History of penicillin

The history of penicillin follows a number of observations and discoveries of apparent evidence of antibiotic activity of the mould Penicillium that led to the development of penicillins that became the most widely used antibiotics. Following the identification of Penicillium rubens as the source of the compound in 1928 and with the production of pure compound in 1942, penicillin became the first naturally derived antibiotic. There are anecdotes about ancient societies using moulds to treat infections, and in the following centuries many people observed the inhibition of bacterial growth by various moulds.[1] However, it is unknown if the species involved were Penicillium species or if the antimicrobial substances produced were penicillin.
While working at St Mary's Hospital in London, Scottish physician Alexander Fleming was the first to experimentally discover that a Penicillium mould secretes an antibacterial substance, and the first to concentrate the active substance involved, which he named penicillin in 1928.[2][3] The mould was determined to be a rare variant of Penicillium notatum (now Penicillium rubens), a laboratory contaminant in his lab.[4] For the next 16 years, he pursued better methods of production of penicillin, medicinal uses and clinical trial. His successful treatment of Harry Lambert who had otherwise-fatal streptococcal meningitis in 1942 proved to be a critical moment in the medical usage of penicillin.
Many later scientists were involved in the stabilization and mass production of penicillin and in the search for more productive strains of Penicillium.[5] Important contributors include Ernst Chain, Howard Florey, Norman Heatley and Edward Abraham.[2] Fleming, Florey and Chain shared the 1945 Nobel Prize in Physiology or Medicine for the discovery and development of penicillin.[6] Dorothy Hodgkin received the 1964 Nobel Prize in Chemistry determining the structures of important biochemical substances including penicillin. Shortly after the discovery of penicillin, there were reports of penicillin resistance in many bacteria. Research that aims to circumvent and understand the mechanisms of antibiotic resistance continues today.[7][8]
Early history[]
Many ancient cultures, including those in Egypt, Greece and India, independently discovered the useful properties of fungi and plants in treating infection.[9] These treatments often worked because many organisms, including many species of mould, naturally produce antibiotic substances. However, ancient practitioners could not precisely identify or isolate the active components in these organisms.
In 17th-century Poland, wet bread was mixed with spider webs (which often contained fungal spores) to treat wounds. The technique was mentioned by Henryk Sienkiewicz in his 1884 book With Fire and Sword. In England in 1640, the idea of using mould as a form of medical treatment was recorded by apothecaries such as John Parkinson, King's Herbarian, who advocated the use of mould in his book on pharmacology.[10]
Early scientific evidence[]
The modern history of penicillin research begins in earnest in the 1870s in the United Kingdom. Sir John Scott Burdon-Sanderson, who started out at St. Mary's Hospital (1852–1858) and later worked there as a lecturer (1854–1862), observed that culture fluid covered with mould would produce no bacterial growth. Burdon-Sanderson's discovery prompted Joseph Lister, an English surgeon and the father of modern antisepsis, to discover in 1871 that urine samples contaminated with mould also did not permit the growth of bacteria. Lister also described the antibacterial action on human tissue of a species of mould he called Penicillium glaucum.[11] A nurse at King's College Hospital whose wounds did not respond to any traditional antiseptic was then given another substance that cured him, and Lister's registrar informed him that it was called Penicillium. In 1874, the Welsh physician William Roberts, who later coined the term "enzyme", observed that bacterial contamination is generally absent in laboratory cultures of Penicillium glaucum. John Tyndall followed up on Burdon-Sanderson's work and demonstrated to the Royal Society in 1875 the antibacterial action of the Penicillium fungus.[12]
In 1876, German biologist Robert Koch discovered that Bacillus anthracis was the causative pathogen of anthrax,[13] which became the first demonstration that a specific bacterium caused a specific disease, and the first direct evidence of germ theory of diseases.[14] In 1877, French biologists Louis Pasteur and Jules Francois Joubert observed that cultures of the anthrax bacilli, when contaminated with moulds, could be successfully inhibited.[15] Reporting in the Comptes Rendus de l'Académie des Sciences, they concluded:
Neutral or slightly alkaline urine is an excellent medium for the bacteria... But if when the urine is inoculated with these bacteria an aerobic organism, for example one of the "common bacteria," is sown at the same time, the anthrax bacterium makes little or no growth and sooner or later dies out altogether. It is a remarkable thing that the same phenomenon is seen in the body even of those animals most susceptible to anthrax, leading to the astonishing result that anthrax bacteria can be introduced in profusion into an animal, which yet does not develop the disease; it is only necessary to add some "common 'bacteria" at the same time to the liquid containing the suspension of anthrax bacteria. These facts perhaps justify the highest hopes for therapeutics.[16]
The phenomenon was described by Pasteur and Koch as antibacterial activity and was named as "antibiosis" by French biologist Jean Paul Vuillemin in 1877.[17][18] (The term antibiosis, meaning "against life", was adopted as "antibiotic" by American biologist and later Nobel laureate Selman Waksman in 1947.[19]) It has also been asserted that Pasteur identified the strain as Penicillium notatum. However, Paul de Kruif's 1926 Microbe Hunters describes this incident as contamination by other bacteria rather than by mould.[20] In 1887, Swiss physician Carl Alois Philipp Garré developed a test method using glass plate to see bacterial inhibition and found similar results.[18] Using his gelatin-based culture plate, he grew two different bacteria and found that their growths were inhibited differently, as he reported:
I inoculated on the untouched cooled [gelatin] plate alternate parallel strokes of B. fluorescens [Pseudomonas fluorescens] and Staph. pyogenes [Streptococcus pyogenes ]... B. fluorescens grew more quickly... [This] is not a question of overgrowth or crowding out of one by another quicker-growing species, as in a garden where luxuriantly growing weeds kill the delicate plants. Nor is it due to the utilization of the available foodstuff by the more quickly growing organisms, rather there is an antagonism caused by the secretion of specific, easily diffusible substances which are inhibitory to the growth of some species but completely ineffective against others.[16]
In 1895, Vincenzo Tiberio, an Italian physician at the University of Naples, published research about moulds initially found in a water well in Arzano; from his observations, he concluded that these moulds contained soluble substances having antibacterial action.[21][22][23][24]
