Transcranial magnetic stimulation
| Transcranial magnetic stimulation | |
|---|---|
 Transcranial magnetic stimulation (schematic diagram) | |
| Specialty | Psychiatry, neurology |
| MeSH | D050781 |
Transcranial magnetic stimulation (TMS) is a noninvasive form of brain stimulation in which a changing magnetic field is used to cause electric current at a specific area of the brain through electromagnetic induction. An electric pulse generator, or stimulator, is connected to a magnetic coil, which in turn is connected to the scalp. The stimulator generates a changing electric current within the coil which induces a magnetic field; this field then causes a second inductance of inverted electric charge within the brain itself.[1]: 3 [2]
TMS has shown diagnostic and therapeutic potential in the central nervous system with a wide variety of disease states in neurology and mental health, with research still evolving.[3][4][5][6][7][8][9][10]
Adverse effects of TMS are rare, and include fainting and seizure.[11] Other potential issues include discomfort, pain, hypomania, cognitive change, hearing loss, and inadvertent current induction in implanted devices such as pacemakers or defibrillators.[11]
Medical uses[]

TMS is non-invasive, and does not require surgery or electrode implantation. Its use can be divided into diagnostic and therapeutic applications. Effects vary based on frequency and intensity of the magnetic pulses as well as the length of the train, which affects the total number of pulses given. [13] TMS treatments are now approved by the FDA in the USA and by NICE in the UK for the treatment of depression and are predominantly provided by private clinics. It is the most preferred non-invasive transcranial stimulation technique as it stimulates cortical tissue without the pain sensations as produced in transcranial electrical stimulation. [14]
Diagnosis[]
TMS can be used clinically to measure activity and function of specific brain circuits in humans, most commonly with single or paired magnetic pulses.[3] The most widely accepted use is in measuring the connection between the primary motor cortex of the central nervous system and the peripheral nervous system to evaluate damage related to past or progressive neurologic insult.[3][15][16][17]
Treatment[]
Repetitive high frequency TMS (rTMS) has shown diagnostic and therapeutic potential with the central nervous system in a variety of disease states, particularly in the fields of neurology and mental health.[3][4][5][7][8][9][10]
Adverse effects[]
Although TMS is generally regarded as safe, risks are increased for therapeutic rTMS compared to single or paired diagnostic TMS.[18] Adverse effects generally increase with higher frequency stimulation.[11]
The greatest immediate risk from TMS is fainting, though this is uncommon. Seizures have been reported, but are rare.[11][19][20] Other adverse effects include short term discomfort, pain, brief episodes of hypomania, cognitive change, hearing loss, impaired working memory, and the induction of electrical currents in implanted devices such as cardiac pacemakers.[11]
Procedure[]
During the procedure, a magnetic coil is positioned at the head of the person receiving the treatment using anatomical landmarks on the skull, in particular the inion and nasion.[12] The coil is then connected to a pulse generator, or stimulator, that delivers electric current to the coil.[2]
Physics[]
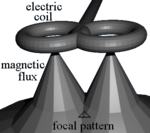

TMS uses electromagnetic induction to generate an electric current across the scalp and skull.[21][22] A plastic-enclosed coil of wire is held next to the skull and when activated, produces a magnetic field oriented orthogonal to the plane of the coil. The magnetic field can then be directed to induce an inverted electric current in the brain that activates nearby nerve cells in a manner similar to a current applied superficially at the cortical surface.[23]
The magnetic field is about the same strength as an MRI, and the pulse generally reaches no more than 5 centimeters into the brain, unless using a modified coil and technique for deeper stimulation.[22]
From the Biot–Savart law,
it has been shown that a current through a wire generates a magnetic field around that wire. Transcranial magnetic stimulation is achieved by quickly discharging current from a large capacitor into a coil to produce pulsed magnetic fields between 2 and 3 Tesla in strength.[24] Directing the magnetic field pulse at a targeted area in the brain causes a localized electrical current which can then either depolarize or hyperpolarize neurons at that site. The magnetic flux generated by the current causes its own electric field, as explained by the Maxwell-Faraday equation,
This electric field causes a change in transmembrane currents resulting in depolarization or hyperpolarization of neurons, causing them to be more or less excitable, respectively.[24]
Deep TMS can reach up to 6 cm into the brain to stimulate deeper layers of the motor cortex, such as that which controls leg motion. The path of this current can be difficult to model because the brain is irregularly shaped with variable internal density and water content, leading to a nonuniform magnetic field strength and conduction throughout its tissues.[25]
Frequency and duration[]
The effects of TMS can be divided based on frequency, duration and intensity (amplitude) of stimulation:[26]
- Single or paired pulse TMS causes neurons in the neocortex under the site of stimulation to depolarize and discharge an action potential. If used in the primary motor cortex, it produces muscle activity referred to as a motor evoked potential (MEP) which can be recorded on electromyography. If used on the occipital cortex, 'phosphenes' (flashes of light) might be perceived by the subject. In most other areas of the cortex, there is no conscious effect, but behaviour may be altered (e.g., slower reaction time on a cognitive task), or changes in brain activity may be detected using diagnostic equipment.[27]
- Repetitive TMS produces longer-lasting effects which persist past the period of stimulation. rTMS can increase or decrease the excitability of the corticospinal tract depending on the intensity of stimulation, coil orientation, and frequency. Low frequency rTMS with a stimulus frequency less than 1 Hz is believed to inhibit cortical firing while a stimulus frequency greater than 1 Hz, or high frequency, is believed to provoke it.[28] Though its mechanism is not clear, it has been suggested as being due to a change in synaptic efficacy related to long-term potentiation (LTP) and long-term depression (LTD).[29]
Coil types[]
Most devices use a coil shaped like a figure-eight to deliver a shallow magnetic field that affects more superficial neurons in the brain.[30] Differences in magnetic coil design should be considered when comparing results, with important elements including the type of material, geometry and specific characteristics of the associated magnetic pulse.
