Birth weight

Birth weight is the body weight of a baby at its birth.[1] The average birth weight in babies of European descent is 3.5 kilograms (7.7 lb), with the normative range between 2.5 and 4.5 kilograms (5.5 and 9.9 lb). On average, babies of South Asian and Chinese descent weigh about 3.26 kilograms (7.2 lb).[2][3] The birth weight of a baby is notable because infants with a very low birth weight are 100 times more likely to die compared to normal birth weight babies.[4] As far as low birth weight prevalence rates changing over time, there has been a slight decrease from 7.9% (1970) to 6.8% (1980), then a slight increase to 8.3% (2006), to the current levels of 8.2% (2016).[4][5] The prevalence of low birth weights has trended slightly upward from 2012 to the present.[6]
There have been numerous studies that have attempted, with varying degrees of success, to show links between birth weight and later-life conditions, including diabetes, obesity, tobacco smoking, and intelligence. Low birth weight is associated with neonatal infection and infant mortality.
Abnormalities[]
- A low birth weight can be caused either by a preterm birth (low gestational age at birth) or of the infant being small for gestational age (slow prenatal growth rate), or a combination of both.[7] Potential causes of low birth weight can also be cause by health issues in the person giving birth, genetic factors, or problems in the placenta.[8]
- A very large birth weight is usually caused by the infant having been large for gestational age. Infants that are large for gestational age have been associated with significantly higher rates of neonatal morbidity.[9]
Determinants[]

Genetics[]
There are two genetic loci that have been strongly linked to birth weight, ADCY5 and CCNL1, as well four that show some evidence (CDKAL1, HHEX-IDE, GCK, and TCF7L2).[10][11][12] The heritability of birth weight ranges from 25-40 %.[13][14] There is a complex relationship between a baby's genes and the maternal environment that the child is developing in. Foetal genes influence how the fetus grows in utero, and the maternal genes influence how the environment affects the growing fetus.[11]
Maternal health[]
The health of the mother during the pregnancy can affect birth weight. A pre-existing disease or acquired disease in pregnancy is sometimes associated with decreased birth weight. For example, celiac disease confers an odds ratio of low birth weight of approximately 1.8.[15] Certain medications (e.g. for high blood pressure or epilepsy) can put a mother at a higher risk for delivering a low birth weight baby.[7] Women younger than 15 or older than 35 are at a higher risk to have a low-birth weight baby.[7][16] Multiple births, where a mother has more than one child at one time, can also be a determinant in birth weight as each baby is likely to be outside the AGA (appropriate for gestational age). Multiple births put children at a higher rate to have low birth weight (56.6%) compared to children born in a single birth ( 6.2%).[4] Low birth weight can also vary by maternal age. In 2008 the rate of low birth weight was the highest in babies born to women younger than 15 years old (12.4%).[16] Women aged 40–54 had a rate of low birth weight at 11.8 percent. The lowest rates of low birth weight happened among babies whose mothers were between the ages of 25–29 years (4.4%) and 30–34 years (7.6%).[16]
Stress[]
Stressful events have been demonstrated to produce significant effects on birth weight. Those mothers who have stressful events during pregnancy, especially during the first and second trimester, are at higher risk to deliver low-birth weight babies.[17][18] Researchers furthered this study and found that maternal stressful events that occur prior to conception have a negative impact on birth weight as well, and can result in a higher risk for preterm and lower birth weight babies.[19][20][21] Women who experienced abuse (physical, sexual, or emotional) during pregnancy are also at increased risk of delivering a low-birth weight baby.[22] For example, in a study completed by Witt et. al, those women who experienced a stressful event (ie. death of close family member, infertility issues, separation from partner) prior to conception had 38% more of a chance to have a very low birth weight baby compared to those who had not experienced a stressful life event.[19] The theory is that stress can impact a baby based on two different mechanisms: neuroendocrine pathway or immune/inflammatory pathway.[23][24] Stress causes the body to produce stress hormones called glucocorticoids that can suppress the immune system., as well as raises levels of placental corticotropin-releasing hormone (CRH) which can lead to preterm labor.[25][24] These findings can pose evidence for future prevention efforts for low birth weight babies. One way to decrease rates of low birth weight and premature delivery is to focus on the health of women prior to conception through reproductive education, screening and counseling regarding mental health issues and stress, and access to primary care.[26]