Two years later, Ernest Duchesne at École du Service de Santé Militaire in Lyon independently discovered the healing properties of a Penicillium glaucum mould, even curing infected guinea pigs of typhoid. He published a dissertation[25][26][27] in 1897 but it was ignored by the Institut Pasteur. Duchesne was himself using a discovery made earlier by Arab stable boys, who used moulds to cure sores on horses. He did not claim that the mould contained any antibacterial substance, only that the mould somehow protected the animals. The penicillin isolated by Fleming does not cure typhoid and so it remains unknown which substance might have been responsible for Duchesne's cure.[a] An Institut Pasteur scientist, Costa Rican Clodomiro Picado Twight, similarly recorded the antibiotic effect of Penicillium in 1923. In these early stages of penicillin research, most species of Penicillium were non-specifically referred to as Penicillium glaucum, so that it is impossible to know the exact species and that it was really penicillin that prevented bacterial growth.[15]
Andre Gratia and Sara Dath at the Free University of Brussels, Belgium, were studying the effects of mould samples on bacteria. In 1924, they found that dead Staphylococcus aureus cultures were contaminated by a mould, a streptomycete. Upon further experimentation, they shows that the mould extract could kill not only S. aureus, but also Pseudomonas aeruginosa, Mycobacterium tuberculosis and Escherichia coli.[28] Gratia called the antibacterial agent as "mycolysate" (killer mould). The next year they found another killer mould that could inhibit anthrax bacterium (B. anthracis). Reporting in Comptes Rendus Des Séances de La Société de Biologie et de Ses Filiales they identified the mould as Penicillium glaucum.[29] But these findings received little attention as the antibacterial agent and its medical value were not fully understood; moreover, Gratia's samples were lost.[28]
The breakthrough discovery[]
Background[]

Penicillin was discovered by a Scottish physician Alexander Fleming in 1928. While working at St Mary's Hospital, London, Fleming was investigating the pattern of variation in S. aureus.[30] He was inspired by the discovery of an Irish physician Joseph Warwick Bigger and his two students C.R. Boland and R.A.Q. O’Meara at the Trinity College, Dublin, Ireland, in 1927. Bigger and his students found that when they cultured a particular strain of S. aureus, which they designated "Y" that they isolated a year before from a pus of axillary abscess from one individual, the bacterium grew into a variety of strains. They published their discovery as “Variant colonies of Staphylococcus aureus” in The Journal of Pathology and Bacteriology, by concluding:
We were surprised and rather disturbed to find, on a number of plates, various types of colonies which differed completely from the typical aureus colony. Some of these were quite white; some, either white or of the usual colour were rough on the surface and with crenated margins.[31]
Fleming and his research scholar Daniel Merlin Pryce pursued this experiment but Pryce was transferred to another laboratory in early 1928. After a few months of working alone, a new scholar Stuart Craddock joined Fleming. Their experiment was successful and Fleming was planning and agreed to write a report in A System of Bacteriology to be published by the Medical Research Council by the end of 1928.[30]
Initial discovery[]
In August, Fleming spent a vacation with his family at his country home The Dhoon at Barton Mills, Suffolk. Before leaving his laboratory, he inoculated several culture plates with S. aureus. He kept the plates aside on one corner of the table away from direct sunlight and to make space for Craddock to work in his absence. While in a vacation, he was appointed Professor of Bacteriology at the St Mary's Hospital Medical School on 1 September 1928. He arrived at his laboratory on 3 September, where Pryce was waiting to greet him.[32] As he and Pryce examined the culture plates, they found one with an open lid and the culture contaminated with a blue-green mould. In the contaminated plate the bacteria around the mould did not grow, while those farther away grew normally, meaning that the mould killed the bacteria.[33] Fleming commented as he watched the plate: "That's funny".[32][34] Pryce remarked to Fleming: "That's how you discovered lysozyme."[35]
Experiment[]

Fleming went off to resume his vacation and returned for the experiments late in September.[30] He collected the original mould and grew them in culture plates. After four days he found that the plates developed large colonies of the mould. He repeated the experiment with the same bacteria-killing results. He later recounted his experience:
When I woke up just after dawn on September 28, 1928, I certainly didn't plan to revolutionize all medicine by discovering the world's first antibiotic, or bacteria killer. But I suppose that was exactly what I did.[36]
He concluded that the mould was releasing a substance that was inhibiting bacterial growth, and he produced culture broth of the mould and subsequently concentrated the antibacterial component.[37] After testing against different bacteria, he found that the mould could kill only specific bacteria. For example, Staphylococcus, Streptococcus, and diphtheria bacillus (Corynebacterium diphtheriae) were easily killed; but there was no effect on typhoid bacterium (Salmonella typhimurium) and influenza bacillus (Haemophilus influenzae). He prepared large-culture method from which he could obtained large amounts of the mould juice. He called this juice "penicillin", as he explained the reason as "to avoid the repetition of the rather cumbersome phrase 'Mould broth filtrate,' the name 'penicillin' will be used."[38] He invented the name on 7 March 1929.[32] He later (in his Nobel lecture) gave a further explanation, saying:
I have been frequently asked why I invented the name "Penicillin". I simply followed perfectly orthodox lines and coined a word which explained that the substance penicillin was derived from a plant of the genus Penicillium just as many years ago the word "Digitalin" was invented for a substance derived from the plant Digitalis.[39]
Fleming had no training in chemistry so that he left all the chemical works to Craddock – he once remarked, "I am a bacteriologist, not a chemist."[30] In January 1929, he recruited Frederick Ridley, his former research scholar who had studied biochemistry, specifically to the study the chemical properties of the mould.[34] But they could not isolate penicillin and before the experiments were over, Craddock and Ridley both left Fleming for other jobs.[32] It was due to their failure to isolate the compound that Fleming practically abandoned further research on the chemical aspects of penicillin,[40] although he did biological tests up to 1939.[32]
Identification of the mould[]

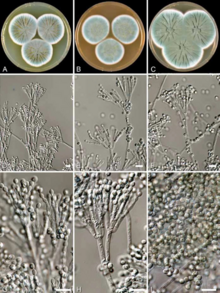
After structural comparison with different species of Penicillium, Fleming initially believed that his specimen was Penicillium chrysogenum, a species described by an American microbiologist Charles Thom in 1910. He was fortunate as Charles John Patrick La Touche, an Irish botanist, had just recently joined as a mycologist at St Mary's to investigate fungi as the cause of asthma. La Touche identified the specimen as Penicillium rubrum,[41][42] the identification used by Fleming in his publication.