The core material may be either a magnetically inert substrate ('air core'), or a solid, ferromagnetically active material ('solid core'). Solid cores result in more efficient transfer of electrical energy to a magnetic field and reduce energy loss to heat, and so can be operated with the higher volume of therapy protocols without interruption due to overheating. Varying the geometric shape of the coil itself can cause variations in focality, shape, and depth of penetration. Differences in coil material and its power supply also affect magnetic pulse width and duration.[31]
A number of different types of coils exist, each of which produce different magnetic fields. The round coil is the original used in TMS. Later, the figure-eight (butterfly) coil was developed to provide a more focal pattern of activation in the brain, and the four-leaf coil for focal stimulation of peripheral nerves. The double-cone coil conforms more to the shape of the head.[32] The Hesed (H-core), circular crown and double cone coils allow more widespread activation and a deeper magnetic penetration. They are supposed to impact deeper areas in the motor cortex and cerebellum controlling the legs and pelvic floor, for example, though the increased depth comes at the cost of a less focused magnetic pulse.[11]
History[]
Luigi Galvani (1737-1798) undertook research on the effects of electricity on the body in the late-eighteenth century and laid the foundations for the field of electrophysiology.[33] In the 1830s Michael Faraday (1791-1867) discovered that an electrical current had a corresponding magnetic field, and that changing one could induce its counterpart.[34]
Work to directly stimulate the human brain with electricity started in the late 1800s, and by the 1930s the Italian physicians Cerletti and Bini had developed electroconvulsive therapy (ECT).[33] ECT became widely used to treat mental illness, and ultimately overused, as it began to be seen as a panacea (medicine). This led to a backlash in the 1970s.[33]
In 1980 Merton and Morton successfully used transcranial electrical stimulation (TES) to stimulate the motor cortex. However, this process was very uncomfortable, and subsequently Anthony T. Barker began to search for an alternative to TES.[35] He began exploring the use of magnetic fields to alter electrical signaling within the brain, and the first stable TMS devices were developed in 1985.[33][34] They were originally intended[by whom?] as diagnostic and research devices, with evaluation of their therapeutic potential being a later development.[33][34] The United States' FDA first approved TMS devices in October 2008.[33]
Research[]
TMS has shown potential with neurologic conditions such as Alzheimer's disease,[4] amyotrophic lateral sclerosis,[4][36] persistent vegetative states,[4] epilepsy,[4][37] stroke related disability,[4][11][16][17][38][39] tinnitus,[4][40] multiple sclerosis,[4] schizophrenia,[4][10] and traumatic brain injury.[41]
With Parkinson's disease, early results suggest that low frequency stimulation may have an effect on medication associated dyskinesia, and that high frequency stimulation improves motor function.[42] The most effective treatment protocols appear to involve high frequency stimulation of the motor cortex, particularly on the dominant side,[43] but with more variable results for treatment of the dorsolateral prefrontal cortex.[44] It is less effective than electroconvulsive therapy for motor symptoms, though both appear to have utility.[45][46][47] Cerebellar stimulation has also shown potential for the treatment of levodopa associated dyskinesia.[48]
In psychiatry, it has shown potential with anxiety disorders, including panic disorder[49] and obsessive-compulsive disorder (OCD).[4] The most promising areas to target for OCD appear to be the orbitofrontal cortex and the supplementary motor area.[50] Older protocols that targeted the prefrontal dorsal cortex were less successful.[51] It has also been studied with autism,[52] substance abuse,[4] addiction,[4][53] and posttraumatic stress disorder (PTSD).[4] For treatment-resistant major depressive disorder, high-frequency (HF) rTMS of the left dorsolateral prefrontal cortex (DLPFC) appears effective and low-frequency (LF) rTMS of the right DLPFC has probable efficacy.[4][5][7][8][9] Research on the efficacy of rTMS in non-treatment-resistant depression is limited.[54]
TMS can also be used to map functional connectivity between the cerebellum and other areas of the brain.[55]
Study blinding[]
Mimicking the physical discomfort of rTMS with placebo to discern its true effect is a challenging issue in research.[4][11][56][57] It is difficult to establish a convincing placebo for TMS during controlled trials in conscious individuals due to the neck pain, headache and twitching in the scalp or upper face associated with the intervention.[4][11] In addition, placebo manipulations can affect brain sugar metabolism and MEPs, which may confound results.[58] This problem is exacerbated when using subjective measures of improvement.[11] Placebo responses in trials of rTMS in major depression are negatively associated with refractoriness to treatment.[59]
A 2011 review found that most studies did not report unblinding. In the minority that did, participants in real and sham rTMS groups were not significantly different in their ability to correctly guess their therapy, though there was a trend for participants in the real group to more often guess correctly.[60]
Animal model limitations[]
TMS research in animal studies is limited due to its early US Food and Drug Administration approval for treatment-resistant depression, limiting development of animal specific magnetic coils.[61]
Treatments for the general public[]
Regulatory approvals[]
Neurosurgery planning[]
obtained United States Federal Food, Drug, and Cosmetic Act§Section 510(k) clearance for the assessment of the primary motor cortex for pre-procedural planning in December 2009[62] and for neurosurgical planning in June 2011.[63]
Depression[]
In 2008, the US Food and Drug Administration authorized the use of rTMS as a treatment for depression that has not improved with other measures.[64][65] A number of deep TMS have received FDA 510k clearance to market for use in adults with treatment resistant major depressive disorders.[66][67][68][69][70] The Royal Australian and New Zealand College of Psychiatrists has endorsed rTMS for treatment resistant major depressive disorder (MDD).[71]
