerlein, K.; Frieling, H.; Kornhuber, J.; Bleich, S.; Hillemacher, T. (2011). "The TTTan aromatase (CYP19A1) polymorphism is associated with compulsive cravings of male patients during alcohol withdrawal". Psychoneuroendocrinology. 36 (8): 1261–1264. doi:10.1016/j.psyneuen.2011.02.010. PMID 21414724. S2CID 29572849.
- ^ "Find Out More, Do More". Office of Substance Abuse, Maine Department of Health and Human Services. Archived from the original on March 10, 2013. Retrieved December 27, 2012.
- ^ Neil R.Carlson, C.Donald Heth. "Psychology: The Science of Behaviour". Pearson Canada Inc, 2010, p. 572.
- ^ Administration (US), Substance Abuse and Mental Health Services; Alcoholism (US), National Institute on Alcohol Abuse and; General (US), Office of the Surgeon (2007). Appendix B: DSM-IV-TR Diagnostic Criteria for Alcohol Abuse and Dependence. Office of the Surgeon General (US).
- ^ Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR). 1. 2000. doi:10.1176/appi.books.9780890423349. ISBN 978-0-89042-334-9.
- ^ "AUDIT – Alcohol Use Disorders Identification Test". Alcohol Learning Centre. 28 June 2010. Archived from the original on 17 March 2012. Retrieved 3 June 2012.
- ^ Supporting guidance Archived 2006-05-02 at the Wayback Machine
- ^ Jump up to: a b Chersich, MF.; Rees, HV. (Jan 2010). "Causal links between binge drinking patterns, unsafe sex and HIV in South Africa: its time to intervene". Int J STD AIDS. 21 (1): 2–7. doi:10.1258/ijsa.2000.009432. PMID 20029060. S2CID 3100905.
- ^ Appenzeller, Brice M.R.; Schneider, Serge; Yegles, Michel; Maul, Armand; Wennig, Robert (2005). "Drugs and chronic alcohol abuse in drivers". Forensic Science International. 155 (2–3): 83–90. doi:10.1016/j.forsciint.2004.07.023. PMID 16226145.
- ^ Rebecca A. (2007). "Alcohol and Drug Abuse Prevention". Psychiatric Annals. 37 (5): 349–358. Archived from the original on 2013-11-05. Retrieved 2013-11-05.
- ^ Jump up to: a b Dube, Shanta R; Anda, Robert F; Felitti, Vincent J; Edwards, Valerie J; Croft, Janet B (2002). "Adverse childhood experiences and personal alcohol abuse as an adult". Addictive Behaviors. 27 (5): 713–725. doi:10.1016/S0306-4603(01)00204-0. PMID 12201379.
- ^ GULLO, M; DAWE, S (2008). "Impulsivity and adolescent substance use: Rashly dismissed as "all-bad"?". Neuroscience & Biobehavioral Reviews. 32 (8): 1507–1518. doi:10.1016/j.neubiorev.2008.06.003. hdl:10072/21184. PMID 18588911. S2CID 21530517.
- ^ Agostinelli, Gina; Grube, Joel (2005). "Effects of Presenting Heavy Drinking Norms on Adolescents? Prevalence Estimates, Evaluative Judgments, and Perceived Standards". Prevention Science. 6 (2): 89–99. doi:10.1007/s11121-005-3408-1. PMID 15889624. S2CID 21984731.
- ^ Haber, Lintzeris, Proude & Lopatko, P, N, E, & O (2009). "Quick Reference Guide to the Treatment of Alcohol Problems" (PDF). Department of Health and Ageing. Retrieved 23 January 2019.CS1 maint: multiple names: authors list (link)
- ^ Chiesa A (Apr 2014). "Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence". Subst Use Misuse. 49 (5): 492–512. doi:10.3109/10826084.2013.770027. PMID 23461667. S2CID 34990668.
- ^ Garland EL (Jan 2014). "Mindfulness training targets neurocognitive mechanisms of addiction at the attention-appraisal-emotion interface". Front Psychiatry. 4 (173): 173. doi:10.3389/fpsyt.2013.00173. PMC 3887509. PMID 24454293.
- ^ Keyes, K.M (15 December 2010). "Stigma and Treatment for Alcohol Disorders in the United States". American Journal of Epidemiology. 172 (12): 1364–1372. doi:10.1093/aje/kwq304. PMC 2998202. PMID 21044992.
- ^ Jump up to: a b Birtel, Michèle D.; Wood, Lisa; Kempa, Nancy J. (June 2017). "Stigma and social support in substance abuse: Implications for mental health and well-being". Psychiatry Research. 252: 1–8. doi:10.1016/j.psychres.2017.01.097. PMID 28237758. S2CID 207453622.
- ^ "Diagnostic Criteria for Alcohol Abuse and Dependence". Alcohol Alert (30 PH 359). October 1995. Archived from the original on 2011-08-17. Retrieved 1 Nov 2013.