In 1931, Thom re-examined different Penicillium including that of Fleming's specimen. He came to a confusing conclusion, stating, "Ad. 35 [Fleming's specimen] is P. notatum WESTLING. This is a member of the P. chrysogenum series with smaller conidia than P. chrysogenum itself."[43] P. notatum was described by Swedish chemist Richard Westling in 1811. From then on, Fleming's mould was synonymously referred to as P. notatum and P. chrysogenum. But Thom adopted and popularised the use of P. chrysogenum.[44] In addition to P. notatum, newly discovered species such as P. meleagrinum and P. cyaneofulvum were recognised as members of P. chrysogenum in 1977.[45] To resolve the confusion, the Seventeenth International Botanical Congress held in Vienna, Austria, in 2005 formally adopted the name P. chrysogenum as the conserved name (nomen conservandum).[46] Whole genome sequence and phylogenetic analysis in 2011 revealed that Fleming's mould belongs to P. rubens, a species described by Belgian microbiologist Philibert Biourge in 1923, and also that P. chrysogenum is a different species.[4][47]
The source of the fungal contamination in Fleming's experiment remained a speculation for several decades. Fleming himself suggested in 1945 that the fungal spores came through the window facing Praed Street. This story was regarded as a fact and was popularised in literature,[48] starting with George Lacken's 1945 book The Story of Penicillin.[32] But it was later disputed by his co-workers including Pryce, who testified much later that Fleming's laboratory window was kept shut all the time.[49] Ronald Hare also agreed in 1970 that the window was most often locked because it was difficult to reach due to a large table with apparatuses placed in front of it. In 1966, La Touche told Hare that he had given Fleming 13 specimens of fungi (10 from his lab) and only one from his lab was showing penicillin-like antibacterial activity.[48] It was from this point a consensus was made that Fleming's mould came from La Touche's lab, which was a floor below in the building, the spores being drifted in the air through the open doors.[50]
Reception and publication[]
Fleming's discovery was not regarded initially as an important discovery. Even as he showed his culture plates to his colleagues, all he received was an indifferent response. He described the discovery on 13 February 1929 before the Medical Research Club. His presentation titled "A medium for the isolation of Pfeiffer's bacillus" did not receive any particular attention.[30]
In 1929, Fleming reported his findings to the British Journal of Experimental Pathology on 10 May 1929, and was published in the next month issue.[51][8] It failed to attract any serious attention. Fleming himself was quite unsure of the medical application and was more concerned on the application for bacterial isolation, as he concluded:
In addition to its possible use in the treatment of bacterial infections penicillin is certainly useful to the bacteriologist for its power of inhibiting unwanted microbes in bacterial cultures so that penicillin insensitive bacteria can readily be isolated. A notable instance of this is the very easy, isolation of Pfeiffers bacillus of influenza when penicillin is used...It is suggested that it may be an efficient antiseptic for application to, or injection into, areas infected with penicillin-sensitive microbes.[51]
G. E. Breen, a fellow member of the Chelsea Arts Club, once asked Fleming, "I just wanted you to tell me whether you think it will ever be possible to make practical use of the stuff [penicillin]. For instance, could I use it?" Fleming gazed vacantly for a moment and then replied, "I don't know. It's too unstable. It will have to be purified, and I can't do that by myself."[30] Even as late as in 1941, the British Medical Journal reported that "the main facts emerging from a very comprehensive study [of penicillin] in which a large team of workers is engaged... does not appear to have been considered as possibly useful from any other point of view."[52][53][b]
Isolation[]
In 1939, Ernst Boris Chain, a German (later naturalised British) chemist, joined the Sir William Dunn School of Pathology at the University of Oxford to investigate on antibiotics. He was immediately impressed by Fleming's 1929 paper, and informed his supervisor, the Australian scientist Howard Florey (later Baron Florey), of the potential drug.[54] By then Florey had acquired a research grant of $25,000 from the Rockefeller Foundation for studying antibiotics.[55] He assembled a research team including Edward Abraham, Arthur Duncan Gardner, Norman Heatley, Margaret Jennings, J. Orr-Ewing and G. Sanders in addition to Chain.[56][57]
The Oxford team prepared a concentrated extract of P. rubens as "a brown powder" that "has been obtained which is freely soluble in water".[58] They found that the powder was not only effective in vitro against bacterial cultures but also and in vivo against bacterial infection in mice. On 5 May 1939, they injected a group of eight mice with a virulent strain of S. aureus, and then injected four of them with the penicillin solution. After one day, all the untreated mice died while the penicillin-treated mice survived. Chain remarked it as "a miracle."[54] They published their findings in The Lancet in 1940.[58]
The team reported details of the isolation method in 1941 with a scheme for large-scale extraction. They also found that penicillin was most abundant as yellow concentrate from the mould extract.[59] But they were able to produce only small quantities. By the early 1942, they could prepare highly purified compound,[60] and worked the chemical formula as C24H32O10N2Ba.[61] In the mid-1942, Chain, Abraham and E. R. Holiday reported the production of the pure compound.[62]
First medical use[]
Fleming performed the first clinical trial with penicillin on Craddock. Craddock had developed severe infection of the nasal antrum (sinusitis) and had undergone surgery. Fleming made use of the surgical opening of the nasal passage and started injecting penicillin on 9 January 1929 but without any effect. It probably was due to the fact that the infection was with influenza bacillus (Haemophilus influenzae), the bacterium which he had found unsusceptible to penicillin.[63] Fleming gave some of his original penicillin samples to his colleague-surgeon Arthur Dickson Wright for clinical test in 1928.[64][65] Although Wright reportedly said that it "seemed to work satisfactorily,"[66] there are no records of its specific use.
