Amyloidosis
| Amyloidosis | |
|---|---|
 | |
| Classic facial features of AL amyloidosis with bleeding under the skin (bruising) around the eyes[1] | |
| Specialty | Endocrinology, rheumatology, cardiology |
| Symptoms | Feeling tired, weight loss, swelling of the legs, shortness of breath, bleeding, feeling light headed with standing[2] |
| Usual onset | 55–65 years old[2] |
| Causes | Genetic or acquired[3] |
| Diagnostic method | Tissue biopsy[2] |
| Treatment | Supportive care, directed at the underlying cause, dialysis, organ transplantation[3] |
| Prognosis | Improved with treatment[3] |
| Frequency | 3–13 per million per year (AL amyloidosis)[2] |
| Deaths | 1 per 1,000 people (developed world)[3] |
Amyloidosis is a group of diseases in which abnormal proteins, known as amyloid fibrils, build up in tissue.[4] There are several types with varying symptoms; signs and symptoms may include diarrhea, weight loss, feeling tired, enlargement of the tongue, bleeding, numbness, feeling faint with standing, swelling of the legs, or enlargement of the spleen.[2]
There are about 30 different types of amyloidosis, each due to a specific protein misfolding.[5] Some are genetic while others are acquired.[3] They are grouped into localized forms, and systemic ones.[2] The four most common types of systemic amyloidosis are light chain (AL), inflammation (AA), dialysis-related (Aβ2M), and hereditary and old age (ATTR and familial amyloid polyneuropathy[6]).[2]
Diagnosis may be suspected when protein is found in the urine, organ enlargement is present, or problems are found with multiple peripheral nerves and it is unclear why.[2] Diagnosis is confirmed by tissue biopsy.[2] Due to the variable presentation, a diagnosis can often take some time to reach.[3]
Treatment is geared towards decreasing the amount of the involved protein.[2] This may sometimes be achieved by determining and treating the underlying cause.[2] AL amyloidosis occurs in about 3–13 per million people per year and AA amyloidosis in about 2 per million people per year.[2] The usual age of onset of these two types is 55 to 60 years old.[2] Without treatment, life expectancy is between six months and four years.[2] In the developed world about 1 per 1,000 people die annually from amyloidosis.[3] Amyloidosis has been described since at least 1639.[2]
Signs and symptoms[]

The presentation of amyloidosis is broad and depends on the site of amyloid accumulation. The kidney and heart are the most common organs involved.
Kidneys[]
Amyloid deposition in the kidneys can cause nephrotic syndrome, which results from a reduction in the kidney's ability to filter and hold on to proteins. The nephrotic syndrome occurs with or without elevations in creatinine and blood urea concentration,[7] two biochemical markers of kidney injury. In AA amyloidosis, the kidneys are involved in 91–96% of people,[8] symptoms ranging from protein in the urine to nephrotic syndrome and rarely chronic kidney disease.
Heart[]
Amyloid deposition in the heart can cause both diastolic and systolic heart failure. EKG changes may be present, showing low voltage and conduction abnormalities like atrioventricular block or sinus node dysfunction. On echocardiography, the heart shows a restrictive filling pattern, with normal to mildly reduced systolic function.[7] AA amyloidosis usually spares the heart.[8] Cardiac amyloidosis can present with symptoms of heart failure including shortness of breath, fatigue, and edema.[9] As cardiac amyloidosis progresses, the amyloid deposition can affect the heart's ability to pump and fill blood as well as its ability to maintain normal rhythm, which leads to worsening heart function and decline in people's quality of life.[9]
Brain[]
People with amyloidosis do not get central nervous system involvement but can develop sensory and autonomic neuropathies. Sensory neuropathy develops in a symmetrical pattern and progresses in a distal to proximal manner. Autonomic neuropathy can present as orthostatic hypotension but may manifest more gradually with nonspecific gastrointestinal symptoms like constipation, nausea, or early satiety.[7]
Liver[]
Accumulation of amyloid proteins in the liver can lead to elevations in serum aminotransferases and alkaline phosphatase, two biomarkers of liver injury, which is seen in about one third of people.[8] Liver enlargement is common. In contrast, spleen enlargement is rare, occurring in 5% of people. Splenic dysfunction, leading to the presence of Howell-Jolly bodies on blood smear, occurs in 24% of people with amyloidosis.[7] Malabsorption is seen in 8.5% of AL amyloidosis and 2.4% of AA amyloidosis. One suggested mechanism for the observed malabsorption is that amyloid deposits in the tips of intestinal villi (fingerlike projections that increase the intestinal area available for absorption of food), begin to erode the functionality of the villi, presenting a sprue-like picture.[8]
Glands[]
Both the thyroid and adrenal glands can be infiltrated. It is estimated that 10–20% of individuals with amyloidosis have hypothyroidism. Adrenal infiltration may be harder to appreciate given that its symptoms of orthostatic hypotension and low blood sodium concentration may be attributed to autonomic neuropathy and heart failure.[7]
"Amyloid deposits occur in the pancreas of patients with diabetes mellitus, although it is not known if this is functionally important. The major component of pancreatic amyloid is a 37-amino acid residue peptide known as islet amyloid polypeptide or 'amylin.' This is stored with insulin in secretory granules in B cells and is co secreted with insulin." (Rang and Dale's Pharmacology, 2015.)
