Mycobacterium
| Mycobacterium | |
|---|---|

| |
| TEM micrograph of M. tuberculosis. | |
| Scientific classification | |
| Domain: | Bacteria
|
| Phylum: | "Actinobacteria"
|
| Class: | Actinobacteria
|
| Order: | |
| Family: | |
| Genus: | Mycobacterium Lehmann & Neumann 1896[1]
|
| Species | |
|
See below. | |
| Synonyms[2] | |
| |
Mycobacterium is a genus of Actinobacteria, given its own family, the Mycobacteriaceae. Over 190 species are recognized in this genus.[3] This genus includes pathogens known to cause serious diseases in mammals, including tuberculosis (Mycobacterium tuberculosis) and leprosy (Mycobacterium leprae) in humans.[4] The Greek prefix myco- means "fungus," alluding to the way mycobacteria have been observed to grow in a mold-like fashion on the surface of cultures.[5] It is acid fast and cannot be stained by the Gram stain procedure.
Microbiologic characteristics[]
Metabolism and morphology[]
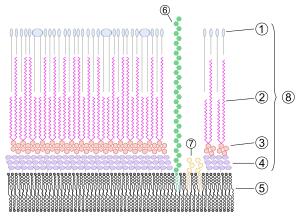
Mycobacteria are aerobic. They are bacillary in form, at least in most phases that have attracted human microbiological attention to date; they are straight or slightly curved rods between 0.2 and 0.6 µm wide and between 1.0 and 10 µm long. They are generally nonmotile bacteria, except for the species Mycobacterium marinum, which has been shown to be motile within macrophages. They are characteristically acid-fast.[4] Mycobacteria have an outer membrane.[6] They possess capsules, and most do not form endospores. M. marinum and perhaps M. bovis have been shown to sporulate;[7] however, this has been contested by further research.[8] The distinguishing characteristic of all Mycobacterium species is that the cell wall is thicker than in many other bacteria, being hydrophobic, waxy, and rich in mycolic acids/mycolates. The cell wall consists of the hydrophobic mycolate layer and a peptidoglycan layer held together by a polysaccharide, arabinogalactan. The cell wall makes a substantial contribution to the hardiness of this genus. The biosynthetic pathways of cell wall components are potential targets for new drugs for tuberculosis.[9]
Many Mycobacterium species adapt readily to growth on very simple substrates, using ammonia or amino acids as nitrogen sources and glycerol as a carbon source in the presence of mineral salts. Optimum growth temperatures vary widely according to the species and range from 25 °C to over 50 °C.[citation needed]
Most Mycobacterium species, including most clinically relevant species, can be cultured in blood agar.[10] However, some species grow very slowly due to extremely long reproductive cycles—M. leprae, may take more than 20 days to proceed through one division cycle (for comparison, some E. coli strains take only 20 minutes), making laboratory culture a slow process.[4] In addition, the availability of genetic manipulation techniques still lags far behind that of other bacterial species.[11]
A natural division occurs between slowly- and rapidly-growing species. Mycobacteria that form colonies clearly visible to the naked eye within 7 days on subculture are termed rapid growers, while those requiring longer periods are termed slow growers.[citation needed]
Pigmentation[]
Some mycobacteria produce carotenoid pigments without light. Others require photoactivation for pigment production.[citation needed]
- Photochromogens (Group I)
- Produce nonpigmented colonies when grown in the dark and pigmented colonies only after exposure to light and reincubation.[citation needed]
- Ex: M. kansasii, M. marinum, M. simiae.
- Scotochromogens (Group II)
- Produce deep yellow to orange colonies when grown in the presence of either the light or the dark.[citation needed]
- Ex: M. scrofulaceum, M. gordonae, M. szulgai.