Cecil George Paine, a pathologist at the Royal Infirmary in Sheffield, was the first to successfully use penicillin for medical treatment.[67] He was a former student of Fleming and when he learned of the discovery, asked the penicillin sample from Fleming.[68] He initially attempted to treat sycosis (eruptions in beard follicles) with penicillin but was unsuccessful, probably because the drug did not penetrate deep enough. Moving on to ophthalmia neonatorum, a gonococcal infection in babies, he achieved the first cure on 25 November 1930, four patients (one adult, the others infants) with eye infections.[69][70]
Florey's team at Oxford showed that Penicillium extract killed different bacteria (Streptococcus pyogenes, Staphylococcus aureus, and Clostridium septique) in culture and effectively cured Streptococcus infection in mice.[54] They reported in the 24 August 1940 issue of The Lancet as "Penicillin as a chemotherapeutic agent" with a conclusion:
The results are clear cut, and show that penicillin is active in vivo against at least three of the organisms inhibited in vitro. It would seem a reasonable hope that all organisms in high dilution in vitro will be found to be dealt with in vivo. Penicillin does not appear to be related to any chemotherapeutic substance at present in use and is particularly remarkable for its activity against the anaerobic organisms associated with gas gangrene.[58]
In 1941, the Oxford team treated a policeman, Albert Alexander, with a severe face infection; his condition improved, but then supplies of penicillin ran out and he died. Subsequently, several other patients were treated successfully.[71] In December 1942, survivors of the Cocoanut Grove fire in Boston were the first burn patients to be successfully treated with penicillin.[72]
The most important clinical test was in August 1942 when Fleming cured Harry Lambert of an otherwise-fatal infection of the nervous system (streptococcal meningitis). Lambert was a work associate of Robert, Fleming's brother, who had requested Fleming for medical treatment.[73] Fleming asked Florey for the purified penicillin sample, which Fleming immediately used to inject into Lambert's spinal canal. Lambert showed signs of improvement the very next day,[74] and completely recovered within a week.[75][76] Fleming reported his clinical trial in The Lancet in 1943.[77] It was upon this medical evidence that the British War Cabinet set up the Penicillin Committee on 5 April 1943. The committee consisted of Cecil Weir, Director General of Equipment, as Chairman, Fleming, Florey, Sir Percival Hartley, Allison and representatives from pharmaceutical companies as members.[74] This led to mass production of penicillin by the next year.[78][79]
Mass production[]
Knowing that large-scale production for medical use was futile in a confined laboratory, the Oxford team tried to convince war-torn British government and private companies for mass production but in vain.[80] Florey and Heatley travelled to the US in June 1941 to persuade US government and pharmaceutical companies there.[81] Knowing that keeping the mould sample in vials could be easily lost, they instead smeared their coat pockets with the mould.[54] They arrived in Washington D.C. in early July to discuss with Ross Granville Harrison, chairman of the National Research Council (NRC), and Charles Thom and Percy Wells of the United States Department of Agriculture. They were directed to approach the USDA Northern Regional Research Laboratory (NRRL, now the National Center for Agricultural Utilization Research) where large-scale fermentations were done.[82] They reached Peoria, Illinois, on 14 July to meet Andrew Jackson Moyer and Robert D. Coghill at the NRRL. The Americans quickly worked on the mould and were able to make culture by the end of July.[80] But they realised that Fleming's mould was not efficient enough to produce large quantities of penicillin.
NRRL mycologist Kenneth Bryan Raper got the help of US Army Transport Command to search for similar mould in different parts of the world and the best moulds were found to be those from Chungkin (China), Bombay (Mumbai, India) and Cape Town (South Africa). But the single-best sample was from cantaloupe (a type of melon) sold in Peoria fruit market in 1943. The mould was identified as P. chrysogenum and designated as NRRL 1951 or cantaloupe strain.[82] There is a popular story that Mary K. Hunt (or Mary Hunt Stevens[83]), a staff member of Raper, collected the mould;[84] for which she had been popularised as "Mouldy Mary."[85][86] But Raper remarked this story as a "folklore" and that the fruit was delivered to the lab by a woman from the Peoria fruit market.[82]
Between 1941 and 1943, Moyer, Coghill and Kenneth Raper developed methods for industrialized penicillin production and isolated higher-yielding strains of the Penicillium fungus.[87] Simultaneous research by Jasper H. Kane and other Pfizer scientists in Brooklyn developed the practical, deep-tank fermentation method for production of large quantities of pharmaceutical-grade penicillin.[88]

When production first began, one-liter containers had a yield of less than 1%, but improved to a yield of 80–90% in 10,000 gallon containers. This increase in efficiency happened between 1939 and 1945 as the result of continuous process innovation. Orvill May, the director of the Agricultural Research Service, had Robert Coghill, who was the chief of the fermentation division, use his experience with fermentation to increase the efficiency of extracting penicillin from the mould. Shorty after beginning, Moyer replaced sucrose with lactose in the growth media, which resulted in an increased yield. An even larger increase occurred when Moyer added corn steep liquor.[81]
One major issue with the process that scientists faced was the inefficiency of growing the mould on the surface of their nutrient baths, rather than having it submerged. Even though a submerged process of growing the mould would be more efficient, the strain used was not suitable for the conditions it would require. This led NRRL to a search for a strain that had already been adapted to work, and one was found in a mouldy cantaloupe acquired from a Peoria farmers' market.[89] To improve upon that strain, researchers subjected it to X-rays to facilitate mutations in its genome and managed to increase production capabilities even more.[90][89]
Now that scientists had a mould that grew well submerged and produced an acceptable amount of penicillin, the next challenge was to provide the required air to the mould for it to grow. This was solved using an aerator, but aeration caused severe foaming as a result of the corn steep. The foaming problem was solved by the introduction of an anti-foaming agent known as glyceryl monoricinoleate.[90]
Chemical analysis[]
The chemical structure of penicillin was first proposed by Edward Abraham in 1942.[91] Dorothy Hodgkin determined the correct chemical structure of penicillin using X-ray crystallography at Oxford in 1945.[92][93][94][7] In 1945, the US Committee on Medical Research and the British Medical Research Council jointly published in Science a chemical analyses done at different universities, pharmaceutical companies and government research departments. The report announced the existence of different forms of penicillin compounds which all shared the same structural component called β-lactam.[95] The penicillins were given various names such as using Roman numerals in UK (such as penicillin I, II, III) in order their discoveries and letters (such as F, G, K, and X) referring to their origins or sources, as below:
| UK nomenclature | US nomenclature | Chemical name |
|---|---|---|
| Penicillin I | Penicillin F | 2-Pentenylpenicillin |
| Penicillin II | Penicillin G | Benzylpenicillin |
| Penicillin III | Penicillin X | p-Hydroxybenzylpenicillin |
| Penicillin IV | Penicillin K | n-Heptylpenicillin |
The chemical names were based on the side chains of the compounds. To avoid the controversial names, Chain introduced in 1948 the chemical names as standard nomenclature, remarking as: "To make the nomenclature as far as possible unambiguous it was decided to replace the system of numbers or letters by prefixes indicating the chemical nature of the side chain R."[96]
In Kundl, Tyrol, Austria, in 1952, Hans Margreiter and Ernst Brandl of Biochemie (now Sandoz) developed the first acid-stable penicillin for oral administration, penicillin V.[97] American chemist John C. Sheehan at the Massachusetts Institute of Technology (MIT) completed the first chemical synthesis of penicillin in 1957.[98][99][100] Sheehan had started his studies into penicillin synthesis in 1948, and during these investigations developed new methods for the synthesis of peptides, as well as new protecting groups—groups that mask the reactivity of certain functional groups.[100][101] Although the initial synthesis developed by Sheehan was not appropriate for mass production of penicillins, one of the intermediate compounds in Sheehan's synthesis was 6-aminopenicillanic acid (6-APA), the nucleus of penicillin.[102][103]
An important development was the discovery of 6-APA itself. In 1957, researchers at the Beecham Research Laboratories (now the Beechem Group) in Surrey isolated 6-APA from the culture media of P. chrysogenum. 6-APA was found to constitute the core 'nucleus' of penicillin (in fact, all β-lactam antibiotics) and was easily chemically modified by attaching side chains through chemical reactions.[104][105] The discovery was published Nature in 1959).[106] This paved the way for new and improved drugs as all semi-synthetic penicillins are produced from chemical manipulation of 6-APA.[107]
The second-generation semi-synthetic β-lactam antibiotic methicillin, designed to counter first-generation-resistant penicillinases, was introduced in the United Kingdom in 1959. Methicillin-resistant forms of Staphylococcus aureus likely already existed at the time.[7][108]
Outcomes[]
Fleming, Florey and Chain equally shared the 1945 Nobel Prize in Physiology or Medicine "for the discovery of penicillin and its curative effect in various infectious diseases."[6]
Methods for production and isolation of penicillin were patented by Andrew Jackson Moyer in US in 1945.[109][110][111] Chain had wanted to file a patent, Florey and his teammates objected to it arguing that it should be a benefit for all.[54] Sir Henry Dale specifically advised that doing so would be unethical.[71] When Fleming learned of the American patents on penicillin production, he was infuriated and commented:
I found penicillin and have given it free for the benefit of humanity. Why should it become a profit-making monopoly of manufacturers in another country?[74]
Dorothy Hodgkin received the 1964 Nobel Prize in Chemistry "for her determinations by X-ray techniques of the structures of important biochemical substances."