Musculoskeletal system[]
Amyloid proteins deposit most commonly inside the knee, followed by hands, wrists, elbow, hip, and ankle, causing joint pain.[10] In males with advanced age (>80 years), there is significant risk of wild-type transthyretin amyloid deposition in synovial tissue of knee joint, but predominantly in old age deposition of wild type transthyretin is seen in cardiac ventricles. In beta 2-microglobulin amyloidosis, males have high risk of getting carpal tunnel syndrome.[11] Aβ2MG amyloidosis (Hemodialysis associated amyloidosis) tends to deposit in synovial tissue, causing chronic inflammation of the synovial tissue in knee, hip, shoulder and interphalangeal joints.[11] Amyloid light chains deposition in shoulder joint causes enlarged shoulders, also known as "shoulder pad sign".[11] Amyloid light chain depositions can also cause bilateral symmetric polyarthritis.[11]
The deposition of amyloid proteins in the bone marrow without causing plasma cell dyscrasias is called amyloidoma. It is commonly found in cervical, lumbar, and sacral vertebrae. Those affected may be presented with bone pain due to bone lysis, lumbar paraparesis, and a variety of neurological symptoms. Vertebral fractures are also common.[11]
Eyes[]
A rare development is amyloid purpura, a susceptibility to bleeding with bruising around the eyes, termed "raccoon-eyes", caused by amyloid deposition in the blood vessels and reduced activity of thrombin and factor X, two clotting proteins that lose their function after binding with amyloid.[7]
Oral cavity[]
Amyloid deposits in tissue can cause enlargement of structures. Twenty percent of people with AL amyloidosis have an enlarged tongue, that can lead to obstructive sleep apnea, difficulty swallowing, and altered taste.[8] Tongue enlargement does not occur in ATTR or AA amyloidosis.[7] Deposition of amyloid in the throat can cause hoarseness.[7]
Pathogenesis[]
Amyloidoses can be considered protein misfolding diseases.[12][13] The vast majority of proteins that have been found to form amyloid deposits are secreted proteins, so the misfolding and formation of amyloid occurs outside cells, in the extracellular space.[12] Of the 37 proteins so far identified as being vulnerable to amyloid formation, only four are cytosolic.[12] Most amyloid-forming proteins are relatively small, but otherwise there is currently no evidence of structural or functional similarities among proteins known to form disease-associated amyloids.[12] One third of amyloid disease is hereditary, in which case there is normally an early age of onset.[12] Half of amyloid-related diseases are sporadic and have a late age of onset – in these cases, the protein aggregation may be associated with aging-related decline in protein regulation. Rarely, some medical treatments are associated with amyloid disease.[12]
Amyloid-forming proteins aggregate into distinctive fibrillar forms with a beta-sheet structure.[12][13] The process of forming amyloid fibrils is thought to have intermediate oligomeric forms. Both the oligomers and amyloid fibrils can be toxic to cells and can interfere with proper organ function.[14] The relative significance of different aggregation species may depend on the protein involved and the organ system affected.[13]
Diagnosis[]
Diagnosis of amyloidosis generally requires tissue biopsy. The biopsy is assessed for evidence of characteristic amyloid deposits. The tissue is treated with various stains. The most useful stain in the diagnosis of amyloid is Congo red, which, combined with polarized light, makes the amyloid proteins appear apple-green on microscopy. Also, thioflavin T stain may be used.[15] A number of imaging techniques such as a DPD scan or SAP scan are also in use.[16]
A sample of tissue can be biopsied or obtained directly from the affected internal organ, but the first-line site of biopsy is subcutaneous abdominal fat, known as a "fat pad biopsy", due to its ease of acquisition.[17][18] An abdominal fat biopsy is not completely sensitive and may result in false negatives, which means a negative result does not exclude the diagnosis of amyloidosis.[17][18] However, direct biopsy of the affected organ may still be unnecessary as other less invasive methods of biopsy can also be used, including rectal salivary gland biopsy, lip, or bone marrow biopsy which can achieve a diagnosis in up to 85% of people.[17]