Migraine[]
The use of single-pulse TMS was approved by the FDA for treatment of migraines in December 2013.[72] It is approved as a Class II medical device under the "de novo pathway".[73][74]
Other neurological areas[]
In the European Economic Area, various versions of Deep TMS H-coils have CE marking for Alzheimer's disease,[75] autism,[75] bipolar disorder,[76] epilepsy,[77] chronic pain,[76] major depressive disorder,[76] Parkinson's disease,[43][78] posttraumatic stress disorder (PTSD),[76] schizophrenia (negative symptoms)[76] and to aid smoking cessation.[75] One review found tentative benefit for cognitive enhancement in healthy people.[79]
In August 2018, the US Food and Drug Administration authorized the use of TMS in the treatment of obsessive-compulsive disorder (OCD).[80]
Coverage by health services and insurers[]
United Kingdom[]
The United Kingdom's National Institute for Health and Care Excellence (NICE) issues guidance to the National Health Service (NHS) in England, Wales, Scotland and Northern Ireland (UK). NICE guidance does not cover whether or not the NHS should fund a procedure. Local NHS bodies (primary care trusts and hospital trusts) make decisions about funding after considering the clinical effectiveness of the procedure and whether the procedure represents value for money for the NHS.[81]
NICE evaluated TMS for severe depression (IPG 242) in 2007, and subsequently considered TMS for reassessment in January 2011 but did not change its evaluation.[82] The Institute found that TMS is safe, but there is insufficient evidence for its efficacy.[82]
In January 2014, NICE reported the results of an evaluation of TMS for treating and preventing migraine (IPG 477). NICE found that short-term TMS is safe but there is insufficient evidence to evaluate safety for long-term and frequent uses. It found that evidence on the efficacy of TMS for the treatment of migraine is limited in quantity, that evidence for the prevention of migraine is limited in both quality and quantity.[83]
Subsequently, in 2015, NICE approved the use of TMS for the treatment of depression in the UK and IPG542 replaced IPG242.[84] NICE said "The evidence on repetitive transcranial magnetic stimulation for depression shows no major safety concerns. The evidence on its efficacy in the short-term is adequate, although the clinical response is variable. Repetitive transcranial magnetic stimulation for depression may be used with normal arrangements for clinical governance and audit."
United States: Commercial health insurance[]
In 2013, several commercial health insurance plans in the United States, including Anthem, Health Net, and Blue Cross Blue Shield of Nebraska and of Rhode Island, covered TMS for the treatment of depression for the first time.[85][86][87][88] In contrast, UnitedHealthcare issued a medical policy for TMS in 2013 that stated there is insufficient evidence that the procedure is beneficial for health outcomes in patients with depression. UnitedHealthcare noted that methodological concerns raised about the scientific evidence studying TMS for depression include small sample size, lack of a validated sham comparison in randomized controlled studies, and variable uses of outcome measures.[89] Other commercial insurance plans whose 2013 medical coverage policies stated that the role of TMS in the treatment of depression and other disorders had not been clearly established or remained investigational included Aetna, Cigna and Regence.[90][91][92]
United States: Medicare[]
Policies for Medicare coverage vary among local jurisdictions within the Medicare system,[93] and Medicare coverage for TMS has varied among jurisdictions and with time. For example:
- In early 2012 in New England, Medicare covered TMS for the first time in the United States.[94][95][96][97] However, that jurisdiction later decided to end coverage after October, 2013.[98]
- In August 2012, the jurisdiction covering Arkansas, Louisiana, Mississippi, Colorado, Texas, Oklahoma, and New Mexico determined that there was insufficient evidence to cover the treatment,[99] but the same jurisdiction subsequently determined that Medicare would cover TMS for the treatment of depression after December 2013.[100]
- Subsequently,[when?] some other Medicare jurisdictions added Medicare coverage for depression.[citation needed]
Costs[]
In the US in 2009, a single TMS session for depressive disorders averaged US$350. A full course of treatment could cost between US$6,000 and US$12,000, depending on the number of treatments.[101][28]
Providers[]
Manufacturers of the TMS devices include[when?] Brainsway, Deymed, MagVenture, Mag&More, Magstim, , Neuronetics, Neurosoft, and NeuroStar.[citation needed]
Current[when?] treatment providers in the UK include a few NHS Trusts and a private operator, Smart TMS. In Cyprus FDA approved treatments for depression and OCD are provided by Cyprus rTMS [102] Also, the Cyprus University of Technology uses rTMS in research.[103]
See also[]
- Cortical stimulation mapping
- Cranial electrotherapy stimulation
- Electrical brain stimulation
- Electroconvulsive therapy
- Low field magnetic stimulation
- Non-invasive cerebellar stimulation
- Transcranial alternating current stimulation
- Transcranial direct-current stimulation
- Transcranial random noise stimulation
References[]
- ^ NICE. January 2014 Transcranial magnetic stimulation for treating and preventing migraine
- ^ Jump up to: a b Michael Craig Miller for Harvard Health Publications. July 26, 2012 Magnetic stimulation: a new approach to treating depression?
- ^ Jump up to: a b c d Groppa S, Oliviero A, Eisen A, Quartarone A, Cohen LG, Mall V, et al. (May 2012). "A practical guide to diagnostic transcranial magnetic stimulation: report of an IFCN committee". Clinical Neurophysiology. 123 (5): 858–82. doi:10.1016/j.clinph.2012.01.010. PMC 4890546. PMID 22349304.
- ^ Jump up to: a b c d e f g h i j k l m n o p q Lefaucheur JP, André-Obadia N, Antal A, Ayache SS, Baeken C, Benninger DH, et al. (November 2014). "Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS)". Clinical Neurophysiology. 125 (11): 2150–2206. doi:10.1016/j.clinph.2014.05.021. PMID 25034472. S2CID 206798663.