Development of penicillin-derivatives[]
The narrow range of treatable diseases or "spectrum of activity" of the penicillins, along with the poor activity of the orally active phenoxymethylpenicillin, led to the search for derivatives of penicillin that could treat a wider range of infections. The isolation of 6-APA, the nucleus of penicillin, allowed for the preparation of semisynthetic penicillins, with various improvements over benzylpenicillin (bioavailability, spectrum, stability, tolerance). The first major development was ampicillin in 1961. It was produced by Beecham Research Laboratories in London.[112] It was more advantageous than the original penicillin as it offered a broader spectrum of activity against Gram-positive and Gram-negative bacteria.[112] Further development yielded β-lactamase-resistant penicillins, including flucloxacillin, dicloxacillin, and methicillin. These were significant for their activity against β-lactamase-producing bacterial species, but were ineffective against the methicillin-resistant Staphylococcus aureus (MRSA) strains that subsequently emerged.[113]
Another development of the line of true penicillins was the antipseudomonal penicillins, such as carbenicillin, ticarcillin, and piperacillin, useful for their activity against Gram-negative bacteria. However, the usefulness of the β-lactam ring was such that related antibiotics, including the mecillinams, the carbapenems and, most important, the cephalosporins, still retain it at the center of their structures.[105][114]
The penicillins related β-lactams have become the most widely used antibiotics in the world.[115] Amoxicillin, a semisynthetic penicillin developed by Beecham Research Laboratories in 1970,[116][117] is the most commonly used of all.[118][119]
Drug resistance[]
Fleming warned the possibility of penicillin resistance in clinical conditions in his Nobel Lecture, and said:
The time may come when penicillin can be bought by anyone in the shops. Then there is the danger that the ignorant man may easily underdose himself and by exposing his microbes to non-lethal quantities of the drug make them resistant.[120]
In 1940, Ernst Chain and Edward Abraham reported the first indication of antibiotic resistance to penicillin, an E. coli strain that produced the penicillinase enzyme, which was capable of breaking down penicillin and completely negating its antibacterial effect.[7][8][121] Chain and Abraham worked out the chemical nature of penicillinase which they reported in Nature as:
The conclusion that the active substance is an enzyme is drawn from the fact that it is destroyed by heating at 90° for 5 minutes and by incubation with papain activated with potassium cyanide at pH 6, and that it is non-dialysable through 'Cellophane' membranes.[122]
In 1942, strains of Staphylococcus aureus had been documented to have developed a strong resistance to penicillin. Most of the strains were resistant to penicillin by the 1960s.[123] In 1967, Streptococcus pneumoniae was also reported to be penicillin resistant. Many strains of bacteria have eventually developed a resistance to penicillin.
Notes[]
- ^ At the time, the term Penicillium glaucum was used as a catch-all phrase for a variety of different fungi, though not for Penicillium notatum. Duchesne's specific mold was unfortunately not preserved, which makes it impossible to be certain today which fungus might have been responsible for the cure and, consequently, even less certain which specific antibacterial substance was responsible.
- ^ The statement "does not appear to have been considered as possibly useful from any other point of view" seems to be later deleted, but is still apparent from Fleming's response (BMJ, 2 (4210): 386–386).
References[]
- ^ "Alexander Fleming". Science History Institute. June 2016. Retrieved 21 August 2018.
- ^ Jump up to: a b "Discovery and Development of Penicillin". International Historic Chemical Landmarks. American Chemical Society. Retrieved 21 August 2018.
- ^ Macfarlane G (1984). Alexander Fleming : the man and the myth. Cambridge, Mass.: Harvard University Press. ISBN 978-0-19-281884-3. OCLC 11519742.
- ^ Jump up to: a b Houbraken J, Frisvad JC, Samson RA (June 2011). "Fleming's penicillin producing strain is not Penicillium chrysogenum but P. rubens". IMA Fungus. 2 (1): 87–95. doi:10.5598/imafungus.2011.02.01.12. PMC 3317369. PMID 22679592.
- ^ Barreiro C, Martín JF, García-Estrada C (2012). "Proteomics shows new faces for the old penicillin producer Penicillium chrysogenum". Journal of Biomedicine & Biotechnology. 2012: 105109. doi:10.1155/2012/105109. PMC 3270403. PMID 22318718.
- ^ Jump up to: a b "The Nobel Prize in Physiology or Medicine 1945". NobelPrize.org. Retrieved 26 July 2020.
- ^ Jump up to: a b c d Davies J, Davies D (September 2010). "Origins and evolution of antibiotic resistance". Microbiology and Molecular Biology Reviews. 74 (3): 417–33. doi:10.1128/MMBR.00016-10. PMC 2937522. PMID 20805405.
- ^ Jump up to: a b c Lobanovska M, Pilla G (March 2017). "Penicillin's Discovery and Antibiotic Resistance: Lessons for the Future?". The Yale Journal of Biology and Medicine. 90 (1): 135–145. PMC 5369031. PMID 28356901.
- ^ "History of Antibiotics | Steps of the Scientific Method, Research and Experiments". Experiment-Resources.com. Archived from the original on 6 August 2011. Retrieved 13 July 2012.
- ^ Nowak A, Nowak MJ, Cybulska K (December 2017). "Stories with microorganisms…". Chemistry-Didactics-Ecology-Metrology. 22 (1–2): 59–68. doi:10.1515/cdem-2017-0003. S2CID 90736968.