- ^ Lieb, R.; Merikangas, K. R.; Höfler, M.; Pfister, H.; Isensee, B.; Wittchen, H.-U. (2002). "Parental alcohol use disorders and alcohol use and disorders in offspring: a community study". Psychological Medicine. 32 (1): 63–78. doi:10.1017/S0033291701004883. PMID 11883731. S2CID 2251288.
- ^ Shin, Sunny Hyucksun; Edwards, Erika; Heeren, Timothy; Amodeo, Maryann (2009). "Relationship between Multiple Forms of Maltreatment by a Parent or Guardian and Adolescent Alcohol Use". American Journal on Addictions. 18 (3): 226–234. doi:10.1080/10550490902786959. PMID 19340641.
- ^ Brown, S. A.; McGue, M.; Maggs, J.; Schulenberg, J.; Hingson, R.; Swartzwelder, S.; Martin, C.; Chung, T.; Tapert, S. F.; Sher, K.; Winters, K. C.; Lowman, C.; Murphy, S. (2008). "A Developmental Perspective on Alcohol and Youths 16 to 20 Years of Age|". Pediatrics. 121 (Suppl 4): S290–S310. doi:10.1542/peds.2007-2243D. PMC 2765460. PMID 18381495.
- ^ Beek, Jenny H. D. A.; Kendler, Kenneth S.; Moor, Marleen H. M.; Geels, Lot M.; Bartels, Meike; Vink, Jacqueline M.; Berg, Stéphanie M.; Willemsen, Gonneke; Boomsma, Dorret I. (2012). "Stable Genetic Effects on Symptoms of Alcohol Abuse and Dependence from Adolescence into Early Adulthood". Behavior Genetics. 42 (1): 40–56. doi:10.1007/s10519-011-9488-8. PMC 3253297. PMID 21818662.
- ^ "Early Age At First Drink May Modify Tween/Teen Risk For Alcohol Dependence". Medical News Today. 21 September 2009. Archived from the original on 13 February 2010.
- ^ Grant, BF.; Dawson, DA. (1997). "Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: results from the National Longitudinal Alcohol Epidemiologic Survey". J Subst Abuse. 9: 103–10. CiteSeerX 10.1.1.473.9819. doi:10.1016/S0899-3289(97)90009-2. PMID 9494942.
- ^ Schwandt, M.L.; Lindell, S.G.; Chen, S.; Higley, J.D.; Suomi, S.J.; Heilig, M.; Barr, C.S. (Feb 2010). "Alcohol response and consumption in adolescent rhesus macaques". Alcohol. 44 (1): 67–80. doi:10.1016/j.alcohol.2009.09.034. PMC 2818103. PMID 20113875.
- ^ Stavro K, Pelletier J, Potvin S (March 2013). "Widespread and sustained cognitive deficits in alcoholism: a meta-analysis". Addict Biol. 18 (2): 203–13. doi:10.1111/j.1369-1600.2011.00418.x. PMID 22264351. S2CID 205401192.
- ^ "Global status report on alcohol and health 2014". World Health Organization. Archived from the original on 15 September 2017. Retrieved 24 July 2017.
- ^ Groves, SA.; Stanley, BH.; Sher, L. (2007). "Ethnicity and the relationship between adolescent alcohol use and suicidal behavior". Int J Adolesc Med Health. 19 (1): 19–25. doi:10.1515/IJAMH.2007.19.1.19. PMID 17458320. S2CID 23339243.
- ^ Jump up to: a b Sung, Hung-En (2016), "Alcohol and Crime", The Blackwell Encyclopedia of Sociology, American Cancer Society, pp. 1–2, doi:10.1002/9781405165518.wbeosa039.pub2, ISBN 9781405165518
- ^ "Send Us a Message." Alcoholism in Canada. Web. 03 Apr. 2012. <http://www.ledgehill.com/resources/addiction-info/alcoholism-in-canada/> Archived March 29, 2012, at the Wayback Machine.
- ^ "Alcohol and costs". AlcoholAction. Archived from the original on 7 December 2014. Retrieved 1 December 2014.
- ^ Romanus, G. (Dec 2000). "Alcopops in Sweden--a supply side initiative". Addiction. 95 Suppl 4 (12s4): S609–19. doi:10.1046/j.1360-0443.95.12s4.12.x. PMID 11218355.
- ^ Dooldeniya, MD.; Khafagy, R.; Mashaly, H.; Browning, AJ.; Sundaram, SK.; Biyani, CS. (Nov 2007). "Lower abdominal pain in women after binge drinking". BMJ. 335 (7627): 992–3. doi:10.1136/bmj.39247.454005.BE. PMC 2072017. PMID 17991983. Archived from the original on 2009-07-26.
- ^ Alcoholism. (2013). Columbia Electronic Encyclopedia, 6th Edition, 1-2.
External links[]
| Classification |
|---|
| Wikimedia Commons has media related to Alcohol abuse. |
- dassa.sa.gov.au
- Rethinking Drinking, National Institute on Alcohol Abuse and Alcoholism
- Alcohol and Crime: Data from 2002 to 2008 Bureau of Justice Statistics
- Healthy Youth! Alcohol & Drug Abuse – U.S. Centers for Disease Control (CDC)
- Alcohol abuse
- Substance abuse