- ^ Jump up to: a b c George, Mark S.; Post, Robert M. (April 2011). "Daily Left Prefrontal Repetitive Transcranial Magnetic Stimulation for Acute Treatment of Medication-Resistant Depression". American Journal of Psychiatry. 168 (4): 356–364. doi:10.1176/appi.ajp.2010.10060864. PMID 21474597.
- ^ Gaynes, Bradley N.; Lux, Linda J.; Lloyd, Stacey W.; Hansen, Richard A.; Gartlehner, Gerald; Keener, Patricia; Brode, Shannon; Evans, Tammeka Swinson; Jonas, Dan; Crotty, Karen; Viswanathan, Meera; Lohr, Kathleen N. (2011). "Nonpharmacologic Interventions for Treatment-Resistant Depression in Adults". AHRQ Comparative Effectiveness Reviews. Agency for Healthcare Research and Quality. PMID 22091472. Cite journal requires
|journal=(help) - ^ Jump up to: a b c Berlim, Marcelo T; Van den Eynde, Frederique; Jeff Daskalakis, Z (19 November 2012). "Clinically Meaningful Efficacy and Acceptability of Low-Frequency Repetitive Transcranial Magnetic Stimulation (rTMS) for Treating Primary Major Depression: A Meta-Analysis of Randomized, Double-Blind and Sham-Controlled Trials". Neuropsychopharmacology. 38 (4): 543–551. doi:10.1038/npp.2012.237. PMC 3572468. PMID 23249815.
- ^ Jump up to: a b c Perera, Tarique; George, Mark; Grammer, Geoffrey; Janicak, Philip; Pascual-Leone, Alvaro; Wirecki, Theodore (April 27, 2015). TMS Therapy For Major Depressive Disorder: Evidence Review and Treatment Recommendations for Clinical Practice (PDF) (Report).
- ^ Jump up to: a b c Bersani, F.S.; Minichino, A.; Enticott, P.G.; Mazzarini, L.; Khan, N.; Antonacci, G.; Raccah, R.N.; Salviati, M.; Delle Chiaie, R.; Bersani, G.; Fitzgerald, P.B.; Biondi, M. (January 2013). "Deep transcranial magnetic stimulation as a treatment for psychiatric disorders: A comprehensive review". European Psychiatry. 28 (1): 30–39. doi:10.1016/j.eurpsy.2012.02.006. PMID 22559998. S2CID 29053871.
- ^ Jump up to: a b c Dougall N, Maayan N, Soares-Weiser K, McDermott LM, McIntosh A (August 2015). "Transcranial magnetic stimulation (TMS) for schizophrenia" (PDF). The Cochrane Database of Systematic Reviews. 8 (8): CD006081. doi:10.1002/14651858.CD006081.pub2. hdl:1893/22520. PMID 26289586.
- ^ Jump up to: a b c d e f g h i j Rossi; et al. (January 2021). "Safety and recommendations for TMS use in healthy subjects and patient populations, with updates on training, ethical and regulatory issues: Expert Guidelines". Clinical Neurophysiology. 132 (1): 269–306. doi:10.1016/j.clinph.2020.10.003. PMID 33243615. S2CID 225049093.
- ^ Jump up to: a b Nauczyciel C, Hellier P, Morandi X, Blestel S, Drapier D, Ferre JC, et al. (April 2011). "Assessment of standard coil positioning in transcranial magnetic stimulation in depression". Psychiatry Research. 186 (2–3): 232–8. doi:10.1016/j.psychres.2010.06.012. PMID 20692709. S2CID 25100990.
- ^ Klomjai, Wanalee; Katz, Rose; Lackmy-Vallée, Alexandra (2015-09-01). "Basic principles of transcranial magnetic stimulation (TMS) and repetitive TMS (rTMS)". Annals of Physical and Rehabilitation Medicine. 58 (4): 208–213. doi:10.1016/j.rehab.2015.05.005. ISSN 1877-0657. PMID 26319963.
- ^ Moliadze, V., Zhao, Y., Eysel, U. and Funke, K., 2003. Effect of transcranial magnetic stimulation on single‐unit activity in the cat primary visual cortex. The Journal of Physiology, 553(2), pp.665-679.
- ^ Rossini PM, Rossi S (February 2007). "Transcranial magnetic stimulation: diagnostic, therapeutic, and research potential". Neurology. 68 (7): 484–8. doi:10.1212/01.wnl.0000250268.13789.b2. PMID 17296913. S2CID 19629888.
- ^ Jump up to: a b Dimyan MA, Cohen LG (February 2010). "Contribution of transcranial magnetic stimulation to the understanding of functional recovery mechanisms after stroke". Neurorehabilitation and Neural Repair. 24 (2): 125–35. doi:10.1177/1545968309345270. PMC 2945387. PMID 19767591.
- ^ Jump up to: a b Nowak DA, Bösl K, Podubeckà J, Carey JR (2010). "Noninvasive brain stimulation and motor recovery after stroke". Restorative Neurology and Neuroscience. 28 (4): 531–44. doi:10.3233/RNN-2010-0552. PMID 20714076.
- ^ van den Noort M, Lim S, Bosch P (December 2014). "Recognizing the risks of brain stimulation". Science. 346 (6215): 1307. doi:10.1126/science.346.6215.1307-a. PMID 25504707.
- ^ Dobek CE, Blumberger DM, Downar J, Daskalakis ZJ, Vila-Rodriguez F (2015). "Risk of seizures in transcranial magnetic stimulation: a clinical review to inform consent process focused on bupropion". Neuropsychiatric Disease and Treatment. 11: 2975–87. doi:10.2147/NDT.S91126. PMC 4670017. PMID 26664122.
