Herpes zoster ophthalmicus
| Herpes zoster ophthalmicus | |
|---|---|
| Other names | Ophthalmic zoster |
 | |
| Herpes zoster ophthalmicus | |
| Specialty | Ophthalmology |
| Symptoms | Rash of the forehead, swelling of the eyelid, pain and red eye[1] |
| Complications | Vision loss, chronic pain[2] |
| Causes | Reactivation of varicella zoster virus[2] |
| Risk factors | Poor immune function, psychological stress, older age[2] |
| Diagnostic method | Based on symptoms[1] |
| Prevention | Herpes zoster vaccine[1] |
| Medication | Antiviral pills such as acyclovir, steroid eye drops[1] |
| Frequency | Up to 125,000 per year (US)[3] |
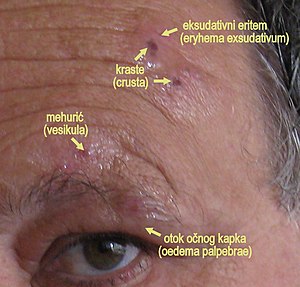
Herpes zoster ophthalmicus (HZO), also known as ophthalmic zoster, is shingles involving the eye or the surrounding area.[1] Symptoms generally include a rash of the forehead with swelling of the eyelid.[1] There may also be eye pain, eye redness, and light sensitivity.[1] Before the rash appears tingling may occur in the forehead along with a fever.[1][3] Complications may include vision loss, increased pressure within the eye, and chronic pain.[2][1]
The underlying mechanism involves a reactivation of the varicella zoster virus within the trigeminal ganglion supplying the ophthalmic nerve (the first division of the trigeminal nerve).[2] Risk factors include poor immune function, psychological stress, and older age.[2] Diagnosis is generally based on symptoms.[1]
Treatment is generally with antiviral pills such as acyclovir.[1] Steroid eye-drops and drops to dilate the pupil may also be used.[1] The herpes zoster vaccine is recommended for prevention in those over the age of 50.[1] HZO is the second most common manifestation of shingles, the first being involvement of skin of the thorax.[citation needed] Shingles affects up to one half million people in the United States per year, of which 10% to 25% is HZO.[3][2]
Signs and symptoms[]
Skin[]
- Viral prodrome
- Preherpetic neuralgia
- Rash, transitioning from papules to vesicles to pustules to scabs.
- Hutchinson's sign: cutaneous involvement of the tip of the nose, indicating nasociliary nerve involvement. A positive Hutchinson's sign increases the likelihood of ocular complications associated with HZO.
- Disseminated distribution in individuals with immunodeficiency.[4]
Cornea[]

- Epithelial: punctate epithelial erosions and : often have anterior stromal infiltrates. Onset 2 to 3 days after the onset of the rash, resolving within 2–3 weeks. Common.
- Stromal:
- Nummular keratitis: have anterior stromal granular deposits. Occurs within 10 days of onset of rash. Uncommon
- Necrotising interstitial keratitis: Characterised by stromal infiltrates, corneal thinning and possibly perforation. Occurs between 3 months and several years after onset of rash. Rare.
- Disciform Keratitis (Disciform Endotheliitis): a disc of , folds in Descemet's membrane, mild inflammation evident within the anterior chamber and fine keratic precipitates. Chronic. Occurs between 3 months and several years after the onset of the rash. Uncommon.
- Neurotrophic: corneal nerve damage causes persistent epithelial defect, thinning and even perforation. Cornea becomes susceptible to bacterial and fungal keratitis. Chronic. Late onset. Uncommon.
- Mucous plaques: linear grey elevations loosely adherent to the underlying diseased epithelium/stroma. Chronic. Onset between 3 months and several years after the onset of the rash.[4]
Uveal[]
Anterior uveitis develops in 40–50% of cases with HZO within 2 weeks of onset of the skin rashes. Typical HZO keratitis at least mild iritis, especially if Hutchinson's sign is positive for the presence of vesicles upon the tip of the nose.
Features:[5]
This non-granulomatous iridocyclitis is associated with:
- Small keratic precipitates
- Mild aqueous flare
- Occasionally haemorrhagic hypopyon
HZO uveitis is associated with complications such as and secondary glaucoma are not uncommon. Complicated cataract may develop in the late stages of the disease.
Anatomy[]
HZO is due to reactivation of VZV within the trigeminal ganglion. The trigeminal ganglion give rise to the three divisions of cranial nerve V (CN V), namely the ophthalmic nerve, the maxillary nerve, and the mandibular nerve. VZV reactivation in trigeminal ganglion predominantly affects the ophthalmic nerve, for reasons not clearly known.[citation needed] The ophthalmic nerve gives rise to three branches: the supraorbital nerve, the supratrochlear nerve, and the nasociliary nerve. Any combination of these nerves can be affected in HZO, although the most feared complications occur with nasociliary nerve involvement, due to its innervation of the eye.[citation needed] The supraorbital and supratrochlear nerves mainly innervate the skin of the forehead.[citation needed] The frontal nerve is more commonly affected than the nasociliary nerve or lacrimal nerve.[5]
Treatment[]
Treatment is usually with antivirals such as acyclovir, valacyclovir, or famcyclovir by mouth.[1] There is uncertainty as to the difference in effect between these three antivirals.[6] Antiviral eye drops have not been found to be useful.[3] These medications work best if started within 3 days of the start of the rash.[2]
Cycloplegics prevent synechiae from forming.
References[]
- ^ Jump up to: a b c d e f g h i j k l m n "Herpes Zoster Ophthalmicus - Eye Disorders". Merck Manuals Professional Edition. Retrieved 21 December 2019.
- ^ Jump up to: a b c d e f g h Shaikh S, Ta CN (November 2002). "Evaluation and management of herpes zoster ophthalmicus". American Family Physician. 66 (9): 1723–30. PMID 12449270.
- ^ Jump up to: a b c d "Herpetic Corneal Infections: Herpes Zoster Ophthalmicus". www.aao.org. Retrieved 21 December 2019.
- ^ Jump up to: a b Denniston AK, Murray PI (2009-06-11). Oxford Handbook of Ophthalmology. ISBN 9780199552641.
- ^ Jump up to: a b Khurana AK (2008). Comprehensive Ophthalmology. ISBN 9781905740789.
- ^ Schuster AK, Harder BC, Schlichtenbrede FC, Jarczok MN, Tesarz J (November 2016). Cochrane Eyes and Vision Group (ed.). "Valacyclovir versus acyclovir for the treatment of herpes zoster ophthalmicus in immunocompetent patients". The Cochrane Database of Systematic Reviews. 11: CD011503. doi:10.1002/14651858.CD011503.pub2. PMC 6464932. PMID 27841441.
External links[]
| Wikimedia Commons has media related to Herpes zoster ophthalmicus. |
| Classification | |
|---|---|
| External resources |
- Varicella zoster virus-associated diseases
- Ophthalmology