Racial stress[]
Non-Hispanic Blacks have the highest infant mortality rate in the United States (11.4 deaths per 1,000 live births compared to the national average of 5.9 deaths per 1,000 live births).[27] Subsequently, there has been growing research supporting the idea of racial discrimination as a risk factor for low birth weight. In one study by Collins et. al, evidence suggested that African American mothers who experienced high levels of racial discrimination were at significantly higher risk of delivering a very low-birth weight baby compared to African American mothers who had not experienced racial discrimination.[28] Black infants (13.2%) are more likely to have low birth weight compared to Asian and Pacific Islander (8.1%), American Indian and Alaska Native (7.6%), Non-Hispanic White (7.0%), and Hispanic Infants (7.1%).[4]
Environmental factors[]
Environmental factors, including exposure of the mother to secondhand smoke[29] can be a factor in determining the birth weight of child. In 2014, 13% of children exposed to smoke were born with low birth weight compared with 7.5% of those children born to nonsmokers.[4] Children born to mothers who smoked or were exposed to secondhand smoke are more likely to develop health problems earlier in life such as neurodevelopmental delays.[30] When mothers actively smoke during pregnancy, their child is at a higher risk of being born with a low birth weight.[31] Smoking can also be a stress management tool used by expecting mothers.[32] There is some support for lower socioeconomic status of the parents being a determinant of low birth weight, but there is conflicting evidence, as socioeconomic status is tied to many other factors.[33][34][35]
Neonatal care[]
Most babies admitted to the NICU are born before 37 weeks of pregnancy or have low birth weight which is less than 5.5 pounds.[36] They could also have a medical condition that requires special care. In the United States nearly half a million babies are born preterm. Because of this, many of these babies also have low birth weights.[36] There are four levels of care in the neonatal care units. Intensive Care, High Dependency Care, Low Dependency, and Transitional Care are the four levels:[37]
- Intensive Care: For babies with serious problems. This includes babies born three months early and have extremely low birth weight.
- High Dependency Care: For babies with less serious problem, but who still may not to be looked after or babies that are recovering from a critical illness.
- Low Dependency Care: For babies that do not need a continuous supervision.
- Transitional Care: For babies that still need medical treatment, but are well enough to be called for at their mother’s bedside.
Influence on the first few years of life[]

Children born with an abnormally low birth weight can have significant problems within the first few years of life. They may have trouble gaining weight, obtaining adequate nutrition, and supporting a strong immune system. They also have higher risks for mortality, behavior problems, and mental deficiencies.[33] Low birth weight babies are more likely to develop the following conditions after birth compared to normal birth weight babies:[7]
- Breathing problems (infant respiratory distress syndrome)
- Bleeding in the brain (intraventricular hemorrhage)
- Patent ductus arteriosus (PDA)
- Necrotizing enterocolitis
- Retinopathy of prematurity
- Jaundice
- Infections
That said, the effects of low birth weight on a child's first few years of life are often intertwined with other maternal, environmental, and genetic factors and most effects of low birth weight are only slightly negatively significant on a child's life when these factors are controlled for.[38] When these factors are controlled, the only significant effect low birth weight has on a child's development is physical growth in the early years and the likelihood of being underweight compared to normal birth weight babies.[38]
Influence on adult life[]
Studies have been conducted to investigate how a person's birth weight can influence aspects of their future life. This includes theorised links with obesity, diabetes and intelligence.
Obesity and diabetes[]
A baby born small or large for gestational age (either of the two extremes) is thought to have an increased risk of obesity in later life,[40][41] but it was also shown that this relationship is fully explained by maternal weight.[42] Middle aged adults with low birth weight present with a higher chance of obesity and diabetes. Children that are born under six pounds were 1.27 times more likely to develop diabetes compared to babies born at a healthy weight over six pounds.
