Neuromuscular monitoring


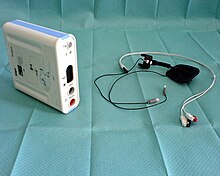
In anesthesia, neuromuscular blocking agents may be required to facilitate endotracheal intubation and provide optimal surgical conditions. When neuromuscular blocking agents are administered, neuromuscular function of the patient must be monitored.[1] Neuromuscular function monitoring is a technique that involves the electrical stimulation of a motor nerve and monitoring the response of the muscle supplied by that nerve.[2] It may be used from the induction of to recovery from neuromuscular blockade. Importantly, it is used to confirm adequacy of recovery after the administration of neuromuscular blocking agents.[3] The response of the muscles to electrical stimulation of the nerves can be recorded subjectively (qualitative) or objectively (quantitatively). Quantitative techniques include electromyography, acceleromyography, kinemyography, phonomygraphy and mechanomyography. Neuromuscular monitoring is recommended when neuromuscular-blocking drugs have been part of the general anesthesia and the doctor wishes to avoid postoperative residual curarization (PORC) in the patient, that is, the residual paralysis of muscles stemming from these drugs.
When train of four monitoring is "used continuously, each set (train) of stimuli normally is repeated every 10th to 12th second. Each stimulus in the train causes the muscle to contract, and 'fade' in the response provides the basis for evaluation." These sets are called trains because their shape bears the resemblance of a train.[4] In train of four monitoring, "peripheral nerve stimulation can ensure proper medication dosing and thus decrease the incidence of side effects" by "assessing the depth of neuromuscular blockade".[5]
Before the patient is fully awake, voluntary muscle testing is not possible and indirect clinical tests, such as apparent muscle tone and pulmonary compliance, can be affected by factors other than PORC. Direct neuromuscular monitoring avoids these problems and allows the doctor to remedy PORC before it becomes a source of patient distress.[6][7][8][9][10]
Patterns of nerve stimulation[]
Various nerve stimulation patterns may be used in neuromuscular function monitoring and the response to these stimulation patterns is used to assess the depth of neuromuscular blockade.
Some patterns of stimulation used today include, single twitch (ST), train-of four (TOF),[11] double burst stimulation (DBS), tetanic stimulation
and the post tetanic count.[12]
Monitoring the response of the muscle to nerve stimulation[]
The response of the muscle to stimulation of the nerve supplying it can be assessed by subjective (visual or tactile) techniques or quantitative (objective) devices that provide a numeric value relating to the depth of neuromuscular blockade.
Quantitative (objective) neuromuscular monitors[]
Quantitative neuromuscular monitors can be subdivided into monitors that measure the electrical response, the compound evoked muscle action potential, and those that monitor the contractile response to stimulation. The measurement of the electrical response to muscle stimulation is called electromyography. The mechanical response to stimulation of the muscle can be measured by mechanomyography, and acceleromyography[13]

Consensus Statement on Perioperative Use of Neuromuscular Monitoring[]
In 2018 recommendations by an international panel of experts on neuromuscular monitoring to assist anaesthesia care providers and professional organisations that develop practice advisories and guidelines regarding the minimum standards for monitoring patients that receive neuromuscular blockade (NMB) during anaesthesia. The recommendations include the following:
- "Quantitative (objective) NMB monitoring should be used whenever non-depolarising neuromuscular blocking drug is administered."
- "Subjective or clinical tests of NMB are not predictive of adequate neuromuscular recovery and are not sensitive to detect residual weakness; their use should be abandoned in favour of quantitative (objective) monitoring."
- "Professional organisations should develop practice standards and guidelines detailing how best to monitor and manage perioperative administration of NMBDs."
- "Terms that describe the levels of NMB should be standardised. New proposed definitions are published in the consensus statement based on quantitative NMB monitoring criteria."[14]
Anaesthetic organisations with guidelines or professional standards on neuromuscular monitoring[]
The Association of Anaesthetists of Great Britain and Ireland published recommendations for standards of monitoring during anaesthesia and recovery in 2015.[15] These included that a peripheral nerve stimulator is mandatory for all patients receiving neuromuscular blocking drugs and that they should be applied and used from induction (to confirm adequate muscle relaxation before intubation) until recovery from blockade and return of consciousness. They state that a more reliable guarantee of return of safe motor function is a train of four ratio of greater than 0.9. A quantitative neuromuscular monitor is required to accurately assess the train of four ratio.[16]
also publishes professional standards and guidelines on monitoring during anaesthesia. In respect to neuromuscular function monitoring - They state " Neuromuscular function monitoring, preferably quantitative, must be available for every patient in whom neuromuscular blockade is induced and should be used whenever the anaesthetist is considering extubation following the use of non-depolarising neuromuscular blockade."[17]
References[]
- ^ Ortega R, Brull SJ, Prielipp R, Gutierrez A, De La Cruz R, Conley CM (January 2018). "Monitoring Neuromuscular Function". The New England Journal of Medicine. 378 (4): e6. doi:10.1056/NEJMvcm1603741. PMID 29365307.
