Ptosis (eyelid)
This article needs additional citations for verification. (October 2008) |
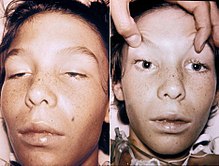
| Ptosis of the eyelids | |
|---|---|
 | |
| Ptosis of the left eyelid (unilateral ptosis). A headshot daguerreotype of an unidentified male, by William Bell in 1852. | |
| Pronunciation |
|
| Specialty | Ophthalmology, neurology |
Ptosis, also known as blepharoptosis,[1] is a drooping or falling of the upper eyelid. The drooping may be worse after being awake longer when the individual's muscles are tired. This condition is sometimes called "Whitaker eye", but that term normally refers to the condition amblyopia. If severe enough and left untreated, the drooping eyelid can cause other conditions, such as amblyopia or astigmatism. This is why it is especially important for this disorder to be treated in children at a young age, before it can interfere with vision development.
The term is from Greek πτῶσις – "a fall, falling".
Signs and symptoms[]
Signs and symptoms typically seen in this condition include:[2]
- The eyelid(s) may appear to droop.
- Droopy eyelids can give the appearance of fatigue.
- The eyelid may not protect the eye as effectively, allowing it to dry out.
- Sagging upper eyelids can partially block the person's field of view.
- Obstructed vision may cause a person to tilt their head back to speak.
- The areas around the eyes may become tired and achy.
- Eyebrows may be constantly lifted to see properly.
Some of the risk factors for ptosis include:
- Eye tumor.
- Diabetes.
- History of stroke.
- Cancer.
- Neurological disorder.
- Age. Eye muscles weaken as they age, increasing the chance of the eyelids drooping.
Causes[]

Ptosis occurs due to dysfunction of the muscles that raise the eyelid or their nerve supply (oculomotor nerve for levator palpebrae superioris and sympathetic nerves for superior tarsal muscle). It can affect one eye or both eyes and is more common in the elderly, as muscles in the eyelids may begin to deteriorate. One can, however, be born with ptosis. This is due to improper development of the infant's levator muscle while still in the mother's womb. Congenital ptosis is hereditary in three main forms.[3] Causes of congenital ptosis remain unknown. Ptosis may be caused by damage to the muscle which raises the eyelid, damage to the superior cervical sympathetic ganglion or damage to the nerve (3rd cranial nerve (oculomotor nerve)) which controls this muscle. Such damage could be a sign or symptom of an underlying disease such as diabetes mellitus, a brain tumor, a pancoast tumor (apex of lung) and diseases which may cause weakness in muscles or nerve damage, such as myasthenia gravis or oculopharyngeal muscular dystrophy. Exposure to the toxins in some snake venoms, such as that of the black mamba, may also cause this effect.
Ptosis can be caused by the aponeurosis of the levator muscle, nerve abnormalities, trauma, inflammation or lesions of the lid or orbit.[4] Dysfunctions of the levators may occur as a result of autoimmune antibodies attacking and eliminating the neurotransmitter.[5]
Ptosis may be due to a myogenic, neurogenic, aponeurotic, mechanical or traumatic cause, and it usually occurs isolated, but may be associated with various other conditions, like immunological, degenerative, or hereditary disorders, tumors or infections.[6]
Acquired ptosis is most commonly caused by aponeurotic ptosis. This can occur as a result of senescence, dehiscence or disinsertion of the levator aponeurosis. Moreover, chronic inflammation or intraocular surgery can lead to the same effect. Also, wearing contact lenses for long periods of time is thought to have a certain impact on the development of this condition.
Congenital neurogenic ptosis is believed to be caused by Horner's syndrome.[4] In this case, a mild ptosis may be associated with ipsilateral ptosis, iris and areola hypopigmentation and anhidrosis due to paresis of the superior tarsal muscle. Acquired Horner syndrome may result after trauma, neoplastic insult, or even vascular disease.
Ptosis due to trauma can ensue after an eyelid laceration with transection of the upper eyelid elevators or disruption of the neural input.[4]
Other causes of ptosis include eyelid neoplasms, neurofibromas or the cicatrization after inflammation or surgery. Mild ptosis may occur with aging. A drooping eyelid can be one of the first signals of a third nerve palsy due to a cerebral aneurysm, that otherwise is asymptomatic and referred to as an oculomotor nerve palsy.
