Fungal sinusitis
| Fungal sinusitis | |
|---|---|
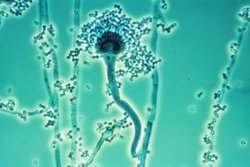 | |
| Aspergillus is responsible in 90% of cases of fungal sinusitis | |
| Specialty | Pulmonology |
| Symptoms | Facial pain[1] |
| Types | Invasive, Non-invasive[1] |
| Diagnostic method | CT scan, MRI[1] |
| Treatment | Surgical(Management depends on which type)[1] |
Fungal sinusitis is the inflammation of the lining mucosa of the paranasal sinuses due to fungal infection.[1] It occurs in people with reduced immunity. The maxillary sinus is the most commonly involved. Fungi responsible for fungal sinusitis are Aspergillus fumigatus (90%), Aspergillus flavus, and Aspergillus niger. Fungal sinusitis occurs most commonly in middle-aged populations. Diabetes mellitus is the most common risk factor involved.[2]
Types[]
The types of fungal sinusitis are based on invasive and non-invasive as follows:[4][5]
- Invasive
- Acute fulminant
- Chronic invasive
- Granulomatous
- Non Invasive
- Saprophytic infection
- Sinus fungal ball
- Eosinophil related FRS including AFRS
Signs and symptoms[]
Individuals with the condition of fungal sinusitis mostly present with features that include facial pain and pain around the eyes, nasal congestion, rhinorrhea(running nose), headache, later there may be ophthalmoplegia (paralysis of ocular muscles).[1]
Pathophysiology[]
The mechanism of fungal sinusitis depends on which form, such as:
- Acute fulminant form – the fungus invades into vessels causing thrombosis, necrosis with minimum inflammation [3]
- Chronic invasive – fungal hyphae invades tissue leaving necrosis with minimal inflammation [3]
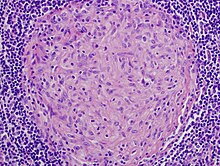
- Granulomatous form – invasive hyphae invades tissue with inflammation and non-caseating granuloma (with foreign bodies).[3]
- Saprophytic infection – growth of fungus seen on mucous crusts within sinus cavity.[3]
- Sinus fungal ball – sequestration of fungal hyphae as densely tangled, and has gritty matted appearance.[3]
- Eosinophil related Allergic fungal sinusitis – though not completely understood, a possible mechanism sees the protein component of fungus elicits IgE mediated allergic mucosal inflammation.[6]
Diagnosis[]
In terms of diagnosis, the clinical examination gives an idea about fungal sinusitis,[5] as well as:

- Suggestive clinical features include - multiple recurrent episodes, persistent pathology, and absent ability to smell (the Eustachian tube may also be affected).[5]
- X Ray - can be done if the diagnosis is not certain.[5]
- CT – can document the presence of sinusitis, in the coronal views[1]
- MRI – used to find the CNS spread (extent of the disease), to evaluate individuals who demonstrate signs of invasive fungal sinusitis [1]
- Histology studies[1]
Treatment[]
Treatment for fungal sinusitis can include surgical debridement; helps by slowing progression of disease thus allowing time for recovery[7] additionally we see the options below:
- In cases where the fungus has invaded the sinus tissue, echinocandins, oral voriconazole, and I.V amphotericin may be used[8]
- For allergic fungal sinusitis, systemic corticosteroids like prednisolone, methylprednisolone are added for their anti-inflammatory effect, bronchodilators and expectorants help to clear secretions in the sinuses.[medical citation needed]
Epidemiology[]
Though it is widely held that fungal infections of the nose and paranasal sinuses are not common, most agree that their frequency has been increasing over past decades.[9]
See also[]
References[]
- ^ Jump up to: a b c d e f g h i "Fungal Sinusitis: Background, History of the Procedure, Problem". eMedicine. 28 June 2016. Retrieved 25 November 2016.
- ^ P. Karthikeyan, V. Nirmal Coumare (October–December 2010). "Incidence and presentation of fungal sinusitis in patient diagnosed with chronic rhinosinusitis". Indian Journal of Otolaryngology Head and Neck Surgery. 62 (4): 381–5. doi:10.1007/s12070-010-0062-0. PMC 3266098. PMID 22319697.CS1 maint: uses authors parameter (link)subscription needed
- ^ Jump up to: a b c d e f "Granulomatous Diseases of the Head and Neck: Overview, Autoimmune Granulomatous Diseases, Granulomatous Diseases of Unknown Etiology". eMedicine. 2018-08-24. Retrieved 11 September 2016.
- ^ Chakrabarti, Arunaloke; Denning, David W.; Ferguson, Berrylin J.; Ponikau, Jens; Buzina, Walter; Kita, Hirohito; Marple, Bradley; Panda, Naresh; Vlaminck, Stephan (2017-01-29). "Fungal Rhinosinusitis: A Categorization and Definitional Schema Addressing Current Controversies". The Laryngoscope. 119 (9): 1809–1818. doi:10.1002/lary.20520. ISSN 0023-852X. PMC 2741302. PMID 19544383.
- ^ Jump up to: a b c d "Sinusitis. Medical professional reference for Sinusitis. | Patient". Patient. Retrieved 29 January 2017.
- ^ Glass, Daniel; Amedee, Ronald G. (1 January 2011). "Allergic Fungal Rhinosinusitis: A Review". The Ochsner Journal. 11 (3): 271–275. ISSN 1524-5012. PMC 3179194. PMID 21960761.
- ^ Soler, Zachary M.; Schlosser, Rodney J. (1 January 2012). "The role of fungi in diseases of the nose and sinuses". American Journal of Rhinology & Allergy. 26 (5): 351–358. doi:10.2500/ajra.2012.26.3807. ISSN 1945-8924. PMC 3904040. PMID 23168148.
- ^ Hupp, James R.; Ferneini, Elie M. (2016). Head, Neck and Orofacial Infections: An Interdisciplinary Approach E-Book. Elsevier Health Sciences. p. 45. ISBN 9780323289467. Retrieved 4 March 2017.
- ^ Karthikeyan, P.; Nirmal Coumare, V. (2017-01-29). "Incidence and Presentation of Fungal Sinusitis in Patient Diagnosed with Chronic Rhinosinusitis". Indian Journal of Otolaryngology and Head & Neck Surgery. 62 (4): 381–385. doi:10.1007/s12070-010-0062-0. ISSN 2231-3796. PMC 3266098. PMID 22319697.
Further reading[]
- Thaler, Erica; Kennedy, David W. (2008). Rhinosinusitis: A Guide for Diagnosis and Management. Springer Science & Business Media. ISBN 9780387730622. Retrieved 22 February 2017.
- Aribandi, Manohar; McCoy, Victor A.; Bazan, Carlos (2007). "Imaging Features of Invasive and Noninvasive Fungal Sinusitis: A Review". RadioGraphics. 27 (5): 1283–1296. doi:10.1148/rg.275065189. PMID 17848691.
External links[]
| Classification | |
|---|---|
| External resources |
| Scholia has a topic profile for Fungal sinusitis. |
- Nose disorders