- ^ MacFarlane G (1979). Howard Florey : the making of a great scientist. Oxford: Oxford Univ. Pr. pp. 14–15. ISBN 978-0198581611.
- ^ Allchin D. "Penicillin & Chance". SHiPS Resource Center. Archived from the original on 28 May 2009. Retrieved 9 February 2010.
- ^ Koch, Robert (2010) [1876]. Robert Koch-Institut. "Die Ätiologie der Milzbrand-Krankheit, begründet auf die Entwicklungsgeschichte des Bacillus Anthracis" [The Etiology of Anthrax Disease, Based on the Developmental History of Bacillus Anthracis]. Cohns Beiträge zur Biologie der Pflanzen (in German). 2 (2): 277 (1–22). doi:10.25646/5064.
- ^ Lakhtakia, Ritu (2014). "The Legacy of Robert Koch: Surmise, search, substantiate". Sultan Qaboos University Medical Journal. 14 (1): e37–41. doi:10.12816/0003334. PMC 3916274. PMID 24516751.
- ^ Jump up to: a b Shama G (September 2016). "La Moisissure et la Bactérie: Deconstructing the fable of the discovery of penicillin by Ernest Duchesne". Endeavour. 40 (3): 188–200. doi:10.1016/j.endeavour.2016.07.005. PMID 27496372.
- ^ Jump up to: a b Florey, Howard W. (1946). "The Use of Micro-organisms for Therapeutic Purposes". The Yale Journal of Biology and Medicine. 19 (1): 101–118.1. PMC 2602034. PMID 20275724.
- ^ Foster, W.; Raoult, A. (1974). "Early descriptions of antibiosis". The Journal of the Royal College of General Practitioners. 24 (149): 889–894. PMC 2157443. PMID 4618289.
- ^ Jump up to: a b Brunel, J. (1951). "Antibiosis from Pasteur to Fleming". Journal of the History of Medicine and Allied Sciences. 6 (3): 287–301. doi:10.1093/jhmas/vi.summer.287. PMID 14873929.
- ^ Waksman, S. A. (1947). "What is an antibiotic or an antibiotic substance?". Mycologia. 39 (5): 565–569. doi:10.1080/00275514.1947.12017635. PMID 20264541.
- ^ Kruif, Paul De (1996) [1926]. Microbe Hunters. Florida (USA): Houghton Mifflin Harcourt. p. 144. ISBN 978-0-15-602777-9.
At once Pasteur jumped to a fine idea: "If the harmless bugs from the air choke out the anthrax bacilli in the bottle, they will do it in the body too! It is a kind of dog-eat-dog!” shouted Pasteur, (...) Pasteur gravely announced: "That there were high hopes for the cure of disease from this experiment", but that is the last you hear of it, for Pasteur was never a man to give the world of science the benefit of studying his failures.
- ^ Tiberio, Vincenzo (1895) "Sugli estratti di alcune muffe" [On the extracts of certain moulds], Annali d'Igiene Sperimentale (Annals of Experimental Hygiene), 2nd series, 5 : 91–103. From p. 95: "Risulta chiaro da queste osservazioni che nella sostanza cellulare delle muffe esaminate son contenuti dei principi solubili in acqua, forniti di azione battericida: sotto questo riguardo sono più attivi o in maggior copia quelli dell' Asp. flavescens, meno quelli del Mu. mucedo e del Penn. glaucum." (It follows clearly from these observations that in the cellular substance of the moulds examined are contained some water-soluble substances, provided with bactericidal action: in this respect are more active or in greater abundance those of Aspergillus flavescens; less, those of Mucor mucedo and Penicillium glaucum.)
- ^ Bucci R., Galli P. (2011) "Vincenzo Tiberio: a misunderstood researcher," Italian Journal of Public Health, 8 (4) : 404–406. (Accessed 1 May 2015)
- ^ "Almanacco della Scienza CNR". Almanacco.rm.cnr.it. 2 March 2011. Retrieved 13 July 2012.
- ^ De Rosa S. "Vincenzo Tiberio, vero scopritore degli antibiotici – Festival della Scienza" (in Italian). Festival2011.festivalscienza.it. Retrieved 13 July 2012.
- ^ Duchesne E (2013). Antagonism between moulds and bacteria. An English translation by Michael Witty. Fort Myers. ASIN B00E0KRZ0E.
- ^ Duchesne E (1897). Contribution à l'étude de la concurrence vitale chez les micro-organismes : antagonisme entre les moisissures et les microbes [Contribution to the study of the vital competition in microorganisms: antagonism between moulds and microbes] (in French). Lyon, France: Alexandre Rey.
- ^ Pouillard J. "Une découverte oubliée : la thèse de médecine du docteur Ernest Duchesne (1874–1912)" [A Forgotten Discovery : Doctor of Medicine Ernest Duchesne's Thesis (1874-1912).] (PDF). Histoire des Sciences Médicales (in French). XXXVI (1): 11–20. Archived from the original (PDF) on 13 July 2019.
- ^ Jump up to: a b Wainwright, Milton (2000). "André Gratia (1893–1950): Forgotten Pioneer of Research into Antimicrobial Agents". Journal of Medical Biography. 8 (1): 39–42. doi:10.1177/096777200000800108. PMID 11608911. S2CID 43285911.
- ^ de Scoville, C; Brouwer, C De; Dujardin, M (1999). "Nobel chronicle: Fleming and Gratia". The Lancet. 354 (9174): 258. doi:10.1016/S0140-6736(05)66334-9. PMID 10421340. S2CID 11659394.
- ^ Jump up to: a b c d e f Lalchhandama K (2020). "Reappraising Fleming's snot and mould". Science Vision. 20 (1): 29–42. doi:10.33493/scivis.20.01.03.
- ^ Bigger JW, Boland CR, O'Meara RA (1927). "Variant colonies of Staphylococcus aureus". The Journal of Pathology and Bacteriology. 30 (2): 261–269. doi:10.1002/path.1700300204.
- ^ Jump up to: a b c d e f Diggins FW (1999). "The true history of the discovery of penicillin, with refutation of the misinformation in the literature". British Journal of Biomedical Science. 56 (2): 83–93. PMID 10695047.
- ^ Wainwright M (February 1993). "The mystery of the plate: Fleming's discovery and contribution to the early development of penicillin". Journal of Medical Biography. 1 (1): 59–65. doi:10.1177/096777209300100113. PMID 11639213. S2CID 7578843.
- ^ Jump up to: a b Wainwright M (February 1993). "The mystery of the plate: Fleming's discovery and contribution to the early development of penicillin". Journal of Medical Biography. 1 (1): 59–65. doi:10.1177/096777209300100113. PMID 11639213. S2CID 7578843.