In the amyloid deposition of the joints, there will be a decreased signal in both T1 and T2 weighted MRI images.[10] In amyloidoma, there will be low T1 signal with gadolinium injection and low T2 signal.[11]
The type of the amyloid protein can be determined in various ways: the detection of abnormal proteins in the bloodstream (on protein electrophoresis or light chain determination); binding of particular antibodies to the amyloid found in the tissue (immunohistochemistry); or extraction of the protein and identification of its individual amino acids.[15] Immunohistochemistry can identify AA amyloidosis the majority of the time, but can miss many cases of AL amyloidosis.[8] Laser microdissection with mass spectrometry is the most reliable method of identifying the different forms of amyloidosis.[19]
AL is the most common form of amyloidosis, and a diagnosis often begins with a search for plasma cell dyscrasia, memory B cells producing aberrant immunoglobulins or portions of immunoglobulins. Immunofixation electrophoresis of urine or serum is positive in 90% of people with AL amyloidosis.[7] Immunofixation electrophoresis is more sensitive than regular electrophoresis but may not be available in all centers. Alternatively immunohistochemical staining of a bone marrow biopsy looking for dominant plasma cells can be sought in people with a high clinical suspicion for AL amyloidosis but negative electrophoresis.[7]
ATTR, or familial transthyretin-associated amyloidosis, is suspected in people with family history of idiopathic neuropathies or heart failure who lack evidence of plasma cell dyscrasias. ATTR can be identified using isoelectric focusing which separates mutated forms of transthyretin. Findings can be corroborated by genetic testing to look for specific known mutations in transthyretin that predispose to amyloidosis.[7]
AA is suspected on clinical grounds in individuals with longstanding infections or inflammatory diseases. AA can be identified by immunohistochemistry staining.[7]

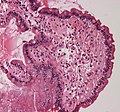
Small bowel duodenum with amyloid deposition Congo red 10X

Amyloidosis, dystrophic calcification
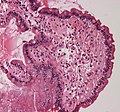
Small bowel duodenum with amyloid deposition 20X

Amyloidosis, Node, Congo Red

Amyloidosis, blood vessels, H&E

Amyloidosis, lymph node, H&E

Amyloidosis, lymph node, polarizer

Micrograph showing amyloid deposition (red fluffy material) in the heart (cardiac amyloidosis). Congo red stain.
Classification[]
Historical classification systems were based on clinical factors. Until the early 1970s, the idea of a single amyloid substance predominated. Various descriptive classification systems were proposed based on the organ distribution of amyloid deposits and clinical findings. Most classification systems included primary (i.e., idiopathic) amyloidosis, in which no associated clinical condition was identified, and secondary amyloidosis (i.e., secondary to chronic inflammatory conditions). Some classification systems included myeloma-associated, familial, and localized amyloidosis.
The modern era of amyloidosis classification began in the late 1960s with the development of methods to make amyloid fibrils soluble. These methods permitted scientists to study the chemical properties of amyloids. Descriptive terms such as primary amyloidosis, secondary amyloidosis, and others (e.g., senile amyloidosis), which are not based on cause, provide little useful information and are no longer recommended.
The modern classification of amyloid disease tends to use an abbreviation of the protein that makes the majority of deposits, prefixed with the letter A. For example, amyloidosis caused by transthyretin is termed "ATTR". Deposition patterns vary between people but are almost always composed of just one amyloidogenic protein. Deposition can be systemic (affecting many different organ systems) or organ-specific. Many amyloidoses are inherited, due to mutations in the precursor protein.