- ^ Fitzgerald PB, Daskalakis ZJ (2013). "7. rTMS-Associated Adverse Events". Repetitive Transcranial Magnetic Stimulation for Depressive Disorders. Berlin Heidelberg: Springer-Verlag. pp. 81–90. doi:10.1007/978-3-642-36467-9. ISBN 978-3-642-36466-2.
- ^ Cavaleri R, Schabrun SM, Chipchase LS (March 2017). "The number of stimuli required to reliably assess corticomotor excitability and primary motor cortical representations using transcranial magnetic stimulation (TMS): a systematic review and meta-analysis". Systematic Reviews. 6 (1): 48. doi:10.1186/s13643-017-0440-8. PMC 5340029. PMID 28264713.
- ^ Jump up to: a b "Brain Stimulation Therapies". NIMH.
- ^ Cacioppo JT, Tassinary LG, Berntson GG, eds. (2007). Handbook of psychophysiology (3rd ed.). New York: Cambridge Univ. Press. p. 121. ISBN 978-0-521-84471-0.
- ^ Jump up to: a b V. Walsh and A. Pascual-Leone, "Transcranial Magnetic Stimulation: A Neurochronometrics of Mind." Cambridge, Massachusetts: MIT Press, 2003.
- ^ (1) Zangen A, Roth Y, Voller B, Hallett M (April 2005). "Transcranial magnetic stimulation of deep brain regions: evidence for efficacy of the H-coil". Clinical Neurophysiology. 116 (4): 775–9. doi:10.1016/j.clinph.2004.11.008. PMID 15792886. S2CID 25101101.
(2) Huang YZ, Sommer M, Thickbroom G, Hamada M, Pascual-Leonne A, Paulus W, et al. (January 2009). "Consensus: New methodologies for brain stimulation". Brain Stimulation. 2 (1): 2–13. doi:10.1016/j.brs.2008.09.007. PMC 5507351. PMID 20633398. - ^ Rubens MT, Zanto TP (March 2012). "Parameterization of transcranial magnetic stimulation". Journal of Neurophysiology. 107 (5): 1257–9. doi:10.1152/jn.00716.2011. PMC 3311692. PMID 22072509.
- ^ Pascual-Leone A, Davey N, Rothwell J, Wassermann EM, Puri BK (2002). Handbook of Transcranial Magnetic Stimulation. London: Edward Arnold. ISBN 978-0-340-72009-7.
- ^ Jump up to: a b Cusin C, Dougherty DD (August 2012). "Somatic therapies for treatment-resistant depression: ECT, TMS, VNS, DBS". Biology of Mood & Anxiety Disorders. 2 (1): 14. doi:10.1186/2045-5380-2-14. PMC 3514332. PMID 22901565.
- ^ Fitzgerald PB, Fountain S, Daskalakis ZJ (December 2006). "A comprehensive review of the effects of rTMS on motor cortical excitability and inhibition". Clinical Neurophysiology. 117 (12): 2584–96. doi:10.1016/j.clinph.2006.06.712. PMID 16890483. S2CID 31458874.
- ^ Bersani FS, Minichino A, Enticott PG, Mazzarini L, Khan N, Antonacci G, et al. (January 2013). "Deep transcranial magnetic stimulation as a treatment for psychiatric disorders: a comprehensive review". European Psychiatry. 28 (1): 30–9. doi:10.1016/j.eurpsy.2012.02.006. PMID 22559998. S2CID 29053871.

- ^ Riehl M (2008). "TMS Stimulator Design". In Wassermann EM, Epstein CM, Ziemann U, Walsh V, Paus T, Lisanby SH (eds.). Oxford Handbook of Transcranial Stimulation. Oxford: Oxford University Press. pp. 13–23, 25–32. ISBN 978-0-19-856892-6.
- ^ Roth BJ, Maccabee PJ, Eberle LP, Amassian VE, Hallett M, Cadwell J, et al. (February 1994). "In vitro evaluation of a 4-leaf coil design for magnetic stimulation of peripheral nerve". Electroencephalography and Clinical Neurophysiology. 93 (1): 68–74. doi:10.1016/0168-5597(94)90093-0. PMID 7511524.
- ^ Jump up to: a b c d e f Horvath JC, Perez JM, Forrow L, Fregni F, Pascual-Leone A (March 2011). "Transcranial magnetic stimulation: a historical evaluation and future prognosis of therapeutically relevant ethical concerns". Journal of Medical Ethics. 37 (3): 137–43. doi:10.1136/jme.2010.039966. JSTOR 23034661. PMID 21106996. S2CID 13262044.
- ^ Jump up to: a b c Noohi S, Amirsalari S (2016). "History, Studies and Specific Uses of Repetitive Transcranial Magnetic Stimulation (rTMS) in Treating Epilepsy". Iranian Journal of Child Neurology. 10 (1): 1–8. PMC 4815479. PMID 27057180.
- ^ Klomjai W, Katz R, Lackmy-Vallée A (September 2015). "Basic principles of transcranial magnetic stimulation (TMS) and repetitive TMS (rTMS)". Annals of Physical and Rehabilitation Medicine. 58 (4): 208–213. doi:10.1016/j.rehab.2015.05.005. PMID 26319963.
- ^ Fang J, Zhou M, Yang M, Zhu C, He L (May 2013). "Repetitive transcranial magnetic stimulation for the treatment of amyotrophic lateral sclerosis or motor neuron disease". The Cochrane Database of Systematic Reviews (5): CD008554. doi:10.1002/14651858.CD008554.pub3. PMC 7173713. PMID 23728676.
- ^ Pereira LS, Müller VT, da Mota Gomes M, Rotenberg A, Fregni F (April 2016). "Safety of repetitive transcranial magnetic stimulation in patients with epilepsy: A systematic review". Epilepsy & Behavior. 57 (Pt A): 167–176. doi:10.1016/j.yebeh.2016.01.015. PMID 26970993. S2CID 3880211.