Drugs[]
Use of high doses of opioid drugs such as morphine, oxycodone, heroin, or hydrocodone can cause ptosis.[7] Pregabalin, an anticonvulsant drug, has also been known to cause mild ptosis.[8]
Mechanism and pathophysiology[]
Different trauma can cause and induce many different mechanisms. For example, myogenic ptosis results from a direct injury to the levator muscle and/or Müller's muscle. On the other hand, neurogenic ptosis is caused by closed head injuries, or traumatically-introduced neurotoxin (wasp/bee/snake venom) or botulinum toxin, due to the effect of those factors on the CNIII or the sympathetic pathway. Mechanical ptosis can also occur due to scarring tissue restricting the patient's eyelid excursion or weighing down the patient's lid.[9] Another mechanism is the disturbance of the oculomotor nerve causing the levator palpebrae to weaken, resulting in the eyelid drooping. Ptosis can also occur in a patient with brain tumors due to pressure on the third nerve, also known as the sympathetic nerve, on the brainstem.
Pathology[]
Myasthenia gravis is a common neurogenic ptosis which could be also classified as neuromuscular ptosis because the site of pathology is at the neuromuscular junction. Studies have shown that up to 70% of myasthenia gravis patients present with ptosis, and 90% of these patients will eventually develop ptosis.[10] In this case, ptosis can be unilateral or bilateral and its severity tends to be oscillating during the day, because of factors such as fatigue or drug effect. This particular type of ptosis is distinguished from the others with the help of a Tensilon test and blood tests. Also, specific to myasthenia gravis is the fact that coldness inhibits the activity of cholinesterase, which makes possible differentiating this type of ptosis by applying ice onto the eyelids. Patients with myasthenic ptosis are very likely to still experience a variation of the drooping of the eyelid at different hours of the day.
Ptosis caused by oculomotor palsy can be unilateral or bilateral, as the subnucleus to the levator muscle is a shared, midline structure in the brainstem. In cases in which the palsy is caused by the compression of the nerve by a tumor or aneurysm, it is highly likely to result in an abnormal ipsilateral papillary response and a larger pupil. Surgical third nerve palsy is characterized by a sudden onset of unilateral ptosis and an enlarged or sluggish pupil to the light. In this case, imaging tests such as CTs or MRIs should be considered. Medical third nerve palsy, contrary to surgical third nerve palsy, usually does not affect the pupil and it tends to slowly improve in several weeks. Surgery to correct ptosis due to medical third nerve palsy is normally considered only if the improvement of ptosis and ocular motility are unsatisfactory after half a year. Patients with third nerve palsy tend to have diminished or absent function of the levator.
When caused by Horner's syndrome, ptosis is usually accompanied by miosis and anhidrosis. In this case, the ptosis is due to the result of interruption innervations to the sympathetic, autonomic Muller's muscle rather than the somatic levator palpebrae superioris muscle. The lid position and pupil size are typically affected by this condition and the ptosis is generally mild, no more than 2 mm. The pupil might be smaller on the affected side. While 4% cocaine instilled to the eyes can confirm the diagnosis of Horner's syndrome, Hydroxyamphetamine eye drops can differentiate the location of the lesion.[10]
Chronic progressive external ophthalmoplegia is a systemic condition which usually affects only the lid position and the external eye movement, without involving the movement of the pupil. This condition accounts for nearly 45% of myogenic ptosis cases. Most patients develop ptosis due to this disease in their adulthood. Characteristic to ptosis caused by this condition is the fact that the protective up rolling of the eyeball when the eyelids are closed is very poor.
Diagnosis[]
The doctor will first perform a physical exam with questions about your medical history. This is to distinguish if the condition is hereditary or not. The doctor will then start with a slit lamp exam after you've explained how often your eyelids droop and how long each episode occurs. The slit lamp exam is done with a high-intensity light allowing a closer look at the patient's eyes. The doctor can also perform a Tensilon test. This test involves injecting the drug Tensilon (edrophonium) into a vein. The doctor then monitors the eyelids for signs of improvements from the drug.