- ^ Gupta N, Rodrigues C, Soman R (September 2015). "Pioneers in Antimicrobial Chemotherapy". The Journal of the Association of Physicians of India. 63 (9): 90–1. PMID 27608881.
- ^ Tan SY, Tatsumura Y (July 2015). "Alexander Fleming (1881-1955): Discoverer of penicillin". Singapore Medical Journal. 56 (7): 366–7. doi:10.11622/smedj.2015105. PMC 4520913. PMID 26243971.
- ^ Arseculeratne SN, Arseculeratne G (May 2017). "A re-appraisal of the conventional history of antibiosis and Penicillin". Mycoses. 60 (5): 343–347. doi:10.1111/myc.12599. PMID 28144986. S2CID 21424547.
- ^ Fleming, Alexander (1929). "On the antibacterial action of cultures of a Penicillium, with special reference to their use in the isolation of B. influenzae". British Journal of Experimental Pathology. 10 (3): 226–236. PMC 2041430. PMID 2048009.; Reprinted as Fleming A (1979). "On the antibacterial action of cultures of a Penicillium, with special reference to their use in the isolation of B. influenzae". British Journal of Experimental Pathology. 60 (1): 3–13. PMC 2041430.
- ^ Fleming A (1945). "Nobel Lecture". www.nobelprize.org. Retrieved 19 July 2020.
- ^ Hess K (2019). "Fleming vs. Florey: It All Comes Down to the Mold". The Histories. 2 (1): 3–10.
- ^ Henderson JW (July 1997). "The yellow brick road to penicillin: a story of serendipity". Mayo Clinic Proceedings. 72 (7): 683–7. doi:10.4065/72.7.683. PMID 9212774.
- ^ Kingston W (June 2008). "Irish contributions to the origins of antibiotics". Irish Journal of Medical Science. 177 (2): 87–92. doi:10.1007/s11845-008-0139-x. PMID 18347757. S2CID 32847260.
- ^ Thom C (1931). "Appendix. History of species used and Dr. Thom's diagnoses of species". Philosophical Transactions of the Royal Society of London. Series B, Containing Papers of a Biological Character. 220 (468–473): 83–92. doi:10.1098/rstb.1931.0015.
- ^ Thom C (1945). "Mycology Presents Penicillin". Mycologia. 37 (4): 460–475. doi:10.2307/3754632. JSTOR 3754632.
- ^ Samson RA, Hadlok R, Stolk AC (1977). "A taxonomic study of the Penicillium chrysogenum series". Antonie van Leeuwenhoek. 43 (2): 169–75. doi:10.1007/BF00395671. PMID 413477. S2CID 41843432.
- ^ "International Code of Botanical Nomenclature (VIENNA CODE). Appendix IV Nomina specifica conservanda et rejicienda. B. Fungi". International Association of Plant Taxonomy. 2006. Retrieved 17 June 2020.
- ^ Houbraken J, Frisvad JC, Seifert KA, Overy DP, Tuthill DM, Valdez JG, Samson RA (December 2012). "New penicillin-producing Penicillium species and an overview of section Chrysogena". Persoonia. 29 (1): 78–100. doi:10.3767/003158512X660571. PMC 3589797. PMID 23606767.
- ^ Jump up to: a b Hare R (January 1982). "New light on the history of penicillin". Medical History. 26 (1): 1–24. doi:10.1017/S0025727300040758. PMC 1139110. PMID 7047933.
- ^ Wyn Jones E, Wyn Jones RG (December 2002). "Merlin Pryce (1902-1976) and penicillin: an abiding mystery". Vesalius. 8 (2): 6–25. PMID 12713008.
- ^ Curry J (1981). "Obituary: C. J. La Touche". Medical Mycology. 19 (2): 164. doi:10.1080/00362178185380261.
- ^ Jump up to: a b Fleming, Alexander (1929). "On the antibacterial action of cultures of a Penicillium, with special reference to their use in the isolation of B. influenzae". British Journal of Experimental Pathology. 10 (3): 226–236. PMC 2041430. PMID 2048009.; Reprint of Fleming A (1979). "On the antibacterial action of cultures of a Penicillium, with special reference to their use in the isolation of B. influenzae". British Journal of Experimental Pathology. 60 (1): 3–13. PMC 2041430.
- ^ "Annotations". British Medical Journal. 2 (4208): 310–2. August 1941. doi:10.1136/bmj.2.4208.310. PMC 2162429. PMID 20783842.
- ^ Fleming A (September 1941). "Penicillin". British Medical Journal. 2 (4210): 386. doi:10.1136/bmj.2.4210.386. PMC 2162878.
- ^ Jump up to: a b c d e Gaynes, Robert (2017). "The Discovery of Penicillin—New Insights After More Than 75 Years of Clinical Use". Emerging Infectious Diseases. 23 (5): 849–853. doi:10.3201/eid2305.161556. PMC 5403050.
- ^ Kong, Kok-Fai; Schneper, Lisa; Mathee, Kalai (2010). "Beta-lactam antibiotics: from antibiosis to resistance and bacteriology". Acta Pathologica, Microbiologica, et Immunologica Scandinavica. 118 (1): 1–36. doi:10.1111/j.1600-0463.2009.02563.x. PMC 2894812. PMID 20041868.
- ^ Jones DS, Jones JH (1 December 2014). "Sir Edward Penley Abraham CBE. 10 June 1913 – 9 May 1999". Biographical Memoirs of Fellows of the Royal Society. 60: 5–22. doi:10.1098/rsbm.2014.0002. ISSN 0080-4606.
- ^ "Ernst B. Chain – Nobel Lecture: The Chemical Structure of the Penicillins". www.nobelprize.org. Retrieved 10 May 2017.
- ^ Jump up to: a b c Chain, E.; Florey, H. W.; Adelaide, M. B.; Gardner, A. D.; Heatley, N. G.; Jennings, M. A.; Orr-Ewing, J.; Sanders, A. G. (1940). "Penicillin as a chemotherapeutic agent". The Lancet. 236 (6104): 226–228. doi:10.1016/S0140-6736(01)08728-1. PMID 8403666.
- ^ Abraham EP, Chain E, Fletcher CM, Florey HW, Gardner AD, Heatley NG, Jennings MA (1941). "Further observations on penicillin. 1941". European Journal of Clinical Pharmacology. 42 (1): 3–9. doi:10.1016/S0140-6736(00)72122-2. PMID 1541313.
- ^ Abraham, E. P.; Chain, E. (1942). "Purification of Penicillin". Nature. 149 (3777): 328. Bibcode:1942Natur.149..328A. doi:10.1038/149328b0. S2CID 4122059.