Growth hormone (GH) therapy at a certain dose induced catch-up of lean body mass (LBM). However percentage body fat decreased in the GH-treated subjects. Bone mineral density SDS measured by DEXA increased significantly in the GH-treated group compared to the untreated subjects, though there is much debate over whether or not SGA (small for gestational age) is significantly adverse to children to warrant inducing catch-up.[43] Babies that have a low birth weight are thought to have an increased risk of developing type 2 diabetes in later life.[44][45][46][47] Low birth weight is linked with increase rates of obesity, insulin resistance, and type 2 diabetes and it is shown that children with the low birth weights have increased leptin levels after they catch up growth during childhood.[48] Adiponectin levels are positively related with birth weight and BMI in babies with an increase of risk of type 2 diabetes.[48] The leptin and adiponection mechanisms are still being studied when involving low birth weight.[48]
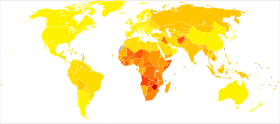
Around the world[]
There is much variation regarding birth weight within continents, countries, and cities. Even though over 20 million babies are born each year with low birth weight, it is hard to know the exact number as more than half of babies born in the world are not weighed at birth.[49] The baby’s weight is an indicator of the mother and baby's health. In 2013, 22 million newborns had low birth weight, around 16 percent of all babies globally.[50] Data on low birth weight is adjusted to account for under reporting. South Asia has the highest rate of babies not weighed at birth with 66 percent, but also have the highest low birth weight at 28 percent worldwide.[50] West and Central Africa and least developed countries are next with 14 percent low birth weight worldwide.[50]
More than 96.5% of low birth weight babies are born in developing countries around the world.[33] Because low birth weight babies can require more extensive care, it places a financial burden on communities.
Prevention[]
The World Health Organization (WHO) recently announced an initiative to have a thirty percent reduction in low birth weight worldwide. This is public health priority, as birth weight can have short and long term effects. WHO estimates that worldwide, 15-20 % of all births each year are considered low birth weight, which is about 20 million births.[51]
The start of prenatal care is very important to help prevent low birth weight and early medical problems. Going to regular doctor’s visits is very important for the health of the mother and the baby. At the visits the OB/GYN will be checking maternal nutrition and weight gain because that is linked with the baby’s weight gain. The mother having a healthy diet is essential for the baby. Maintaining good nutrition by taking folic acid, which can be found in fruits and vegetables, is linked to the prevention of[52][53] premature births and low birth weight. Alcohol, cigarettes, and drugs should also be avoided during pregnancy because they can also lead to poor growth and other complications. By seeing the doctor they are also able to monitor pre-existing medical illnesses to make sure they are under control during pregnancy. Mothers with high blood pressure and type 2 diabetes are more likely to have infants with low birth weights.[54] One essential action to increase normal birth weights is to have affordable, accessible, and culturally sensitive prenatal care worldwide. This is essential not just for treating low birth weight, but also preventing it. Other prevention efforts include: smoking cessation programs, food-distribution systems, stress reduction and social service supports.[51]
See also[]
References[]
- ^ "Definitions". Georgia Department of Public Health. 4 December 2008. Archived from the original on 2 April 2012.
Birthweight: Infant's weight recorded at the time of birth
- ^ "New birth weight curves tailored to baby's ethnicity | Toronto Star". thestar.com. 15 February 2012. Retrieved 22 September 2016.
- ^ Janssen PA, Thiessen P, Klein MC, Whitfield MF, Macnab YC, Cullis-Kuhl SC (July 2007). "Standards for the measurement of birth weight, length and head circumference at term in neonates of European, Chinese and South Asian ancestry". Open Medicine. 1 (2): e74-88. PMC 2802014. PMID 20101298.
- ^ a b c d e "Low and very low birthweight infants". Child Trends Databank. 2016.
- ^ "FastStats". www.cdc.gov. 8 August 2018. Retrieved 25 November 2018.
- ^ Martin JA, Hamilton BE, Osterman MJ, Driscoll AK, Drake P (January 2018). "Births: Final Data for 2016". National Vital Statistics Reports. 67 (1): 1–55. PMID 29775434.
- ^ a b c d "Low birthweight". Retrieved 25 November 2018.
- ^ "Birth Weight". medlineplus.gov. Retrieved 29 October 2020.
- ^ Mendez-Figueroa H, Truong VT, Pedroza C, Chauhan SP (June 2017). "Large for Gestational Age Infants and Adverse Outcomes among Uncomplicated Pregnancies at Term". American Journal of Perinatology. 34 (7): 655–662. doi:10.1055/s-0036-1597325. PMID 27926975. S2CID 4165673.