- Non-chromogens (Groups III and IV)
- Nonpigmented in the light and dark or have only a pale yellow, buff or tan pigment that does not intensify after light exposure.[citation needed]
- Ex: M. tuberculosis, M. avium-intra-cellulare, M. bovis, M. ulcerans, M. xenopi
- Ex: M. fortuitum, M. chelonae
Staining characteristics[]
Mycobacteria are classical acid-fast organisms.[12] Stains used in evaluation of tissue specimens or microbiological specimens include , Ziehl–Neelsen stain, and Kinyoun stain.[citation needed]
Mycobacteria appear phenotypically most closely related to members of Nocardia, Rhodococcus, and Corynebacterium.[citation needed]
Ecology[]
Mycobacteria are widespread organisms, typically living in water (including tap water treated with chlorine) and food sources. Some, however, including the tuberculosis and the leprosy organisms, appear to be obligate parasites and are not found as free-living members of the genus.[citation needed]
Pathogenicity[]
Mycobacteria can colonize their hosts without the hosts showing any adverse signs. For example, billions of people around the world have asymptomatic infections of M. tuberculosis (Latent TB).[citation needed]
Mycobacterial infections are notoriously difficult to treat. The organisms are hardy due to their cell wall, which is neither truly Gram negative nor positive. In addition, they are naturally resistant to a number of antibiotics that disrupt cell-wall biosynthesis, such as penicillin. Due to their unique cell wall, they can survive long exposure to acids, alkalis, detergents, oxidative bursts, lysis by complement, and many antibiotics. Most mycobacteria are susceptible to the antibiotics clarithromycin and rifamycin, but antibiotic-resistant strains have emerged.[citation needed]
As with other bacterial pathogens, M. tuberculosis produces a number of surface and secreted proteins that contribute to its virulence. However, the mechanism by which these proteins contribute to virulence remains unknown.[13]
Medical classification[]
Mycobacteria can be classified into several major groups for purpose of diagnosis and treatment: M. tuberculosis complex, which can cause tuberculosis: M. tuberculosis, M. bovis, M. africanum, and M. microti; M. leprae, which causes Hansen's disease or leprosy; nontuberculous mycobacteria (NTM) are all the other mycobacteria, which can cause pulmonary disease resembling tuberculosis, lymphadenitis, skin disease, or disseminated disease.[citation needed]
Mycosides[]
Mycosides are glycolipid compounds isolated from Mycobacterium that contain varying lipid, carbohydrate, and amino acid moieties.[14] Mycosides A and B have 18 and 20 carbon atoms, respectively.[15]
Genomics[]
Comparative analyses of mycobacterial genomes have identified several conserved indels and signature proteins that are uniquely found in all sequenced species from the genus Mycobacterium.[16][17] Additionally, 14 proteins are found only in the species from the genera Mycobacterium and Nocardia, suggesting that these two genera are closely related.[17]
The genomes of some mycobacteria are quite large when compared to other bacteria. For instance, the genome of M. vulneris encodes 6,653 proteins, which is larger than that of small eukaryotes such as yeast (which encodes only ~6,000 proteins).[18]
Evolution[]
M. ulcerans evolved from M. marinum.[19]
Species[]

The blue triangle corresponds to tubercle bacilli sequences that are identical or differing by a single nucleotide. The sequences of the genus Mycobacterium that matched most closely to those of M. tuberculosis were retrieved from the BIBI database (http://pbil.univ-lyon.fr/bibi/[permanent dead link]) and aligned with those obtained for 17 smooth and MTBC strains. The unrooted neighbor-joining tree is based on 1,325 aligned nucleotide positions of the 16S rRNA gene. The scale gives the pairwise distances after Jukes-Cantor correction. Bootstrap support values higher than 90% are indicated at the nodes.
Phenotypic tests can be used to identify and distinguish different mycobacteria species and strains. In older systems, mycobacteria are grouped based upon their appearance and rate of growth. However, these are symplesiomorphies, and more recent classification is based upon cladistics. Over 100 species are currently recognised.
O'Neill and coworkers recently presented a comprehensive phylogenetic analysis based on an alignment of core genomes of 57 strains of bacteria, including all available mycobacteria.[20]
Slowly growing[]
Runyon's group I, II and III
Mycobacterium tuberculosis complex[]
Also see main article about Mycobacterium tuberculosis complex
- Mycobacterium tuberculosis complex (MTBC) members are causative agents of human and animal tuberculosis. Species in this complex include:
- M. africanum
- M. bovis
- M. bovis BCG
- M. canetti
- M. caprae
- M. microti
- M. pinnipedii
- M. tuberculosis, the major cause of human tuberculosis
Mycobacterium avium complex[]
- Mycobacterium avium complex (MAC) is a group of species that, in a disseminated infection but not lung infection, used to be a significant cause of death in AIDS patients. Species in this complex include:
- M. avium
- M. avium paratuberculosis, which has been implicated in Crohn's disease in humans and is the causative agent of Johne's disease in cattle and sheep
- M. avium silvaticum
- M. avium "hominissuis"
- M. colombiense
- M. indicus pranii
- M. intracellulare
Mycobacterium gordonae clade[]
Mycobacterium kansasii clade[]
Mycobacterium nonchromogenicum/terrae clade[]
Mycolactone-producing mycobacteria[]
- M. ulcerans, which causes the "Buruli", or "Bairnsdale" ulcer
Mycobacterium simiae clade[]
- M. florentinum
- M. genavense
- M. heidelbergense
- M. interjectum
- M. kubicae
- M. lentiflavum
- M. montefiorense
- M. palustre
- M. parascrofulaceum
- M. simiae
- M. triplex
Ungrouped[]
- M. bohemicum
- M. botniense
- M. branderi
- M. celatum
- M. chimaera
- M. conspicuum
- M. cookii
- M. doricum
- M. farcinogenes
- M. haemophilum
- M. heckeshornense
- M. intracellulare
- M. lacus
- M. leprae, which causes leprosy
- M. lepraemurium
- M. lepromatosis, another (less significant) cause of leprosy, described in 2008
- M. malmoense
- M. marinum, causes a rare disease called Aquarium granuloma.