Another comprehensive eye exam for proper diagnosis is a visual field test. A visual field test assesses how much the ptosis affects the superior vision. Since nerve damage is one of the causes for ptosis the ophthalmologist will check the patient's pupil for abnormalities. Along with checking the patient's pupil, the doctor will also check the patient's muscle function by having the patient look around.
The ophthalmologist may also measure the degree of the eyelid droop by measuring the marginal reflex distance. The marginal reflex distance is the distance between the center of the pupil and the edge of the upper lid. Along with the marginal reflex distance, the ophthalmologist may examine the strength/ function of the patient's levator muscle. The ophthalmologist will do this test by holding the frontalis muscle (located in the forehead). While holding the forehead, the ophthalmologist will measure how far the eyelid travels when the patient is gazing down.
Through these tests, the ophthalmologist will diagnose if the patient has ptosis and what type of ptosis. After diagnosing the types of ptosis the ophthalmologist will then decide if the patient is a good candidate for surgery.[11]
Classification[]

Depending upon the cause it can be classified into:
- Neurogenic ptosis which includes oculomotor nerve palsy, Horner's syndrome, Marcus Gunn jaw winking syndrome, third cranial nerve misdirection.
- Myogenic ptosis which includes oculopharyngeal muscular dystrophy, myasthenia gravis, myotonic dystrophy, ocular myopathy, simple congenital ptosis, blepharophimosis syndrome.
- Aponeurotic ptosis which may be involutional or post-operative.
- Mechanical ptosis which occurs due to edema or tumors of the upper lid.
- Neurotoxic ptosis which is a classic symptom of envenomation[12] by elapid snakes such as cobras,[13] kraits,[14] mambas and taipans. Bilateral ptosis is usually accompanied by diplopia, dysphagia and/or progressive muscular paralysis. Regardless, neurotoxic ptosis is a precursor to respiratory failure and eventual suffocation caused by complete paralysis of the thoracic diaphragm. It is therefore a medical emergency and immediate treatment is required. Similarly, ptosis may occur in victims of botulism (caused by botulinum toxin) and this is also regarded as a life-threatening symptom.
- Pseudo-ptosis due to:
- Lack of lid support: empty socket or atrophic globe.
- Higher lid position on the other side: as in lid retraction.

Treatment[]
Aponeurotic and congenital ptosis may require surgical correction if severe enough to interfere with the vision or if appearance is a concern. Treatment depends on the type of ptosis, and is usually performed by an ophthalmic plastic surgeon or a reconstructive surgeon who specializes in diseases and problems of the eyelid.
If the condition occurs in a child, then the doctor will delay the surgery until the patient is 4 or 5 years old. If the patient is under the recommended age for surgery, then the doctor will test if occlusion therapy can compensate for the patient's impeded vision. The reason for delaying the surgery until the patient is at least 4–5 years of age is due to the delay for the frontonasal and upper face to complete their complex growth. After this complex growth is complete, the doctors will be able to obtain a more accurate measurement of the conditions. However, if the patient's vision impediment worsens or proves unresponsive to the occlusion therapy, then surgery will be needed sooner.[15]
Surgical procedures include:
- Levator resection
- Müller muscle resection
- Frontalis sling operation (preferred option for oculopharyngeal muscular dystrophy)
- Whitnall sling
The frontalis sling surgery can only be done if the patient's ptosis condition is due to diseased or stretched-out muscles. The stretching-out of muscle is due to age. The frontalis sling surgery is done to either tighten or shorten the affected muscles, thereby allowing the process to raise the patient's lid's resting position. The procedure is done with the doctor using the sling to loop the material, then threading it underneath the patient's eyebrows and above the lashes.[16] Once the sling has been tightened, this allows the patient's forehead's muscle to aid in lifting the lid. The sling can be looped in a pentagon shape, triangle (singular or double) shape. Many different types of slings in the market today include monofilament nylon, silicone rods, polyester, silk, collagen, stainless steel or polypropylene.[15]
Frontalis sling surgery is considered the most effective surgical treatment for moderate to severe congenital ptosis.[17] Many different materials can be used for the surgery, though it is currently unclear which material has the highest success rate.