Other forms are due to different diseases causing overabundant or abnormal protein production – such as with overproduction of immunoglobulin light chains (termed AL amyloidosis), or with continuous overproduction of acute phase proteins in chronic inflammation (which can lead to AA amyloidosis).
About 60 amyloid proteins have been identified so far.[20] Of those, at least 36 have been associated with a human disease.[21]
The names of amyloids usually start with the letter "A". Here is a brief description of the more common types of amyloid:
| Abbr. | Amyloid type/Gene | Description | OMIM |
|---|---|---|---|
| AL | amyloid light chain | AL amyloidosis / multiple myeloma. Contains immunoglobulin light-chains (λ,κ) derived from plasma cells. | 254500 |
| AA | SAA | Serum amyloid A protein (SAA) is an acute-phase reactant that is produced in times of inflammation. | |
| Aβ | β amyloid/APP | Found in Alzheimer disease brain lesions. | 605714 |
| ALECT2 | LECT2 | In LECT2 amyloidosis, the LECT2 protein deposits in the kidneys and various other tissues but only kidneys show signs or symptoms; these are typical those of kidney failure.[22] | |
| ATTR | transthyretin | Transthyretin is a protein that is mainly formed in the liver that transports thyroxine and retinol binding protein.[7] A mutant form of a normal serum protein that is deposited in the genetically determined familial amyloid polyneuropathies. TTR is also deposited in the heart in wild-type transthyretin amyloidosis, also known as senile systemic amyloidosis.[23] Also found in leptomeningeal amyloidosis. | 105210 |
| Aβ2M | β2 microglobulin | Not to be confused with Aβ, β2m is a normal serum protein, part of major histocompatibility complex (MHC) Class 1 molecules. Haemodialysis-associated amyloidosis | |
| AIAPP | amylin | Found in the pancreas of people with type 2 diabetes. | |
| APrP | prion protein | In prion diseases, misfolded prion proteins deposit in tissues and resemble amyloid proteins. Some examples are Creutzfeldt–Jakob disease (humans), BSE or "mad cow disease" (cattle), and scrapie (sheep and goats). A recently described familial prion disease presents with peripheral amyloidosis causing autonomic neuropathy and diarrhea.[24] | 123400 |
| AGel | GSN | Finnish type amyloidosis | 105120 |
| ACys | CST3 | Cerebral amyloid angiopathy, Icelandic-type | 105150 |
| AApoA1 | APOA1 | Familial visceral amyloidosis | 105200 |
| AFib | FGA | Familial visceral amyloidosis | 105200 |
| ALys | LYZ | Familial visceral amyloidosis | 105200 |
| ? | OSMR | Primary cutaneous amyloidosis | 105250 |
| ABri ADan |
ITM2B | Cerebral amyloid angiopathy, British-type Danish-type |
176500 117300 |
| APro | prolactin | Prolactinoma | |
| AKer | keratoepithelin | Familial corneal amyloidosis | |
| AANF | atrial natriuretic factor | Senile amyloid of atria of heart | |
| ACal | calcitonin | Medullary carcinoma of the thyroid |
As of 2010, 27 human and 9 animal fibril proteins were classified, along with 8 inclusion bodies.[25]
Alternative[]
An older clinical method of classification refers to amyloidoses as systemic or localised
- Systemic amyloidoses affect more than one body organ or system. Examples are AL, AA and Aβ2m.[26]
- Localised amyloidoses affect only one body organ or tissue type. Examples are Aβ, IAPP, Atrial natriuretic factor (in isolated atrial amyloidosis), and Calcitonin (in medullary carcinoma of the thyroid)[26]
Another classification is primary or secondary.
- Primary amyloidoses arise from a disease with disordered immune cell function, such as multiple myeloma or other immunocyte dyscrasias.
- Secondary (reactive) amyloidoses occur as a complication of some other chronic inflammatory or tissue-destroying disease. Examples are reactive systemic amyloidosis and secondary cutaneous amyloidosis.[26]
Additionally, based on the tissues in which it is deposited, it is divided into mesenchymal (organs derived from mesoderm) or parenchymal (organs derived from ectoderm or endoderm).