- ^ Martin PI, Naeser MA, Ho M, Treglia E, Kaplan E, Baker EH, Pascual-Leone A (November 2009). "Research with transcranial magnetic stimulation in the treatment of aphasia". Current Neurology and Neuroscience Reports. 9 (6): 451–8. doi:10.1007/s11910-009-0067-9. PMC 2887285. PMID 19818232.
- ^ Corti M, Patten C, Triggs W (March 2012). "Repetitive transcranial magnetic stimulation of motor cortex after stroke: a focused review". American Journal of Physical Medicine & Rehabilitation. 91 (3): 254–70. doi:10.1097/PHM.0b013e318228bf0c. PMID 22042336. S2CID 16233265.
- ^ Kleinjung T, Vielsmeier V, Landgrebe M, Hajak G, Langguth B (2008). "Transcranial magnetic stimulation: a new diagnostic and therapeutic tool for tinnitus patients". The International Tinnitus Journal. 14 (2): 112–8. PMID 19205161.
- ^ Shin SS, Dixon CE, Okonkwo DO, Richardson RM (November 2014). "Neurostimulation for traumatic brain injury". Journal of Neurosurgery. 121 (5): 1219–31. doi:10.3171/2014.7.JNS131826. PMID 25170668.
- ^ Machado S, Bittencourt J, Minc D, Portella CE, Velasques B, Cunha M, et al. (2008). "Therapeutic applications of repetitive transcranial magnetic stimulation in clinical neurorehabilitation". Functional Neurology. 23 (3): 113–22. PMID 19152730.
- ^ Jump up to: a b Chou YH, Hickey PT, Sundman M, Song AW, Chen NK (April 2015). "Effects of repetitive transcranial magnetic stimulation on motor symptoms in Parkinson disease: a systematic review and meta-analysis". JAMA Neurology. 72 (4): 432–40. doi:10.1001/jamaneurol.2014.4380. PMC 4425190. PMID 25686212.
- ^ Yang C, Guo Z, Peng H, Xing G, Chen H, McClure MA, et al. (November 2018). "Repetitive transcranial magnetic stimulation therapy for motor recovery in Parkinson's disease: A Meta-analysis". Brain and Behavior. 8 (11): e01132. doi:10.1002/brb3.1132. PMC 6236247. PMID 30264518.
- ^ Fregni F, Simon DK, Wu A, Pascual-Leone A (December 2005). "Non-invasive brain stimulation for Parkinson's disease: a systematic review and meta-analysis of the literature". Journal of Neurology, Neurosurgery, and Psychiatry. 76 (12): 1614–23. doi:10.1136/jnnp.2005.069849. PMC 1739437. PMID 16291882.
- ^ Lefaucheur JP (December 2009). "Treatment of Parkinson's disease by cortical stimulation". Expert Review of Neurotherapeutics. 9 (12): 1755–71. doi:10.1586/ern.09.132. PMID 19951135. S2CID 6404434.
- ^ Arias-Carrión O (April 2008). "Basic mechanisms of rTMS: Implications in Parkinson's disease". International Archives of Medicine. 1 (1): 2. doi:10.1186/1755-7682-1-2. PMC 2375865. PMID 18471317.
- ^ França C, de Andrade DC, Teixeira MJ, Galhardoni R, Silva V, Barbosa ER, Cury RG (2018). "Effects of cerebellar neuromodulation in movement disorders: A systematic review". Brain Stimulation. 11 (2): 249–260. doi:10.1016/j.brs.2017.11.015. PMID 29191439. S2CID 46810543.
- ^ Li H, Wang J, Li C, Xiao Z (September 2014). "Repetitive transcranial magnetic stimulation (rTMS) for panic disorder in adults". The Cochrane Database of Systematic Reviews. 9 (9): CD009083. doi:10.1002/14651858.CD009083.pub2. PMC 6885044. PMID 25230088.
- ^ Berlim MT, Neufeld NH, Van den Eynde F (August 2013). "Repetitive transcranial magnetic stimulation (rTMS) for obsessive-compulsive disorder (OCD): an exploratory meta-analysis of randomized and sham-controlled trials". Journal of Psychiatric Research. 47 (8): 999–1006. doi:10.1016/j.jpsychires.2013.03.022. PMID 23615189.
- ^ Saba G, Moukheiber A, Pelissolo A (May 2015). "Transcranial cortical stimulation in the treatment of obsessive-compulsive disorders: efficacy studies". Current Psychiatry Reports. 17 (5): 36. doi:10.1007/s11920-015-0571-3. PMID 25825002. S2CID 22071333.
- ^ Oberman LM, Enticott PG, Casanova MF, Rotenberg A, Pascual-Leone A, McCracken JT (February 2016). "Transcranial magnetic stimulation in autism spectrum disorder: Challenges, promise, and roadmap for future research". Autism Research. 9 (2): 184–203. doi:10.1002/aur.1567. PMC 4956084. PMID 26536383.
- ^ Nizard J, Lefaucheur JP, Helbert M, de Chauvigny E, Nguyen JP (July 2012). "Non-invasive stimulation therapies for the treatment of refractory pain". Discovery Medicine. 14 (74): 21–31. PMID 22846200. Archived from the original on 2014-02-26.
- ^ Kiebs, Maximilian; Hurlemann, René; Mutz, Julian (August 2019). "Repetitive transcranial magnetic stimulation in non-treatment-resistant depression". British Journal of Psychiatry. 215 (2): 445–446. doi:10.1192/bjp.2019.75. ISSN 0007-1250. PMID 31014413.