The Levator Resection and Advancement surgery should only be considered for patients who are experiencing a levator function less than or equal to 5 mm.[15] The levator function is a measurement of the distance that the eyelid travels starting with the downgaze moving to the upgaze without moving the frontalis muscle.[18] Although this procedure can be completed through two different approaches, the internal and the external, the external approach allows the surgeons to obtain a better view of the surgical site during the procedure. The surgeon will begin with an incision on the eyelid. Once the levator has been exposed, the surgeon either fold it or cut it off before suturing it to the tarsal plate. During this procedure, it is up to the surgeon to decide the height and the contour of the patient's eyelid, with input from the patient.
The Whitnall sling procedure is done with an incision from the levator to the Whitnall ligament. Then the surgeon will suture the Whitnall's ligament connecting it to the superior tarsal edge. This procedure most likely is done if the patients are concerned about cosmetic appearance. The Whitnall sling procedure is able to provide a better cosmetic result because the procedure is able to keep the Whitnall's ligament intact. This allows the support of the lacrimal gland and temporal eyelid to be maintained.[19]
Despite the gains that the patient can obtain from the surgeries, there are risk factors. After the surgery, the patient may experience asymmetrical (uneven) eyelids. If the surgery was not done carefully, the patient may experience dry eyes due to the eye no longer fully closing. The patient may also experience bleeding after the surgery and infections, if the surgical site is not taken care of properly.[20] On rare occasions, the patient will experience a loss in eyelid movement.[21]
Non-surgical modalities like the use of "crutch" glasses or ptosis crutches or special scleral contact lenses to support the eyelid may also be used.
Ptosis that is caused by a disease may improve if the disease is treated successfully, although some related diseases, such as oculopharyngeal muscular dystrophy, currently have no cures.
Prognosis[]
If the ptosis is left untreated, then patients may experience amblyopia, also known as lazy eye, which can permanently damage the patient's vision.[20] After careful observation and planning from specialists, ptosis can be successfully treated. Treatment like surgery will allow the patient to begin experiencing improvement in vision as well as cosmetic results. Among all the patients who were previously treated with ptosis, half required additional surgery within 8 to 10 years of the first surgery. If the ptosis is not related to major health issues (such as cancerous tumours or traumatic injuries), then the condition will not shorten the patient's life expectancy.[22]
Epidemiology[]
According to ophthalmology studies done on ptosis patients, occurrence rates are as follows. The average age for females experiencing aponeurotic ptosis is 67.83 years and the corresponding male average age is 68.19. The average age for congenital ptosis is 12.27 years for females and 8.57 years for males. The average age for mechanical ptosis is 49.41 years in females and 43.30 years in males. The average age for myogenic ptosis is 53.45 for females and 43.30 for males. The average age for neurogenic ptosis is 43.6 years in females and 32.62 years in males. Lastly, the average age for traumatic ptosis is 35.12 years in females and 33.4 years in males.[23] Ptosis was not found to have any overall gender or racial preference.[24]
Research directions[]
Current studies have indicated that previous methods such as occlusion therapy and surgery are considered to be the most appropriate for treating this condition. Further studies are encouraged to be able to determine the optimal surgical indications. Any discoveries on approaches with dry eye will help further the oculoplastic surgeries.[25]
Etymology[]
Ptosis is derived from the Greek word πτῶσις ("fall"), and is defined as the "abnormal lowering or prolapse of an organ or body part".
See also[]
References[]
- ^ Mark W. Leitman. "External structures". Manual for Eye Examination (9 ed.). Wiley Blackwell. p. 61.
- ^ "Ptosis Of The Eyelid: Symptoms, Causes, Treatments". www.eyeinstitute.co.nz. Retrieved 2019-12-09.
- ^ "Congenital Ptosis". MEDgle. Archived from the original on 2016-01-05. Retrieved 2008-10-20.
- ^ Jump up to: a b c Adult Ptosis at eMedicine
- ^ "Eye Ptosis Congenital". Retrieved 2010-06-14.
- ^ Finsterer, J (2003). "Ptosis: causes, presentation, and management". Aesthetic Plastic Surgery. 27 (3): 193–204. doi:10.1007/s00266-003-0127-5. PMID 12925861. S2CID 12774266.