Treatment[]
Treatment depends on the type of amyloidosis that is present. Treatment with high dose melphalan, a chemotherapy agent, followed by stem cell transplantation has shown promise in early studies and is recommended for stage I and II AL amyloidosis.[19] However, only 20–25% of people are eligible for stem cell transplant. Chemotherapy and steroids, with melphalan plus dexamethasone, is mainstay treatment in AL people not eligible for transplant.[19]
In AA, symptoms may improve if the underlying condition is treated; eprodisate has been shown to slow renal impairment by inhibiting polymerization of amyloid fibrils.[27]
Management of ATTR amyloidosis will depend on its classification as wild type or variant.[28] Both may be treated with tafamidis, a low toxicity oral agent that prevents destabilization of correctly folded protein.[28] Studies showed tafamidis reduced mortality and hospitalization due to heart failure.[28] Previously, for variant ATTR amyloidosis, liver transplant was the only effective treatment.[28] However, newer therapies including diflunisal, an anti-inflammatory drug, and inotersen and patisiran, drugs which prevent misfolded protein formation, have shown early promises in slowing disease progression.[28] The latter two drugs have shown their benefit in neurological impairment scores and quality of life measures.[28] However, their role in cardiac ATTR amyloidosis is still being investigated.[28]
In 2018, patisiran was not recommended by NICE in the UK for hereditary transthyretin-related amyloidosis.[29] As of July 2019 further review however is occurring.[30] It was approved for this use in the United States however.[31]
In 2018, inotersen was approved by the European Medicines Agency to treat polyneuropathy in adult patients with hereditary transthyretin amyloidosis [32]
In 2021, in a clinical trial using the CRISPR gene-editing technique, several participants had an "80% to 96% drop in TTR levels, on par or better than the average of 81%" who were given patisiran[33]
Support groups[]
People affected by amyloidosis are supported by organizations, including the Amyloidosis Research Consortium, Amyloidosis Foundation, Amyloidosis Support Groups, and Amyloidosis Australia.[34][35]
Prognosis[]
Prognosis varies with the type of amyloidosis and the affected organ system. Prognosis for untreated AL cardiac amyloidosis is poor, with a median survival of six months.[36] More specifically, AL amyloidosis can be classified as stage I, II or III based on cardiac biomarkers like Nt-proBNP and cardiac troponin.[37] Survival diminishes with increasing stage, however recent advancements in treatments have improved median survival rates for stages I, II, and III, to 91.2, 60, and 7 months respectively.[37]
Outcomes in a person with AA amyloidosis depend on the underlying disease and correlate with the concentration of serum amyloid A protein.[8]
People with ATTR have a better prognosis and may survive for over a decade.[7]
Senile systemic amyloidosis was determined to be the primary cause of death for 70% of people over 110 who have been autopsied.[38][39]
Epidemiology[]
Amyloidosis has a combined estimated prevalence of 30 per 100,000 persons with the three most common forms being AL, ATTR, and AA.[40] The median age at diagnosis is 64.[8]
AL has the highest incidence at approximately 12 cases per million persons per year and an estimated prevalence of 30,000 to 45,000 cases in the US and European Union.[40][41]
AA amyloidoses is the most common form in developing countries and can complicate longstanding infections with tuberculosis, osteomyelitis, and bronchiectesis. In the west, AA is more likely to occur from autoimmune inflammatory states.[7] The most common causes of AA amyloidosis in the West are rheumatoid arthritis, inflammatory bowel disease, psoriasis, and familial Mediterranean fever.
People undergoing long-term hemodialysis (14–15 years) can develop amyloidosis from accumulation of light chains of the HLA 1 complex which is normally filtered out by the kidneys.[8]
Senile amyloidosis resulting from deposition of normal transthyretin, mainly in the heart, is found in 10–36% of people over 80.[8]
Research[]
Treatments for ATTR-related neuropathy include TTR-specific oligonucleotides in the form of small interfering RNA (patisiran) or antisense inotersen,[42] the former having recently received FDA approval.[43] Research into treatments for ATTR amyloidosis have compared liver transplantation, oral drugs that stabilize the misfolding protein (including tafamidis and diflunisal), and newer therapeutic agents still being investigated (including patisiran).[44] Based on available research, liver transplant remains the most effective treatment option for advanced ATTR amyloidosis, protein stabilizing drugs may slow disease progression but were insufficient to justify delay of liver transplant, and newer agents such as patisiran require additional studies.[44]
See also[]
References[]
- ^ Hawkins P (29 April 2015). "AL amyloidosis". Wikilite.com. Archived from the original on 22 December 2015. Retrieved 19 December 2015.