- M. neoaurum
- M. monacense
- M. murale
- M. nebraskense
- M. saskatchewanense
- M. scrofulaceum
- M. shimoidei
- M. szulgai
- M. tusciae
- M. xenopi
Intermediate growth rate[]
Rapidly growing[]
Mycobacterium abscessus clade[]
Together they are known as the M. abscessus complex
Mycobacterium chelonae clade[]
Mycobacterium fortuitum clade[]
- M. boenickei
- M. brisbanense
- M. cosmeticum
- M. fortuitum
- M. houstonense
- M. mageritense
- M. neworleansense
- M. peregrinum
- M. porcinum
- M. senegalense
- M. septicum
Mycobacterium mucogenicum clade[]
Mycobacterium parafortuitum clade[]
Mycobacterium vaccae clade[]
- M. aurum
- M. vaccae
CF (Cystic Fibrosis)[]
Ungrouped[]
- M. agri
- M. aichiense
- M. alvei
- M. arupense
- M. brumae
- M. canariasense
- M. chubuense
- M. conceptionense
- M. confluentis
- M. duvalii
- M. elephantis
- M. flavescens
- M. gadium
- M. gilvum
- M. hassiacum
- M. holsaticum
- M. iranicum
- M. komossense
- M. madagascariense
- M. moriokaense
- M. obuense
- M. phlei
- M. psychrotolerans
- M. pulveris
- M. pyrenivorans
- M. smegmatis
- M. goodii
- M. wolinskyi
- M. sphagni
- M. thermoresistibile
- M. vanbaalenii
Ungrouped[]
- M. arosiense
- M. aubagnense
- M. chlorophenolicum
- M. fluoroanthenivorans
- M. kumamotonense
- M. novocastrense
- M. parmense
- M. poriferae
- M. rhodesiae
- M. seoulense
- M. tokaiense
Proposed division of the genus[]
Gupta et al. have, based on the analysis of 150 species in the genus, proposed dividing Mycobacterium into five genera.[21] The proposed new genera are:
- Mycobacterium based on the Tuberculosis-Simiae clade
- Mycolicibacterium based on the Fortuitum-Vaccae clade
- Mycolicibacter based on the Terrae clade
- Mycolicibacillus based on the Triviale clade
- Mycobacteroides based on the Abscessus-Chelonae clade
This nomenclatural division of the genus Mycobacterium has been opposed on the basis that it unnecessarily complicates medical diagnoses and treatments.[22]
Mycobacteriophage[]
Mycobacteria can be infected by mycobacteriophages, bacterial viruses that may be used in the future to treat tuberculosis and related diseases by phage therapy. The procedure may not go into practice in the case of Mtb for some time, as bacteriophage particles cannot penetrate into the tuberculosis bacilli, or clumps.[citation needed]
Diagnosis[]
Mycobacteria can be grown by bacterial culture, but are slowly growing, and 6-8 weeks are generally required before concluding that there is no mycobacterial growth.[23]
In anatomic pathology specimens, immunohistochemistry and modifications of Ziehl–Neelsen staining (such as the ) have comparable diagnostic utility. Both of them are superior to traditional Ziehl–Neelsen stain.[24]
References[]
- ^ Lehmann KB, Neumann R. (1896). Atlas und Grundriss der Bakteriologie und Lehrbuch der speziellen bakteriologischen Diagnostik [Atlas and Outline of Bacteriology and Textbook of Special Bacteriological Diagnostics] (1st ed.). München: J.F. Lehmann.CS1 maint: uses authors parameter (link)
- ^ Euzéby JP, Parte AC. "Mycobacterium". List of Prokaryotic names with Standing in Nomenclature (LPSN). Retrieved June 16, 2021.CS1 maint: uses authors parameter (link)
- ^ King, HC; Khera-Butler, T; James, P; Oakley, BB; Erenso, G; Aseffa, A; Knight, R; Wellington, EM; Courtenay, O (2017). "Environmental reservoirs of pathogenic mycobacteria across the Ethiopian biogeographical landscape". PLOS ONE. 12 (3): e0173811. Bibcode:2017PLoSO..1273811K. doi:10.1371/journal.pone.0173811. PMC 5363844. PMID 28333945.