- ^ Iqbal N (2002). "Ptosis, convergence disorder and heroin" (PDF). Annals of Saudi Medicine. 22 (5–6): 369–71. doi:10.5144/0256-4947.2002.369. PMID 17146268.
- ^ "Lyrica (Pregabalin) – Reports of Side Effects & Adverse Reactions". DrugLib.com. Retrieved 2010-07-12.
- ^ Jacobs, Sarah Mireles; Tyring, Ariel J.; Amadi, Arash J. (2018). "Traumatic Ptosis: Evaluation of Etiology, Management and Prognosis". Journal of Ophthalmic & Vision Research. 13 (4): 447–452. doi:10.4103/jovr.jovr_148_17. ISSN 2008-2010. PMC 6210876. PMID 30479715.
- ^ Jump up to: a b "Ptosis" (PDF). Retrieved 2010-06-14.
- ^ "Diagnosing Ptosis". nyulangone.org. Retrieved 2019-12-09.
- ^ Warrell, D. A.; Hudson, B. J.; Lalloo, D. G.; Trevett, A. J.; Whitehead, P; Bamler, P. R.; Ranaivoson, M; Wiyono, A; Richie, T. L.; Fryauff, D. J.; O'Shea, M. T.; Richards, A. M.; Theakston, R. D. (1996). "The emerging syndrome of envenoming by the New Guinea small-eyed snake Micropechis ikaheka". QJM : Monthly Journal of the Association of Physicians. 89 (7): 523–30. doi:10.1093/qjmed/89.7.523. PMID 8759493.
- ^ "Nature's poisons". Science Museum (London). Archived from the original on 2008-12-30. Retrieved 2008-10-21.
- ^ "Management of Snake bites in South East Asia – Part 2". World Health Organization. Archived from the original on 2012-04-07. Retrieved 2008-10-12.
- ^ Jump up to: a b c City, Janice Liao, MD, New York. "Ptosis: Diagnostic Tips & Surgical Options". www.reviewofophthalmology.com. Retrieved 2019-12-09.
- ^ "What is Frontalis Sling? What are the advantages and disadvantages?". American Academy of Ophthalmology. 2012-04-12. Retrieved 2019-12-09.
- ^ Rosenberg JB, Andersen J, Barmettler A (2019). "Types of materials for frontalis sling surgery for congenital ptosis". Cochrane Database Syst Rev. 2019 (4): CD012725. doi:10.1002/14651858.CD012725.pub2. PMC 6478334. PMID 31013353.CS1 maint: multiple names: authors list (link)
- ^ "Blepharoptosis - EyeWiki". eyewiki.aao.org. Retrieved 2019-12-09.
- ^ "Treatment Controversies, Congenital Ptosis. EyeRounds.org - Ophthalmology - The University of Iowa". webeye.ophth.uiowa.edu. Retrieved 2019-12-09.
- ^ Jump up to: a b "Ptosis Information and Symptoms -". 2020aec.com. Retrieved 2019-12-09.
- ^ "What To Do If You Have Drooping Eyelids (Ptosis)". All About Vision. Retrieved 2019-12-09.
- ^ "Ptosis, Congenital - EyeWiki". eyewiki.aao.org. Retrieved 2019-12-09.
- ^ Gonzalez-Esnaurrizar, G. (2008-05-14). "The Epidemiology and Etiology of Ptosis in a Ophthalmic Center". Investigative Ophthalmology & Visual Science. 49 (13): 640. ISSN 1552-5783.
- ^ Philadelphia, Jurij R. Bilyk, MD. "How to Spot and Treat Dangerous Ptosis". www.reviewofophthalmology.com. Retrieved 2019-12-08.
- ^ Aakalu, Vinay (2011). "Current Ptosis Management: A National Survey of ASOPRS Member" (PDF). Original Investigation. 0.
Further reading[]
- The AMA Medical Guide, Random House, Inc. New York, 1997 ed.
External links[]
| Classification | |
|---|---|
| External resources |
- Congenital disorders of eyes
- Disorders of eyelid, lacrimal system and orbit