- ^ Naguib M, Brull SJ, Johnson KB (January 2017). "Conceptual and technical insights into the basis of neuromuscular monitoring". Anaesthesia. 72 Suppl 1 (S1): 16–37. doi:10.1111/anae.13738. PMID 28044330.
- ^ Checketts MR, Alladi R, Ferguson K, Gemmell L, Handy JM, Klein AA, Love NJ, Misra U, Morris C, Nathanson MH, Rodney GE, Verma R, Pandit JJ (January 2016). "Recommendations for standards of monitoring during anaesthesia and recovery 2015: Association of Anaesthetists of Great Britain and Ireland". Anaesthesia. 71 (1): 85–93. doi:10.1111/anae.13316. PMC 5063182. PMID 26582586.
- ^ "Train-of-Four Stimulation". Churchill Livingstone. 2000. Archived from the original on 11 September 2014. Retrieved 10 September 2014.
- ^ Saenz AD, Maillie S, Eiger G (12 July 2013). Spencer DC (ed.). "Peripheral Nerve Stimulator - Train of Four Monitoring". Medscape. Retrieved 10 September 2014.
- ^ Viby-Mogensen J. "Chapter 39: Neuromuscular Monitoring" (PDF). Miller's Anesthesia (5th ed.). Churchill Livingstone, Inc.
- ^ Harvey AM, Masland RL (1941). "Actions of durarizing preparations in the human". Journal of Pharmacology and Experimental Therapeutics. 73 (3): 304–311.
- ^ Botelho SY (November 1955). "Comparison of simultaneously recorded electrical and mechanical activity in myasthenia gravis patients and in partially curarized normal humans". The American Journal of Medicine. 19 (5): 693–6. doi:10.1016/S0002-9343(55)80010-1. PMID 13268466.
- ^ Christie TH, Churchill-Davidson HC (April 1958). "The St. Thomas's Hospital nerve stimulator in the diagnosis of prolonged apnoea". Lancet. 1 (7024): 776. doi:10.1016/s0140-6736(58)91583-6. PMID 13526270.
- ^ Engbaek J, Ostergaard D, Viby-Mogensen J (March 1989). "Double burst stimulation (DBS): a new pattern of nerve stimulation to identify residual neuromuscular block". British Journal of Anaesthesia. 62 (3): 274–8. doi:10.1093/bja/62.3.274. PMID 2522790.
- ^ ALI, HASSAN H.; UTTING, J.E.; GRAY, CECIL (November 1970). "Stimulus Frequency in the Detection of Neuromuscular Block in Humans". British Journal of Anaesthesia. 42 (11): 967–978. doi:10.1093/bja/42.11.967. ISSN 0007-0912. PMID 5488360.
- ^ Ortega, Rafael; Brull, Sorin J.; Prielipp, Richard; Gutierrez, Alexander; de la Cruz, Rossemary; Conley, Christopher M. (2018). "Monitoring Neuromuscular Function | NEJM". New England Journal of Medicine. 378 (4): e6. doi:10.1056/nejmvcm1603741. PMID 29365307.
- ^ Brull, Sorin J.; Kopman, Aaron F. (January 2017). "Current Status of Neuromuscular Reversal and Monitoring". Anesthesiology. 126 (1): 173–190. doi:10.1097/aln.0000000000001409. ISSN 0003-3022. PMID 27820709.
- ^ Naguib, Mohamed; Brull, Sorin J.; Kopman, Aaron F.; Hunter, Jennifer M.; Fülesdi, Béla; Arkes, Hal R.; Elstein, Arthur; Todd, Michael M.; Johnson, Ken B. (July 2018). "Consensus Statement on Perioperative Use of Neuromuscular Monitoring". Anesthesia & Analgesia. 127 (1): 71–80. doi:10.1213/ane.0000000000002670. ISSN 0003-2999. PMID 29200077.
- ^ Checketts, M. R.; Alladi, R.; Ferguson, K.; Gemmell, L.; Handy, J. M.; Klein, A. A.; Love, N. J.; Misra, U.; Morris, C. (2016). "Recommendations for standards of monitoring during anaesthesia and recovery 2015 : Association of Anaesthetists of Great Britain and Ireland". Anaesthesia. 71 (1): 85–93. doi:10.1111/anae.13316. ISSN 1365-2044. PMC 5063182. PMID 26582586.
- ^ Hemmerling, Thomas M.; Le, Nhien (January 2007). "Brief review: Neuromuscular monitoring: an update for the clinician". Canadian Journal of Anesthesia. 54 (1): 58–72. doi:10.1007/bf03021901. ISSN 0832-610X. PMID 17197470.
- ^ "Australian and New Zealand College of AnaesthetistsProfessional Standards 2017 PS18 Guidelines on monitoring during anaesthesia" (PDF).
Further reading[]
- Hemmerling TM, Le N (January 2007). "Brief review: Neuromuscular monitoring: an update for the clinician". Canadian Journal of Anesthesia. 54 (1): 58–72. doi:10.1007/BF03021901. PMID 17197470. Archived from the original on 2009-04-14.
- Anesthesia
- Medical monitoring