- ^ Jump up to: a b c Ryan KJ, Ray CG, eds. (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. ISBN 0-8385-8529-9.
- ^ Kerr, James H.; Barrett, Terry L. (1 December 1994). "Atypical Mycobacterial Diseases". In James, William D. (ed.). Military Dermatology. Washington D.C.: Office of the Surgeon General. p. 401. CiteSeerX 10.1.1.175.3823. Retrieved 10 November 2020.
- ^ Niederweis M, Danilchanka O, Huff J, Hoffmann C, Engelhardt H (2010). "Mycobacterial outer membranes: in search of proteins". Trends in Microbiology. 18 (3): 109–16. doi:10.1016/j.tim.2009.12.005. PMC 2931330. PMID 20060722.
- ^ Ghosh, Jaydip; Larsson, Pontus; Singh, Bhupender; Pettersson, B M Fredrik; Islam, Nurul M; Nath Sarkar, Sailendra; Dasgupta, Santanu; Kirsebom, Leif A (2009). "Sporulation in mycobacteria". Proceedings of the National Academy of Sciences of the United States of America. 106 (26): 10781–86. Bibcode:2009PNAS..10610781G. doi:10.1073/pnas.0904104106. PMC 2705590. PMID 19541637.
- ^ Traag, BA; Driks, A; Stragier, P; Bitter, W; Broussard, G; Hatfull, G; Chu, F; Adams, KN; Ramakrishnan, L; Losick, R (Jan 2010). "Do mycobacteria produce endospores?". Proc Natl Acad Sci U S A. 107 (2): 878–81. Bibcode:2010PNAS..107..878T. doi:10.1073/pnas.0911299107. PMC 2818926. PMID 20080769.
- ^ Bhamidi S (2009). "Mycobacterial Cell Wall Arabinogalactan". Bacterial Polysaccharides: Current Innovations and Future Trends. Caister Academic Press. ISBN 978-1-904455-45-5.
- ^ Lagier, Jean-Christophe; Edouard, Sophie; Pagnier, Isabelle; Mediannikov, Oleg; Drancourt, Michel; Raoult, Didier (2015). "Current and Past Strategies for Bacterial Culture in Clinical Microbiology". Clinical Microbiology Reviews. 28 (1): 208–36. doi:10.1128/CMR.00110-14. PMC 4284306. PMID 25567228.
- ^ Parish T, Brown A, eds. (2009). Mycobacterium: Genomics and Molecular Biology. Caister Academic Press. ISBN 978-1-904455-40-0.
- ^ McMurray DN (1996). "Mycobacteria and Nocardia". In Baron S; et al. (eds.). Baron's Medical Microbiology (4th ed.). Univ of Texas Medical Branch. ISBN 0-9631172-1-1.
- ^ McCann, Jessica R.; Kurtz, Sherry; Braunstein, Miriam (2009). "Secreted and Exported Proteins Important to Mycobacterium tuberculosis Pathogenesis". In Wooldridge, Karl (ed.). Bacterial Secreted Proteins: Secretory Mechanisms and Role in Pathogenesis. Norfolk, UK: Caister Academic Press. pp. 265–97. ISBN 978-1904455424.
- ^ Smith, Donald W.; Randall, H. M.; Maclennan, A. P.; Lederer, E. (June 1960). "Mycosides: a New Class of Type-Specific Glycolipids of Mycobacteria". Nature. 186 (4728): 887–888. Bibcode:1960Natur.186..887S. doi:10.1038/186887a0. PMID 13831939. S2CID 4149360.
- ^ "fatty alcohols and aldehydes". Archived from the original on 2012-06-25. Retrieved 2007-08-05.
- ^ Gao, B.; Paramanathan, R.; Gupta, R. S. (2006). "Signature proteins that are distinctive characteristics of Actinobacteria and their subgroups". Antonie van Leeuwenhoek. 90 (1): 69–91. doi:10.1007/s10482-006-9061-2. PMID 16670965. S2CID 25817892.