- ^ van Dun K, Bodranghien F, Manto M, Mariën P (June 2017). "Targeting the Cerebellum by Noninvasive Neurostimulation: a Review". Cerebellum. 16 (3): 695–741. doi:10.1007/s12311-016-0840-7. PMID 28032321. S2CID 3999098.
- ^ Duecker F, Sack AT (2015). "Rethinking the role of sham TMS". Frontiers in Psychology. 6: 210. doi:10.3389/fpsyg.2015.00210. PMC 4341423. PMID 25767458.
- ^ Davis NJ, Gold E, Pascual-Leone A, Bracewell RM (October 2013). "Challenges of proper placebo control for non-invasive brain stimulation in clinical and experimental applications". The European Journal of Neuroscience. 38 (7): 2973–7. doi:10.1111/ejn.12307. PMID 23869660. S2CID 2152097.
- ^ Marangell LB, Martinez M, Jurdi RA, Zboyan H (September 2007). "Neurostimulation therapies in depression: a review of new modalities". Acta Psychiatrica Scandinavica. 116 (3): 174–81. doi:10.1111/j.1600-0447.2007.01033.x. PMID 17655558. S2CID 38081703.
- ^ Brunoni AR, Lopes M, Kaptchuk TJ, Fregni F (2009). "Placebo response of non-pharmacological and pharmacological trials in major depression: a systematic review and meta-analysis". PLOS ONE. 4 (3): e4824. Bibcode:2009PLoSO...4.4824B. doi:10.1371/journal.pone.0004824. PMC 2653635. PMID 19293925.
- ^ Broadbent HJ, van den Eynde F, Guillaume S, Hanif EL, Stahl D, David AS, et al. (June 2011). "Blinding success of rTMS applied to the dorsolateral prefrontal cortex in randomised sham-controlled trials: a systematic review". The World Journal of Biological Psychiatry. 12 (4): 240–8. doi:10.3109/15622975.2010.541281. PMID 21426265. S2CID 21439740.
- ^ Wassermann EM, Zimmermann T (January 2012). "Transcranial magnetic brain stimulation: therapeutic promises and scientific gaps". Pharmacology & Therapeutics. 133 (1): 98–107. doi:10.1016/j.pharmthera.2011.09.003. PMC 3241868. PMID 21924290.
- ^ "FDA clears Nexstim´s Navigated Brain Stimulation for non-invasive cortical mapping prior to neurosurgery – Archive – Press Releases – News – Nexstim". nexstim.com.
- ^ "Nexstim Announces FDA Clearance for NexSpeech® – Enabling Noninvasive Speech Mapping Prior to Neurosurgery – Business Wire". businesswire.com. 11 June 2012.
- ^ Slotema CW, Blom JD, Hoek HW, Sommer IE (July 2010). "Should we expand the toolbox of psychiatric treatment methods to include Repetitive Transcranial Magnetic Stimulation (rTMS)? A meta-analysis of the efficacy of rTMS in psychiatric disorders". The Journal of Clinical Psychiatry. 71 (7): 873–84. doi:10.4088/JCP.08m04872gre. PMID 20361902.
- ^ Nakamura M (2012). "[Therapeutic application of repetitive transcranial magnetic stimulation for major depression]". Seishin Shinkeigaku Zasshi = Psychiatria et Neurologia Japonica. 114 (11): 1231–49. PMID 23367835.
- ^ (July 2015) "BRAINSWAY DEEP TMS SYSTEM" (PDF). Jan 7, 2013.
- ^ (July 2015)FDA 510K
- ^ Melkerson MN (2008-12-16). "Special Premarket 510(k) Notification for NeuroStar® TMS Therapy System for Major Depressive Disorder" (PDF). Food and Drug Administration. Retrieved 2010-07-16.
- ^ "Letter to Magstim Company Limited" (PDF). May 8, 2015.
- ^ "FDA approves Brainsway's depression treatment device". Globes. January 9, 2013. Archived from the original on December 16, 2013. Retrieved December 16, 2013.
- ^ The Royal Australian and New Zealand College of Psychiatrists. (2013) Position Statement 79. Repetitive Transcranial Magnetic Stimulation. Practice and Partnerships Committee
- ^ FDA 13 December 2013 FDA letter to eNeura re de novo classification review
- ^ Michael Drues, for Med Device Online. 5 February 2014 Secrets Of The De Novo Pathway, Part 1: Why Aren't More Device Makers Using It?
- ^ Schwedt TJ, Vargas B (September 2015). "Neurostimulation for Treatment of Migraine and Cluster Headache". Pain Medicine. 16 (9): 1827–34. doi:10.1111/pme.12792. PMC 4572909. PMID 26177612.
- ^ Jump up to: a b c "Brainsway reports positive Deep TMS system trial data for OCD". Medicaldevice-network. September 6, 2013. Retrieved December 16, 2013.
- ^ Jump up to: a b c d e "Brainsway's Deep TMS EU Cleared for Neuropathic Chronic Pain". medGadget. July 3, 2012. Retrieved December 16, 2013.
- ^ Gersner R, Oberman L, Sanchez MJ, Chiriboga N, Kaye HL, Pascual-Leone A, et al. (2016-01-01). "H-coil repetitive transcranial magnetic stimulation for treatment of temporal lobe epilepsy: A case report". Epilepsy & Behavior Case Reports. 5 (Supplement C): 52–6. doi:10.1016/j.ebcr.2016.03.001. PMC 4832041. PMID 27114902.
- ^ Torres F, Villalon E, Poblete P, Moraga-Amaro R, Linsambarth S, Riquelme R, et al. (2015-10-26). "Retrospective Evaluation of Deep Transcranial Magnetic Stimulation as Add-On Treatment for Parkinson's Disease". Frontiers in Neurology. 6: 210. doi:10.3389/fneur.2015.00210. PMC 4620693. PMID 26579065.
