Orbital blowout fracture
| Blowout fracture | |
|---|---|
| Other names | Orbital floor fracture |
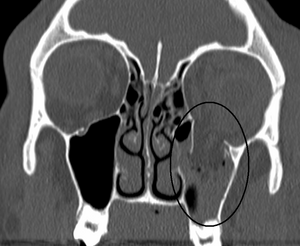 | |
| An orbital blowout fracture of the floor of the left orbit. | |
| Specialty | Oral & Maxillofacial Surgery |
| Symptoms | Double vision especially when looking up, numbness of the lateral nose skin, the cheek below the eyelid, and the upper lip, Bloody nose, lateral subconjunctival hemorrhage (bright red blood over the sclera (white of the eye)) |
| Causes | Direct trauma to the eye socket. |
An orbital blowout fracture is a traumatic deformity of the orbital floor or medial wall, typically resulting from impact of a blunt object larger than the orbital aperture, or eye socket. Most commonly the inferior orbital wall i.e. the floor is likely to collapse, because the bones of the roof and lateral walls are robust. Although the bone forming the medial wall is thinnest, it is buttressed by the bone separating the ethmoidal air cells. The comparatively thin bone of the floor of the orbit and roof of the maxillary sinus has no support and therefore it is the inferior wall that collapses mostly. So the medial wall blowout fractures are second most common, whereas superior wall i.e. the roof and lateral wall blowout fractures are uncommon & rare respectively. There are two broad categories of blowout fractures: open door, which are large, displaced and comminuted, and trapdoor, which are linear, hinged, and minimally displaced. They are characterized by double vision, sunken ocular globes, and loss of sensation of the cheek and upper gums due to infraorbital nerve injury.[1]
In pure orbital blowout fractures, the orbital rim (the most anterior bony margin of the orbit) is preserved, while with impure fractures, the orbital rim is also injured. With the trapdoor variant, there is a high frequency of extra-ocular muscle entrapment, despite minimal signs of external trauma, a phenomenon referred to as a 'white-eyed' orbital blowout fracture.[2] They can occur with other injuries such as transfacial Le Fort fractures or zygomaticomaxillary complex fractures. The most common causes are assault and motor vehicle accidents. In children, the trapdoor subtype are more common.[3]
Surgical intervention may be required to prevent diplopia and enophthalmos. Patients that are not experiencing enophthalmos or diplopia, and that have good extraocular mobility can be closely followed by ophthalmology without surgery.[4]
Signs & Symptoms[]
Some clinically observed signs and symptoms include:[5][6]
- Orbital pain
- Eyes displaced posteriorly into sockets (enophthalmos)
- Limitation of eye movement
- Loss of sensation (hypoesthesia) along the trigeminal (V2) nerve distribution
- Seeing-double when looking up or down (vertical diplopia)
- Orbital and lid subcutaneous emphysema, especially when blowing the nose or sneezing
- Nausea and bradycardia due to oculocardiac reflex inability to elevate eye ball, and move eyeball downward due to inferior rectus entrapment
Causes[]
Common medical causes of blowout fracture may include:[citation needed]
- Direct orbital blunt injury
- Sports injury (squash ball,[7] tennis ball etc.)