- ^ Freathy RM, Mook-Kanamori DO, Sovio U, Prokopenko I, Timpson NJ, Berry DJ, et al. (May 2010). "Variants in ADCY5 and near CCNL1 are associated with fetal growth and birth weight". Nature Genetics. 42 (5): 430–5. doi:10.1038/ng.567. PMC 2862164. PMID 20372150.
- ^ a b Yaghootkar H, Freathy RM (May 2012). "Genetic origins of low birth weight". Current Opinion in Clinical Nutrition and Metabolic Care. 15 (3): 258–64. doi:10.1097/mco.0b013e328351f543. PMID 22406741. S2CID 3402464.
- ^ Ryckman KK, Feenstra B, Shaffer JR, Bream EN, Geller F, Feingold E, et al. (January 2012). "Replication of a genome-wide association study of birth weight in preterm neonates". The Journal of Pediatrics. 160 (1): 19–24.e4. doi:10.1016/j.jpeds.2011.07.038. PMC 3237813. PMID 21885063.
- ^ Clausson B, Lichtenstein P, Cnattingius S (March 2000). "Genetic influence on birthweight and gestational length determined by studies in offspring of twins". BJOG. 107 (3): 375–81. doi:10.1111/j.1471-0528.2000.tb13234.x. PMID 10740335. S2CID 43470321.
- ^ Lunde A, Melve KK, Gjessing HK, Skjaerven R, Irgens LM (April 2007). "Genetic and environmental influences on birth weight, birth length, head circumference, and gestational age by use of population-based parent-offspring data". American Journal of Epidemiology. 165 (7): 734–41. doi:10.1093/aje/kwk107. PMID 17311798.
- ^ Tersigni C, Castellani R, de Waure C, Fattorossi A, De Spirito M, Gasbarrini A, et al. (2014). "Celiac disease and reproductive disorders: meta-analysis of epidemiologic associations and potential pathogenic mechanisms". Human Reproduction Update. 20 (4): 582–93. doi:10.1093/humupd/dmu007. PMID 24619876.
- ^ a b c "Low Birth Weight". Child Health USA 2011. Retrieved 25 November 2018.
- ^ Hedegaard M, Henriksen TB, Secher NJ, Hatch MC, Sabroe S (July 1996). "Do stressful life events affect duration of gestation and risk of preterm delivery?". Epidemiology. 7 (4): 339–45. doi:10.1097/00001648-199607000-00001. JSTOR 3702049. PMID 8793357. S2CID 25514196.
- ^ Zhu P, Tao F, Hao J, Sun Y, Jiang X (July 2010). "Prenatal life events stress: implications for preterm birth and infant birthweight". American Journal of Obstetrics and Gynecology. 203 (1): 34.e1–8. doi:10.1016/j.ajog.2010.02.023. PMID 20417475.
- ^ a b Witt WP, Cheng ER, Wisk LE, Litzelman K, Chatterjee D, Mandell K, Wakeel F (February 2014). "Maternal stressful life events prior to conception and the impact on infant birth weight in the United States". American Journal of Public Health. 104 Suppl 1 (1): S81-9. doi:10.2105/AJPH.2013.301544. PMC 3975462. PMID 24354829.
- ^ Khashan AS, McNamee R, Abel KM, Mortensen PB, Kenny LC, Pedersen MG, et al. (February 2009). "Rates of preterm birth following antenatal maternal exposure to severe life events: a population-based cohort study". Human Reproduction. 24 (2): 429–37. doi:10.1093/humrep/den418. PMID 19054778.
- ^ Class QA, Khashan AS, Lichtenstein P, Långström N, D'Onofrio BM (July 2013). "Maternal stress and infant mortality: the importance of the preconception period". Psychological Science. 24 (7): 1309–16. doi:10.1177/0956797612468010. PMC 3713176. PMID 23653129.
- ^ Murphy CC, Schei B, Myhr TL, Du Mont J (May 2001). "Abuse: a risk factor for low birth weight? A systematic review and meta-analysis". CMAJ. 164 (11): 1567–72. PMC 81110. PMID 11402794.
- ^ Wadhwa PD, Culhane JF, Rauh V, Barve SS (June 2001). "Stress and preterm birth: neuroendocrine, immune/inflammatory, and vascular mechanisms". Maternal and Child Health Journal. 5 (2): 119–25. doi:10.1023/A:1011353216619. PMID 11573837. S2CID 13524067.