- ^ Jump up to: a b Gao, B.; Gupta, R. S. (2012). "Phylogenetic Framework and Molecular Signatures for the Main Clades of the Phylum Actinobacteria". Microbiology and Molecular Biology Reviews. 76 (1): 66–112. doi:10.1128/MMBR.05011-11. PMC 3294427. PMID 22390973.
- ^ Croce, Olivier; Robert, Catherine; Raoult, Didier; Drancourt, Michel (2014-05-08). "Draft Genome Sequence of Mycobacterium vulneris DSM 45247T". Genome Announcements. 2 (3). doi:10.1128/genomeA.00370-14. ISSN 2169-8287. PMC 4014686. PMID 24812218.
- ^ Vandelannoote K, Meehan CJ, Eddyani M, Affolabi D, Phanzu DM, Eyangoh S, Jordaens K, Portaels F, Mangas K, Seemann T, Marsollier L, Marion E, Chauty A, Landier J, Fontanet A, Leirs H, Stinear TP, de Jong BC1 (2017). "Multiple Introductions and Recent Spread of the Emerging Human Pathogen Mycobacterium ulcerans across Africa". Genome Biol Evol 9(3):414–26
- ^ O'Neill, MB; Mortimer, TD; Pepperell, CS (2015). "Diversity of Mycobacterium tuberculosis across Evolutionary Scales". PLOS Pathog. 11 (11): e1005257. doi:10.1371/journal.ppat.1005257. PMC 4642946. PMID 26562841.
- ^ Gupta, RS; Lo, B; Son, J (2018). "Phylogenomics and comparative genomic studies robustly support division of the genus Mycobacterium into an emended genus Mycobacterium and four novel genera". Front Microbiol. 9: 67. doi:10.3389/fmicb.2018.00067. PMC 5819568. PMID 29497402.
- ^ Tortoli E, Brown-Elliott BA, Chalmers JD, Cirillo DM, Daley CL, Emler S, Floto RA, Garcia MJ, Hoefsloot W, Koh WJ, Lange C, Loebinger M, Maurer FP, Morimoto K, Niemann S, Richter E, Turenne CY, Vasireddy R, Vasireddy S, Wagner D, Wallace Jr RJ, Wengenack N, van Ingen J. (2019). "Same meat, different gravy: Ignore the new names of mycobacteria". Eur Respir J. 54 (1): 1900795. doi:10.1183/13993003.00795-2019. PMID 31296783.
- ^ Pfyffer, G. E.; Wittwer, F. (2012). "Incubation Time of Mycobacterial Cultures: How Long Is Long Enough To Issue a Final Negative Report to the Clinician?". Journal of Clinical Microbiology. 50 (12): 4188–4189. doi:10.1128/JCM.02283-12. ISSN 0095-1137. PMC 3502948. PMID 23052304.
- ^ Crothers, Jessica W; Laga, Alvaro C; Solomon, Isaac H (2021). "Clinical Performance of Mycobacterial Immunohistochemistry in Anatomic Pathology Specimens". American Journal of Clinical Pathology. 155 (1): 97–105. doi:10.1093/ajcp/aqaa119. ISSN 0002-9173. PMID 32915191.
Further reading[]
- Diagnosis and Treatment of Disease Caused by Nontuberculous Mycobacteria. American Thoracic Society. Am J Respiratory and Critical Care Medicine. Aug 1997 156(2) Part 2 Supplement
- RIDOM: Ribosomal Differentiation of Medical Microorganisms
- J.P. Euzéby: List of Prokaryotic Names with Standing in Nomenclature – Genus Mycobacterium
External links[]
- Tuberculist: Genome annotation database
- MTB Sysborg: Genome annotation database from the Institute of Genomics and Integrative Biology
- TB Structural Genomics Consortium: Structures of Mycobacterium tuberculosis proteins
- MycDB: Mycobacterium database
- TBDB: Tuberculosis database
- Mycobacterium genomes and related information at PATRIC, a Bioinformatics Resource Center funded by NIAID
- Frequently Asked Questions about NTM Lung Disease
- PRASITE: Identification of mycobacteria
- Acid-fast bacilli
- Corynebacterineae
- Tuberculosis
- Bacteriology
- Bacterial diseases
- Bacteria genera
- Mycobacteria
- Pathogenic bacteria
- Infectious causes of cancer