- ^ Jump up to: a b c d e f g h i j k l m n o Hazenberg BP (May 2013). "Amyloidosis: a clinical overview" (PDF). Rheumatic Diseases Clinics of North America. 39 (2): 323–45. doi:10.1016/j.rdc.2013.02.012. PMID 23597967. S2CID 215069282.
- ^ Jump up to: a b c d e f g Pepys MB (2006). "Amyloidosis". Annual Review of Medicine. 57: 223–41. doi:10.1146/annurev.med.57.121304.131243. PMID 16409147.
- ^ "AL amyloidosis". rarediseases.info.nih.gov. Genetic and Rare Diseases Information Center (GARD). Archived from the original on 24 April 2017. Retrieved 22 April 2017.
- ^ Sipe JD, Benson MD, Buxbaum JN, Ikeda S, Merlini G, Saraiva MJ, Westermark P (December 2014). "Nomenclature 2014: Amyloid fibril proteins and clinical classification of the amyloidosis". Amyloid. 21 (4): 221–4. doi:10.3109/13506129.2014.964858. PMID 25263598. S2CID 41000320.
- ^ Ando Y, Coelho T, Berk JL, Cruz MW, Ericzon BG, Ikeda S, et al. (February 2013). "Guideline of transthyretin-related hereditary amyloidosis for clinicians". Orphanet Journal of Rare Diseases. 8: 31. doi:10.1186/1750-1172-8-31. PMC 3584981. PMID 23425518.
- ^ Jump up to: a b c d e f g h i j k l m n o Falk RH, Comenzo RL, Skinner M (September 1997). "The systemic amyloidoses". The New England Journal of Medicine. 337 (13): 898–909. doi:10.1056/NEJM199709253371306. PMID 9302305.
- ^ Jump up to: a b c d e f g h i j Ebert EC, Nagar M (March 2008). "Gastrointestinal manifestations of amyloidosis". The American Journal of Gastroenterology. 103 (3): 776–87. PMID 18076735.
- ^ Jump up to: a b Kyriakou P, Mouselimis D, Tsarouchas A, Rigopoulos A, Bakogiannis C, Noutsias M, Vassilikos V (December 2018). "Diagnosis of cardiac amyloidosis: a systematic review on the role of imaging and biomarkers". BMC Cardiovascular Disorders. 18 (1): 221. doi:10.1186/s12872-018-0952-8. PMC 6278059. PMID 30509186.
- ^ Jump up to: a b Takahashi N, Glockner J, Howe BM, Hartman RP, Kawashima A (May 2016). "Taxonomy and Imaging Manifestations of Systemic Amyloidosis". Radiologic Clinics of North America. 54 (3): 597–612. doi:10.1016/j.rcl.2015.12.012. PMID 27153791.
- ^ Jump up to: a b c d e f Nguyen TX, Naqvi A, Thompson TL, Wilson RH (Spring 2018). "Musculoskeletal Manifestations of Amyloidosis: A Focused Review". Journal of Surgical Orthopaedic Advances. 27 (1): 1–5. PMID 29762107.
- ^ Jump up to: a b c d e f g Chiti F, Dobson CM (June 2017). "Protein Misfolding, Amyloid Formation, and Human Disease: A Summary of Progress Over the Last Decade". Annual Review of Biochemistry. 86: 27–68. doi:10.1146/annurev-biochem-061516-045115. PMID 28498720.
- ^ Jump up to: a b c Merlini, Giampaolo; Seldin, David C.; Gertz, Morie A. (10 May 2011). "Amyloidosis: Pathogenesis and New Therapeutic Options". Journal of Clinical Oncology. 29 (14): 1924–1933. doi:10.1200/JCO.2010.32.2271. PMC 3138545. PMID 21483018.
- ^ [1], Karp, Judith E., ed. Amyloidosis Diagnosis and Treatment. Rochester: Humana, 2010. Online Source.
- ^ Jump up to: a b Dember LM (December 2006). "Amyloidosis-associated kidney disease". Journal of the American Society of Nephrology. 17 (12): 3458–71. doi:10.1681/ASN.2006050460. PMID 17093068. Archived from the original on 2011-12-05.