- ^ a b Wadhwa PD, Culhane JF, Rauh V, Barve SS, Hogan V, Sandman CA, et al. (July 2001). "Stress, infection and preterm birth: a biobehavioural perspective". Paediatric and Perinatal Epidemiology. 15 Suppl 2 (s2): 17–29. doi:10.1046/j.1365-3016.2001.00005.x. PMID 11520397.
- ^ Rich-Edwards J, Krieger N, Majzoub J, Zierler S, Lieberman E, Gillman M (July 2001). "Maternal experiences of racism and violence as predictors of preterm birth: rationale and study design". Paediatric and Perinatal Epidemiology. 15 Suppl 2 (s2): 124–35. doi:10.1046/j.1365-3016.2001.00013.x. PMID 11520405.
- ^ Cheng TL, Kotelchuck M, Guyer B (2012). "Preconception women's health and pediatrics: an opportunity to address infant mortality and family health". Academic Pediatrics. 12 (5): 357–9. doi:10.1016/j.acap.2012.04.006. PMC 4443477. PMID 22658953.
- ^ "Infant Mortality | Maternal and Infant Health | Reproductive Health | CDC". www.cdc.gov. 3 August 2018.
- ^ Collins JW, David RJ, Handler A, Wall S, Andes S (December 2004). "Very low birthweight in African American infants: the role of maternal exposure to interpersonal racial discrimination". American Journal of Public Health. 94 (12): 2132–8. doi:10.2105/AJPH.94.12.2132. PMC 1448603. PMID 15569965.
- ^ "The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General". Surgeon General of the United States. 27 June 2006. p. 198–205. Retrieved 16 June 2014.
- ^ Lee BE, Hong YC, Park H, Ha M, Kim JH, Chang N, et al. (May 2011). "Secondhand smoke exposure during pregnancy and infantile neurodevelopment". Environmental Research. 111 (4): 539–44. Bibcode:2011ER....111..539L. doi:10.1016/j.envres.2011.02.014. PMID 21397902.
- ^ Pereira PP, Da Mata FA, Figueiredo AC, de Andrade KR, Pereira MG (May 2017). "Maternal Active Smoking During Pregnancy and Low Birth Weight in the Americas: A Systematic Review and Meta-analysis". Nicotine & Tobacco Research. 19 (5): 497–505. doi:10.1093/ntr/ntw228. PMID 28403455. S2CID 3803610.
- ^ Damron KR (May 2017). "Review of the Relationships Among Psychosocial Stress, Secondhand Smoke, and Perinatal Smoking". Journal of Obstetric, Gynecologic, and Neonatal Nursing. 46 (3): 325–333. doi:10.1016/j.jogn.2017.01.012. PMID 28390924. S2CID 4576511.
- ^ a b c Mahumud RA, Sultana M, Sarker AR (January 2017). "Distribution and Determinants of Low Birth Weight in Developing Countries". Journal of Preventive Medicine and Public Health = Yebang Uihakhoe Chi. 50 (1): 18–28. doi:10.3961/jpmph.16.087. PMC 5327679. PMID 28173687.
- ^ Parker JD, Schoendorf KC, Kiely JL (July 1994). "Associations between measures of socioeconomic status and low birth weight, small for gestational age, and premature delivery in the United States". Annals of Epidemiology. 4 (4): 271–8. doi:10.1016/1047-2797(94)90082-5. PMID 7921316.
- ^ Martinson ML, Reichman NE (April 2016). "Socioeconomic Inequalities in Low Birth Weight in the United States, the United Kingdom, Canada, and Australia". American Journal of Public Health. 106 (4): 748–54. doi:10.2105/AJPH.2015.303007. PMC 4986052. PMID 26794171.
- ^ a b "The Neonatal Intensive Care Unit". Stanford Children Health. Retrieved 15 November 2018.
- ^ "What is neonatal care?". Liverpools Womens NHS Foundation Trust. Retrieved 25 November 2018.
- ^ a b Datar A, Jacknowitz A (November 2009). "Birth weight effects on children's mental, motor, and physical development: evidence from twins data". Maternal and Child Health Journal. 13 (6): 780–94. doi:10.1007/s10995-009-0461-6. PMC 2855622. PMID 19308711.