- Motor vehicle accidents
Mechanism[]
The force of a blow to the orbit is dissipated by a fracture of the surrounding bone, usually the orbital floor and/or the medial orbital wall. In blowout fractures, the medial wall is fractured indirectly. When an external force is applied to the orbital cavity from an object whose diameter is larger than that of the orbit, the orbital contents are retropulsed and compressed.[8] The consequent sudden rise in intraorbital pressure is transmitted to the walls of the orbit, which ultimately leads to fractures of the thin medial wall and/or orbital floor. Theoretically, this mechanism should lead to more fractures of the medial wall than the floor, since the medial wall is slightly thinner (0.25 mm vs 0.50 mm).[9] However, it is known that pure blowout fractures most frequently involve the orbital floor. This may be attributed to the honeycomb structure of the numerous bony septa of the ethmoid sinuses, which support the lamina papyracea, thus allowing it to withstand the sudden rise in intraorbital hydraulic pressure better than the orbital floor.[10]
In children, the flexibility of the actively developing floor of the orbit fractures in a linear pattern that snaps backward. This is commonly referred to as a trapdoor fracture.[4] The trapdoor can entrap soft-tissue contents, thus causing permanent structural change that requires surgical intervention.[4]
Diagnosis[]
Diagnosis is based on clinical and radiographic evidence. Periorbital bruising and subconjunctival hemorrhage are indirect signs of a possible fracture.[citation needed]
Imaging[]
Thin cut (2-3mm) CT scan with axial and coronal view is the optimal study of choice for orbital fractures.[8][11]
Plain radiographs, on the other hand, do not have the sensitively capture blowout fractures.[12] On Water's view radiograph, polypoid mass can be observed hanging from the floor into the maxillary antrum, classically known as teardrop sign, as it usually is in shape of a teardrop. This polypoid mass consists of herniated orbital contents, periorbital fat and inferior rectus muscle. The affected sinus is partially opacified on radiograph. Air-fluid level in maxillary sinus may sometimes be seen due to presence of blood. Lucency in orbits (on a radiograph) usually indicate orbital emphysema.[citation needed]
Treatment[]
Initial management[]
All patients should follow-up with an ophthalmologist within 1 week of the fracture. To prevent orbital emphysema, patients are advised to avoid blowing of the nose.[8] Nasal decongestants are commonly used. It is also common practice to administer prophylactic antibiotics when the fracture enters a sinus, although this practice is largely anecdotal.[5][13] Amoxicillin-clavulanate and azithromycin are most commonly used.[5] Oral corticosteroids are used to decrease swelling.[14]
Surgery[]
Surgery is indicated if there is enophthalmos greater than 2 mm on imaging, Double vision on primary or inferior gaze, entrapment of extraocular muscles, or the fracture involves greater than 50% of the orbital floor.[5] When not surgically repaired, most blowout fractures heal spontaneously without significant consequence.[citation needed]
Surgical repair of a "blowout" is rarely undertaken immediately; it can be safely postponed for up to two weeks, if necessary, to let the swelling subside. Surgery to treat the fracture generally leaves little or no scarring and the recovery period is usually brief. Ideally, the surgery will provide a permanent cure, but sometimes it provides only partial relief from double vision or a sunken eye.[15] Reconstruction is usually performed with a titanium mesh or porous polyethylene through a transconjunctival or subciliary incision. More recently, there has been success with endoscopic, or minimally invasive, approaches.[16]
Epidemiology[]
Orbital fractures, in general, are more prevalent in men than women. In one study in children, 81% of cases were boys (mean age 12.5 years).[17] In another study in adults, men accounted for 72% of orbital fractures (mean age 81).[18]
History[]
Orbital floor fractures were investigated and described by MacKenzie in Paris in 1844[19] and the term blow out fracture was coined in 1957 by Smith & Regan,[20] who were investigating injuries to the orbit and resultant inferior rectus entrapment, by placing a hurling ball on cadaverous orbits and striking it with a mallet.
References[]
- ^ Caranci, F; Cicala, D; Cappabianca, S; Briganti, F; Brunese, L; Fonio, P (2012). "Orbital fractures: Role of imaging". Seminars in Ultrasound, CT and MRI. 33 (5): 385–91. doi:10.1053/j.sult.2012.06.007. PMID 22964404.
- ^ Caranci, F; Cicala, D; Cappabianca, S; Briganti, F; Brunese, L; Fonio, P (2012). "Orbital fractures: Role of imaging". Seminars in Ultrasound, CT and MRI. 33 (5): 385–91. doi:10.1053/j.sult.2012.06.007. PMID 22964404.
- ^ Ellis e, 3rd (2012). "Orbital trauma". Oral and Maxillofacial Surgery Clinics of North America. 24 (4): 629–48. doi:10.1016/j.coms.2012.07.006. PMID 22981078.
- ^ a b c W., Flint, Paul; 1935-, Cummings, Charles W. (Charles William) (2010-01-01). Otolaryngology head and neck surgery. Mosby. ISBN 9780323052832. OCLC 664324957.CS1 maint: numeric names: authors list (link)
- ^ a b c d Jatla, Kalpana K; Enzenauer, Robert W (2004). "Orbital fractures: a review of current literature". Current Surgery. 61 (1): 25–29. doi:10.1016/j.cursur.2003.08.003. PMID 14972167.