- ^ Sachchithanantham S, Wechalekar AD (2013). "Imaging in systemic amyloidosis". British Medical Bulletin. 107: 41–56. doi:10.1093/bmb/ldt021. PMID 23896486.
- ^ Jump up to: a b c Merlini G, Dispenzieri A, Sanchorawala V, Schönland SO, Palladini G, Hawkins PN, Gertz MA (October 2018). "Systemic immunoglobulin light chain amyloidosis" (PDF). Nature Reviews. Disease Primers. 4 (1): 38. doi:10.1038/s41572-018-0034-3. PMID 30361521. S2CID 53023121.
- ^ Jump up to: a b Wechalekar AD, Gillmore JD, Hawkins PN (June 2016). "Systemic amyloidosis". Lancet. 387 (10038): 2641–2654. doi:10.1016/S0140-6736(15)01274-X. PMID 26719234. S2CID 4762107.
- ^ Jump up to: a b c Rosenzweig M, Landau H (November 2011). "Light chain (AL) amyloidosis: update on diagnosis and management". Journal of Hematology & Oncology. 4 (1): 47. doi:10.1186/1756-8722-4-47. PMC 3228694. PMID 22100031.
- ^ Mok KH, Pettersson J, Orrenius S, Svanborg C (March 2007). "HAMLET, protein folding, and tumor cell death". Biochemical and Biophysical Research Communications. 354 (1): 1–7. doi:10.1016/j.bbrc.2006.12.167. PMID 17223074.
- ^ Pettersson-Kastberg J, Aits S, Gustafsson L, Mossberg A, Storm P, Trulsson M, et al. (November 2008). "Can misfolded proteins be beneficial? The HAMLET case". Annals of Medicine. 41 (3): 162–76. doi:10.1080/07853890802502614. PMID 18985467. S2CID 31198109.
- ^ Slowik V, Apte U (July 2017). "Leukocyte Cell-Derived Chemotaxin-2: It's [sic] Role in Pathophysiology and Future in Clinical Medicine". Clinical and Translational Science. 10 (4): 249–259. doi:10.1111/cts.12469. PMC 5504477. PMID 28466965.
- ^ Hassan W, Al-Sergani H, Mourad W, Tabbaa R (2005). "Amyloid heart disease. New frontiers and insights in pathophysiology, diagnosis, and management". Texas Heart Institute Journal. 32 (2): 178–84. PMC 1163465. PMID 16107109.
- ^ Mead S, Gandhi S, Beck J, Caine D, Gallujipali D, Carswell C, et al. (November 2013). "A novel prion disease associated with diarrhea and autonomic neuropathy". The New England Journal of Medicine. 369 (20): 1904–14. doi:10.1056/NEJMoa1214747. PMC 3863770. PMID 24224623.
- ^ Sipe JD, Benson MD, Buxbaum JN, Ikeda S, Merlini G, Saraiva MJ, Westermark P (September 2010). "Amyloid fibril protein nomenclature: 2010 recommendations from the nomenclature committee of the International Society of Amyloidosis". Amyloid. 17 (3–4): 101–4. doi:10.3109/13506129.2010.526812. PMID 21039326.
- ^ Jump up to: a b c Table 5-12 in: Mitchell RS, Kumar V, Abbas AK, Fausto N (2007). Robbins Basic Pathology. Philadelphia: Saunders. ISBN 978-1-4160-2973-1. 8th edition.
- ^ Real de Asúa D, Costa R, Galván JM, Filigheddu MT, Trujillo D, Cadiñanos J (2014). "Systemic AA amyloidosis: epidemiology, diagnosis, and management". Clin Epidemiol. 6: 369–77. doi:10.2147/CLEP.S39981. PMC 4218891. PMID 25378951.
- ^ Jump up to: a b c d e f g Gertz MA, Dispenzieri A (July 2020). "Systemic Amyloidosis Recognition, Prognosis, and Therapy: A Systematic Review". JAMA. 324 (1): 79–89. doi:10.1001/jama.2020.5493. PMID 32633805.
- ^ "Patisiran for treating hereditary transthyretinrelated amyloidosis". Retrieved 20 July 2019.
- ^ "Patisiran for treating hereditary transthyretin-related amyloidosis [ID1279] | Guidance | NICE". www.nice.org.uk. Retrieved 20 July 2019.