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved 11 November 2009.
- ^ "3 stages of childhood may predict obesity risk - Fitness - NBC News". 3 June 2005. Retrieved 28 November 2007.
- ^ Singhal A, Wells J, Cole TJ, Fewtrell M, Lucas A (March 2003). "Programming of lean body mass: a link between birth weight, obesity, and cardiovascular disease?". The American Journal of Clinical Nutrition. 77 (3): 726–30. doi:10.1093/ajcn/77.3.726. PMID 12600868.
- ^ Parsons TJ, Power C, Manor O (December 2001). "Fetal and early life growth and body mass index from birth to early adulthood in 1958 British cohort: longitudinal study". BMJ. 323 (7325): 1331–5. doi:10.1136/bmj.323.7325.1331. PMC 60670. PMID 11739217.
- ^ "GH Treatment Effects on Body Composition in SGA". Growth, Genetics & Hormones. 24 (1). May 2008. Archived from the original on 22 June 2008.
- ^ "Low birth weight diabetes link". BBC News. 25 February 2005. Retrieved 28 November 2007.
- ^ Gillman MW, Rifas-Shiman S, Berkey CS, Field AE, Colditz GA (March 2003). "Maternal gestational diabetes, birth weight, and adolescent obesity". Pediatrics. 111 (3): e221-6. doi:10.1542/peds.111.3.e221. PMID 12612275.
- ^ Rich-Edwards JW, Colditz GA, Stampfer MJ, Willett WC, Gillman MW, Hennekens CH, et al. (February 1999). "Birthweight and the risk for type 2 diabetes mellitus in adult women". Annals of Internal Medicine. 130 (4 Pt 1): 278–84. doi:10.7326/0003-4819-130-4_part_1-199902160-00005. PMID 10068385. S2CID 17291266.
- ^ Li Y, Ley SH, Tobias DK, Chiuve SE, VanderWeele TJ, Rich-Edwards JW, et al. (July 2015). "Birth weight and later life adherence to unhealthy lifestyles in predicting type 2 diabetes: prospective cohort study". BMJ. 351: h3672. doi:10.1136/bmj.h3672. PMC 4510778. PMID 26199273.
- ^ a b c Jornayvaz FR, Vollenweider P, Bochud M, Mooser V, Waeber G, Marques-Vidal P (May 2016). "Low birth weight leads to obesity, diabetes and increased leptin levels in adults: the CoLaus study". Cardiovascular Diabetology. 15: 73. doi:10.1186/s12933-016-0389-2. PMC 4855501. PMID 27141948.
- ^ "Low birthweight - UNICEF DATA". UNICEF DATA. Retrieved 25 November 2018.
- ^ a b c "Low BirthWeight". UNICEF DATA. Retrieved 25 November 2018.
- ^ a b "Global Nutrition Targets 2025: Low birth weight policy brief". World Health Organization. Archived from the original on 18 February 2015. Retrieved 25 November 2018.
- ^ "New study examines effect of timing of folic acid supplementation during pregnancy". ScienceDaily.com.
- ^ Hodgetts VA, Morris RK, Francis A, Gardosi J, Ismail KM (March 2015). "Effectiveness of folic acid supplementation in pregnancy on reducing the risk of small-for-gestational age neonates: a population study, systematic review and meta-analysis". BJOG. 122 (4): 478–90. doi:10.1111/1471-0528.13202. PMID 25424556. S2CID 8243224.
- ^ "Low and Very Low Birth Weight Babies:Prevention Tips for Expectant Mothers". HealthXchange. Retrieved 16 November 2018.
Further reading[]
- Peleg D, Kennedy CM, Hunter SK (August 1998). "Intrauterine growth restriction: identification and management". American Family Physician. 58 (2): 453–60, 466–7. PMID 9713399.
- Jornayvaz FR, Vollenweider P, Bochud M, Mooser V, Waeber G, Marques-Vidal P (May 2016). "Low birth weight leads to obesity, diabetes and increased leptin levels in adults: the CoLaus study". Cardiovascular Diabetology. 15: 73. doi:10.1186/s12933-016-0389-2. PMC 4855501. PMID 27141948.
External links[]
- Obstetrics
- Neonatology
- Human body weight
- Midwifery