- ^ J., Friedman, Neil; II, Pineda, Roberto; Infirmary., Massachusetts Eye and Ear (2014). The Massachusetts eye and ear infirmary illustrated manual of ophthalmology. ISBN 9781455776443. OCLC 944088986.
- ^ Nickson, Chris (July 26, 2014) [August 8, 2010]. "Blown Out, aka Ophthalmology Befuddler 014". Life in the Fast Lane. Retrieved December 29, 2016.
- ^ a b c Joseph, Jeffrey; Glavas, Ioannis P. (2011-01-12). "Orbital fractures: a review". Clinical Ophthalmology. 5: 95–100. doi:10.2147/opth.s14972. PMC 3037036. PMID 21339801.
- ^ Phan, Laura T., W. Jordan Piluek, and Timothy J. McCulley. "Orbital trapdoor fractures." Saudi Journal of Ophthalmology (2012).
- ^ O-Lee, T. J., and Peter J. Koltai. "Pediatric Facial Fractures." Pediatric Otolaryngology for the Clinician (2009): 91-95.
- ^ Ng, P.; Chu, C.; Young, N.; Soo, M. (1996-08-01). "Imaging of orbital floor fractures". Australasian Radiology. 40 (3): 264–268. doi:10.1111/j.1440-1673.1996.tb00400.x. ISSN 0004-8461. PMID 8826732.
- ^ Brady, S. M.; McMann, M. A.; Mazzoli, R. A.; Bushley, D. M.; Ainbinder, D. J.; Carroll, R. B. (2001-03-01). "The diagnosis and management of orbital blowout fractures: update 2001". The American Journal of Emergency Medicine. 19 (2): 147–154. doi:10.1053/ajem.2001.21315. ISSN 0735-6757. PMID 11239261.
- ^ Martin, Bruce; Ghosh, Angaj (2003-01-01). "Antibiotics in orbital floor fractures". Emergency Medicine Journal. 20 (1): 66. doi:10.1136/emj.20.1.66-a. ISSN 1472-0205. PMC 1726033. PMID 12533379.
- ^ Courtney, D. J.; Thomas, S.; Whitfield, P. H. (2000-10-01). "Isolated orbital blowout fractures: survey and review". The British Journal of Oral & Maxillofacial Surgery. 38 (5): 496–504. doi:10.1054/bjom.2000.0500. ISSN 0266-4356. PMID 11010781.
- ^ Mwanza, J. C. K., D. K. Ngoy, and D. L. Kayembe. "Reconstruction of orbital floor blow-out fractures with silicone implant." Bulletin de la Société belge d'ophtalmologie 280 (2001): 57–62.
- ^ Wilde, F; Lorenz, K; Ebner, A. K.; Krauss, O; Mascha, F; Schramm, A (2013). "Intraoperative imaging with a 3D C-arm system after zygomatico-orbital complex fracture reduction". Journal of Oral and Maxillofacial Surgery. 71 (5): 894–910. doi:10.1016/j.joms.2012.10.031. PMID 23352428.
- ^ Hatton, M. P.; Watkins, L. M.; Rubin, P. A. (2001-05-01). "Orbital fractures in children". Ophthalmic Plastic and Reconstructive Surgery. 17 (3): 174–179. doi:10.1097/00002341-200105000-00005. ISSN 0740-9303. PMID 11388382. S2CID 13653675.
- ^ Manolidis, S.; Weeks, B. H.; Kirby, M.; Scarlett, M.; Hollier, L. (2002-11-01). "Classification and surgical management of orbital fractures: experience with 111 orbital reconstructions". The Journal of Craniofacial Surgery. 13 (6): 726–737, discussion 738. doi:10.1097/00001665-200211000-00002. ISSN 1049-2275. PMID 12457084. S2CID 43630551.
- ^ Ng P, Chu C, Young N, Soo M (Aug 1996). "Imaging of orbital floor fractures". Australasian Radiology. 40 (3): 264–268. doi:10.1111/j.1440-1673.1996.tb00400.x. PMID 8826732.
- ^ "Blowout fracture of the orbit: mechanism and correction of internal orbital fracture. By Byron Smith and William F. Regan, Jr". Adv Ophthalmic Plast Reconstr Surg. 6: 197–205. 1987. PMID 3331936.
External links[]
| Classification |
|---|
- CT Scans of Blowout Fracture from MedPix
- Bone fractures