- ^ Hoy SM (October 2018). "Patisiran: First Global Approval". Drugs. 78 (15): 1625–1631. doi:10.1007/s40265-018-0983-6. PMID 30251172. S2CID 52813638.
- ^ https://www.ema.europa.eu/en/medicines/human/EPAR/tegsedi
- ^ Gillmore, Julian D.; Gane, Ed; Taubel, Jorg; Kao, Justin; Fontana, Marianna; Maitland, Michael L.; Seitzer, Jessica; o'Connell, Daniel; Walsh, Kathryn R.; Wood, Kristy; Phillips, Jonathan; Xu, Yuanxin; Amaral, Adam; Boyd, Adam P.; Cehelsky, Jeffrey E.; McKee, Mark D.; Schiermeier, Andrew; Harari, Olivier; Murphy, Andrew; Kyratsous, Christos A.; Zambrowicz, Brian; Soltys, Randy; Gutstein, David E.; Leonard, John; Sepp-Lorenzino, Laura; Lebwohl, David (2021). "CRISPR-Cas9 in Vivo Gene Editing for Transthyretin Amyloidosis". New England Journal of Medicine. 385 (6): 493–502. doi:10.1056/NEJMoa2107454. PMID 34215024.
- ^ "Amyloidosis - NORD (National Organization for Rare Disorders)". NORD (National Organization for Rare Disorders). Archived from the original on 2016-03-16. Retrieved 2016-03-15.
- ^ "Amyloidosis primary cutaneous – Disease – Organizations – Genetic and Rare Diseases Information Center (GARD) – NCATS Program". rarediseases.info.nih.gov. Archived from the original on 2016-03-15. Retrieved 2016-03-15.
- ^ Merlini G (December 2017). "AL amyloidosis: from molecular mechanisms to targeted therapies". Hematology. American Society of Hematology. Education Program. 2017 (1): 1–12. doi:10.1182/asheducation-2017.1.1. PMC 6142527. PMID 29222231.
- ^ Jump up to: a b Falk RH, Alexander KM, Liao R, Dorbala S (September 2016). "AL (Light-Chain) Cardiac Amyloidosis: A Review of Diagnosis and Therapy". Journal of the American College of Cardiology. 68 (12): 1323–41. doi:10.1016/j.jacc.2016.06.053. PMID 27634125.
- ^ Coles LS, Young RD (May 2012). "Supercentenarians and transthyretin amyloidosis: the next frontier of human life extension". Preventive Medicine. 54 Suppl (Suppl): S9-11. doi:10.1016/j.ypmed.2012.03.003. PMID 22579241.
- ^ "Searching for the Secrets of the Super Old". Science. 26 September 2008. pp. 1764–1765. Archived from the original on 9 March 2013. Retrieved 22 February 2013.
- ^ Jump up to: a b Lin HM, Gao X, Cooke CE, Berg D, Labotka R, Faller DV, et al. (June 2017). "Disease burden of systemic light-chain amyloidosis: a systematic literature review". Current Medical Research and Opinion. 33 (6): 1017–1031. doi:10.1080/03007995.2017.1297930. PMID 28277869. S2CID 205541963.
- ^ Gertz MA, Dispenzieri A (July 2020). "Systemic Amyloidosis Recognition, Prognosis, and Therapy: A Systematic Review". JAMA. 324 (1): 79–89. doi:10.1001/jama.2020.5493. PMID 32633805.
- ^ Buxbaum JN (July 2018). "Oligonucleotide Drugs for Transthyretin Amyloidosis". The New England Journal of Medicine. 379 (1): 82–85. doi:10.1056/nejme1805499. PMID 29972750.
- ^ Office of the Commissioner. "Press Announcements - FDA approves first-of-its kind targeted RNA-based therapy to treat a rare disease". www.fda.gov. Retrieved 2018-08-11.
- ^ Jump up to: a b Cristóbal Gutiérrez H, Pelayo-Negro AL, Gómez Gómez D, Martín Vega MÁ, Valero Domínguez M (July 2020). "Overview of treatments used in transthyretin-related hereditary amyloidosis: a systematic review". European Journal of Hospital Pharmacy. 27 (4): 194–201. doi:10.1136/ejhpharm-2018-001823. PMC 7335620. PMID 32587078.
External links[]
| Classification | |
|---|---|
| External resources |
- Amyloidosis
- Protein folding
- Skin conditions resulting from errors in metabolism