- ^ Luber B, Lisanby SH (January 2014). "Enhancement of human cognitive performance using transcranial magnetic stimulation (TMS)". NeuroImage. 85 Pt 3 (3): 961–70. doi:10.1016/j.neuroimage.2013.06.007. PMC 4083569. PMID 23770409.
- ^ "FDA permits marketing of transcranial magnetic stimulation for treatment of obsessive compulsive disorder". 2020-02-20.
- ^ NICE About NICE: What we do
- ^ Jump up to: a b "Transcranial magnetic stimulation for severe depression (IPG242)". London, England: National Institute for Health and Clinical Excellence. 2011-03-04.
- ^ "Transcranial magnetic stimulation for treating and preventing migraine". London, England: National Institute for Health and Clinical Excellence. January 2014.
- ^ "Repetitive transcranial magnetic stimulation for depression". National Institute for Health and Care Excellence. 16 December 2015. Retrieved 6 December 2019.
- ^ "Medical Policy: Transcranial Magnetic Stimulation for Depression and Other Neuropsychiatric Disorders". Policy No. BEH.00002. Anthem, Inc. 2013-04-16. Archived from the original on 2013-12-11. Retrieved 2013-12-11.
- ^ Health Net (March 2012). "National Medical Policy: Transcranial Magnetic Stimulation" (PDF). Policy Number NMP 508. Health Net. Archived from the original (PDF) on 2012-10-11. Retrieved 2012-09-05.
- ^ "Medical Policy Manual" (PDF). Section IV.67. Blue Cross Blue Shield of Nebraska. 2011-05-18. Archived from the original (PDF) on 2012-10-11.
- ^ "Medical Coverage Policy: Transcranial Magnetic Stimulation for Treatment of Depression and Other Psychiatric/Neurologic Disorders" (PDF). Blue Cross Blue Shield of Rhode Island. 2012-05-15. Archived from the original (PDF) on 2012-10-11. Retrieved 2012-09-05.
- ^ UnitedHealthcare (2013-12-01). "Transcranial Magnetic Stimulation" (PDF). UnitedHealthCare. p. 2. Archived from the original (PDF) on 2013-05-20. Retrieved 2013-12-11.
- ^ Aetna (2013-10-11). "Clinical Policy Bulletin: Transcranial Magnetic Stimulation and Cranial Electrical Stimulation". Number 0469. Aetna. Archived from the original on 2013-12-11. Retrieved 2013-12-11.
- ^ Cigna (2013-01-15). "Cigna Medical Coverage Policy: Transcranial Magnetic Stimulation" (PDF). Coverage Policy Number 0383. Cigna. Archived from the original (PDF) on 2013-12-11. Retrieved 2013-12-11.
- ^ Regence (2013-06-01). "Medical Policy: Transcranial Magnetic Stimulation as a Treatment of Depression and Other Disorders" (PDF). Policy No. 17. Regence. Archived from the original (PDF) on 2013-12-11. Retrieved 2013-12-11.
- ^ "Medicare Administrative Contractors". Centers for Medicare and Medicaid Services. 2013-07-10. Archived from the original on 2014-02-14. Retrieved 2014-02-14.
- ^ NHIC, Corp. (2013-10-24). "Local Coverage Determination (LCD) for Repetitive Transcranial Magnetic Stimulation (rTMS) (L32228)". Centers for Medicare and Medicaid Services. Archived from the original on 2014-02-17. Retrieved 2014-02-17.
- ^ "Important Treatment Option for Depression Receives Medicare Coverage". Press Release. PBN.com: Providence Business News. 2012-03-30. Archived from the original on 2012-10-11. Retrieved 2012-10-11.
- ^ The Institute for Clinical and Economic Review (June 2012). "Coverage Policy Analysis: Repetitive Transcranial Magnetic Stimulation (rTMS)" (PDF). The New England Comparative Effectiveness Public Advisory Council (CEPAC). Archived from the original (PDF) on 2013-12-11. Retrieved 2013-12-11.
- ^ "Transcranial Magnetic Stimulation Cites Influence of New England Comparative Effectiveness Public Advisory Council (CEPAC)". Berlin, Vermont: Central Vermont Medical Center. 2012-02-06. Archived from the original on 2012-10-13. Retrieved 2012-10-12.
- ^ National Government Services, Inc. (2013-10-25). "Local Coverage Determination (LCD): Transcranial Magnetic Stimulation (L32038)". Centers for Medicare and Medicaid Services. Retrieved 2014-02-17.
- ^ Novitas Solutions, Inc. (2013-12-04). "LCD L32752 – Transcranial Magnetic Stimulation for Depression". Contractor's Determination Number L32752. Centers for Medicare and Medicaid Services. Retrieved 2014-02-17.
- ^ Novitas Solutions, Inc. (2013-12-05). "LCD L33660 – Transcranial Magnetic Stimulation (TMS) for the Treatment of Depression". Contractor's Determination Number L33660. Centers for Medicare and Medicaid Services. Retrieved 2014-02-17.
- ^ Simpson KN, Welch MJ, Kozel FA, Demitrack MA, Nahas Z (March 2009). "Cost-effectiveness of transcranial magnetic stimulation in the treatment of major depression: a health economics analysis". Advances in Therapy. 26 (3): 346–68. doi:10.1007/s12325-009-0013-x. PMID 19330495. S2CID 11136891.
- ^ https://www.cyprusrtms.com
- ^ https://www.cut.ac.cy/faculties/hsc/reh/research/research-labs/the-neurorehabilitation-lab/
- Physical psychiatric treatments
- Electrotherapy
- Magnetic devices
- Neurophysiology
- Neuropsychology
- Neurotechnology
- Treatment of bipolar disorder
- Treatment of depression
- Medical devices
- 1985 introductions
- 2008 introductions
- Bioelectromagnetics

