Subcutaneous T-cell lymphoma
| Subcutaneous T-cell lymphoma | |
|---|---|
| Specialty | Oncology, cutaneous oncology |
| Complications | HPS (hemophagocytic syndrome) |
| Diagnostic method | Requires biopsy confirmation by expert hemopathologist |
| Differential diagnosis | Lupus panniculitis, cutaneous gamma delta T Cell lymphoma |
Subcutaneous T-cell lymphoma (also known as a "panniculitis-like T-cell lymphoma") is a cutaneous condition that most commonly presents in young adults, and is characterized by subcutaneous nodules.[1]: 739 Common symptoms include fever, fatigue, and pancytopenia.
Cause[]
This section is empty. You can help by . (June 2017) |
Diagnosis[]
Classification[]
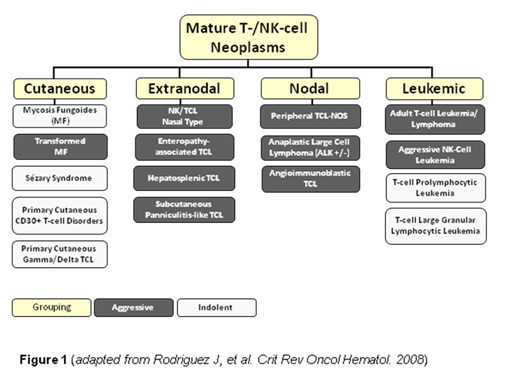
Subcutaneous panniculitis-like T-cell lymphoma, is a subtype of Peripheral T-cell lymphoma. Peripheral T-cell lymphoma (PTCL) is defined as a diverse group of aggressive lymphomas that develop from mature-stage white blood cells called T-cells and natural killer cells (NK cells) (see figure for an overview of PTCL subtypes). PTCL is a type of non-Hodgkin’s lymphoma (NHL).[2] NHL affects two particular types of white blood cells: B-cells and T-cells. PTCL specifically affects T-cells, and results when T-cells develop and grow abnormally.
Subcutaneous Panniculitis-like T-cell Lymphoma is a rare type of lymphoma that infiltrates the subcutaneous fat but does not involve the skin. There are two subtypes – alpha-beta and gamma-delta. Patients with the gamma-delta subtype have a more aggressive clinical course.[3]
It is described as CD3+/CD4-/CD8+, with CD30 and CD56 usually negative.[4]
Treatment[]
Historically, Subcutaneous Panniculitis-like T-cell Lymphoma, as with other types of T-cell lymphoma, was treated similarly to B-cell lymphomas. However, in recent years, scientists have developed techniques to better recognize the different types of lymphomas, such as PTCL. It is now understood that PTCL behaves differently from B-cell lymphomas and therapies are being developed that specifically target these types of lymphoma. Currently, however, there are no drugs approved by the U.S. Food and Drug Administration (FDA) specifically for PTCL. There are two drugs, Pralatrexate and Romidepsin, which are both approved by the FDA for relapsed or refractory T cell lymphoma. Anthracycline-containing chemotherapy regimens are commonly offered as the initial therapy. Some patients may receive an autologous or allogeneic stem cell transplant.[5][6][7][8][9][10][11][12] Novel approaches to the treatment of PTCL in the relapsed or refractory setting are under investigation.
CHOP or CHOP-like regimens have been used.[13]
Research[]
Pralatrexate is one compound currently under investigation to add to the frontline treatment of PTCL. It is currently approved by the FDA for relapsed or refractory T cell lymphoma. Side effects include mouth sores, which can be severe.[citation needed]
See also[]
- Cutaneous T-cell lymphoma
- Lennert lymphoma
- Skin lesion
References[]
- ^ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 978-0-7216-2921-6.
- ^ Swerdlow SH, WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues, 2008
- ^ Vose JM (October 2008). "Peripheral T-cell non-Hodgkin's lymphoma". Hematol. Oncol. Clin. North Am. 22 (5): 997–1005, x. doi:10.1016/j.hoc.2008.07.010. PMID 18954748.
- ^ Kong, YY.; Dai, B.; Kong, JC.; Zhou, XY.; Lu, HF.; Shen, L.; Du, X.; Shi, DR. (Oct 2008). "Subcutaneous panniculitis-like T-cell lymphoma: a clinicopathologic, immunophenotypic, and molecular study of 22 Asian cases according to WHO-EORTC classification". Am J Surg Pathol. 32 (10): 1495–502. doi:10.1097/PAS.0b013e31817a9081. PMID 18708940.
- ^ Reimer P, Rüdiger T, Geissinger E, et al. (January 2009). "Autologous stem-cell transplantation as first-line therapy in peripheral T-cell lymphomas: results of a prospective multicenter study". J. Clin. Oncol. 27 (1): 106–13. doi:10.1200/JCO.2008.17.4870. PMID 19029417.
- ^ Mercadal S, Briones J, Xicoy B, et al. (May 2008). "Intensive chemotherapy (high-dose CHOP/ESHAP regimen) followed by autologous stem-cell transplantation in previously untreated patients with peripheral T-cell lymphoma". Ann. Oncol. 19 (5): 958–63. doi:10.1093/annonc/mdn022. PMID 18303032.
- ^ Rodríguez J, Conde E, Gutiérrez A, et al. (July 2007). "Frontline autologous stem cell transplantation in high-risk peripheral T-cell lymphoma: a prospective study from The Gel-Tamo Study Group". Eur. J. Haematol. 79 (1): 32–8. doi:10.1111/j.1600-0609.2007.00856.x. PMID 17598836.
- ^ Corradini P, Tarella C, Zallio F, et al. (September 2006). "Long-term follow-up of patients with peripheral T-cell lymphomas treated up-front with high-dose chemotherapy followed by autologous stem cell transplantation". Leukemia. 20 (9): 1533–8. doi:10.1038/sj.leu.2404306. PMID 16871285.
- ^ d’Amore F, et al. Blood. 2006;108:A401
- ^ Gisselbrecht C, Lepage E, Molina T, et al. (May 2002). "Shortened first-line high-dose chemotherapy for patients with poor-prognosis aggressive lymphoma". J. Clin. Oncol. 20 (10): 2472–9. doi:10.1200/JCO.2002.02.125. PMID 12011124.
- ^ Deconinck E, Lamy T, Foussard C, et al. (June 2000). "Autologous stem cell transplantation for anaplastic large-cell lymphomas: results of a prospective trial". Br. J. Haematol. 109 (4): 736–42. doi:10.1046/j.1365-2141.2000.02098.x. PMID 10929023.
- ^ Haioun C, Lepage E, Gisselbrecht C, et al. (August 2000). "Survival benefit of high-dose therapy in poor-risk aggressive non-Hodgkin's lymphoma: final analysis of the prospective LNH87-2 protocol—a groupe d'Etude des lymphomes de l'Adulte study". J. Clin. Oncol. 18 (16): 3025–30. doi:10.1200/JCO.2000.18.16.3025. PMID 10944137.
- ^ Rojnuckarin, P.; Nakorn, TN.; Assanasen, T.; Wannakrairot, P.; Intragumtornchai, T. (Mar 2007). "Cyclosporin in subcutaneous panniculitis-like T-cell lymphoma". Leuk Lymphoma. 48 (3): 560–3. doi:10.1080/10428190601078456. PMID 17454599.
External links[]
| Classification | |
|---|---|
| External resources |
- Lymphoid-related cutaneous conditions