- ^ Abraham, E. P.; Baker, W.; Chain, E.; Florey, H. W.; Holiday, E. R.; Robinson, R. (1942). "Nitrogenous Character of Penicillin". Nature. 149 (3778): 356. Bibcode:1942Natur.149..356A. doi:10.1038/149356a0. S2CID 4055617.
- ^ Abraham EP, Chain E, Holiday ER (1942). "Purification and Some Physical and Chemical Properties of Penicillin". British Journal of Experimental Pathology. 23 (3): 103–119. PMC 2065494.
- ^ Hare, R. (1982). "New light on the history of penicillin". Medical History. 26 (1): 1–24. doi:10.1017/s0025727300040758. PMC 1139110. PMID 7047933.
- ^ Wainwright, M.; Swan, H.T. (1987). "The Sheffield penicillin story". Mycologist. 1 (1): 28–30. doi:10.1016/S0269-915X(87)80022-8.
- ^ Wainwright, Milton (1990). "Besredka's "antivirus" in relation to Fleming's initial views on the nature of penicillin". Medical History. 34 (1): 79–85. doi:10.1017/S0025727300050286. PMC 1036002. PMID 2405221.
- ^ Wainwright, M (1987). "The history of the therapeutic use of crude penicillin". Medical History. 31 (1): 41–50. doi:10.1017/s0025727300046305. PMC 1139683. PMID 3543562.
- ^ Wainwright, Milton (1989). "Moulds in Folk Medicine". Folklore. 100 (2): 162–166. doi:10.1080/0015587X.1989.9715763.
- ^ "Dr Cecil George Paine - Unsung Medical Heroes - Blackwell's Bookshop Online". blackwells.co.uk. Retrieved 19 October 2020.
- ^ Wainwright M, Swan HT (January 1986). "C.G. Paine and the earliest surviving clinical records of penicillin therapy". Medical History. 30 (1): 42–56. doi:10.1017/S0025727300045026. PMC 1139580. PMID 3511336.
- ^ Alharbi, Sulaiman Ali; Wainwright, Milton; Alahmadi, Tahani Awad; Salleeh, Hashim Bin; Faden, Asmaa A.; Chinnathambi, Arunachalam (2014). "What if Fleming had not discovered penicillin?". Saudi Journal of Biological Sciences. 21 (4): 289–293. doi:10.1016/j.sjbs.2013.12.007. PMC 4150221. PMID 25183937.
- ^ Jump up to: a b "Making Penicillin Possible: Norman Heatley Remembers". ScienceWatch. Thomson Scientific. 2007. Archived from the original on 21 February 2007. Retrieved 13 February 2007.
- ^ Levy SB (2002). The Antibiotic Paradox: How the Misuse of Antibiotics Destroys Their Curative Powers. Da Capo Press. pp. 5–7. ISBN 978-0-7382-0440-6.
- ^ Ligon, B. Lee (2004). "Sir Alexander Fleming: Scottish researcher who discovered penicillin". Seminars in Pediatric Infectious Diseases. 15 (1): 58–64. doi:10.1053/j.spid.2004.02.002. PMID 15175996.
- ^ Jump up to: a b c Allison, V. D. (1974). "Personal recollections of Sir Almroth Wright and Sir Alexander Fleming". The Ulster Medical Journal. 43 (2): 89–98. PMC 2385475. PMID 4612919.
- ^ Bennett, Joan W; Chung, King-Thom (2001), "Alexander Fleming and the discovery of penicillin", Advances in Applied Microbiology, Elsevier, 49: 163–184, doi:10.1016/s0065-2164(01)49013-7, ISBN 978-0-12-002649-4, PMID 11757350, retrieved 17 October 2020
- ^ Cairns, H.; Lewin, W. S.; Duthie, E. S.; Smith, HonorV. (1944). "Pneumococcal Meningitis Treated with Penicillin". The Lancet. 243 (6299): 655–659. doi:10.1016/S0140-6736(00)77085-1.
- ^ Fleming, Alexander (1943). "Streptococcal Meningitis treated With Penicillin". The Lancet. 242 (6267): 434–438. doi:10.1016/S0140-6736(00)87452-8.
- ^ Mathews, John A. (2008). "The Birth of the Biotechnology Era: Penicillin in Australia, 1943–80". Prometheus. 26 (4): 317–333. doi:10.1080/08109020802459306. S2CID 143123783.
- ^ Baldry, Peter (1976). The Battle Against Bacteria: A Fresh Look. CUP Archive. p. 115. ISBN 978-0-521-21268-7.
- ^ Jump up to: a b Andrew Carroll (2 June 2014). "Here is Where: Penicillin Comes to Peoria". HistoryNet. Retrieved 4 January 2021.
- ^ Jump up to: a b "Discovery and Development of Penicillin: International Historic Chemical Landmark". Washington, D.C.: American Chemical Society. Archived from the original on 28 June 2019. Retrieved 15 July 2019.
- ^ Jump up to: a b c Neushul, P. (1993). "Science, government, and the mass production of penicillin". Journal of the History of Medicine and Allied Sciences. 48 (4): 371–395. doi:10.1093/jhmas/48.4.371. PMID 8283024.
- ^ Bentley, Ronald (2009). "Different roads to discovery; Prontosil (hence sulfa drugs) and penicillin (hence β-lactams)". Journal of Industrial Microbiology & Biotechnology. 36 (6): 775–786. doi:10.1007/s10295-009-0553-8. PMID 19283418. S2CID 35432074.
- ^ Kardos, Nelson; Demain, Arnold L. (2011). "Penicillin: the medicine with the greatest impact on therapeutic outcomes". Applied Microbiology and Biotechnology. 92 (4): 677–687. doi:10.1007/s00253-011-3587-6. PMID 21964640. S2CID 39223087.
- ^ Bauze, Robert (1997). "Editorial: Howard Florey and the penicillin story". Journal of Orthopaedic Surgery. Retrieved 4 January 2021.
- ^ Taylor, Robert B. (2016), "Drugs and Other Remedies", White Coat Tales, Cham: Springer International Publishing, pp. 67–84, doi:10.1007/978-3-319-29055-3_3, ISBN 978-3-319-29053-9, retrieved 4 January 2021
- ^ (1) "Penicillium chrysogenum (aka P. notatum), the natural source for the wonder drug penicillin, the first antibiotic". Tom Volk's Fungus of the Month for November 2003.
(2) "Historic Peoria, Illinois". Northern Regional Research Lab. Archived from the original on 6 November 2006. Retrieved 6 June 2007. - ^ "1900–1950". Exploring Our History. Pfizer Inc. 2009. Retrieved 2 August 2009.
- ^ Jump up to: a b Mestrovic T (13 May 2010). "Penicillin Production".
- ^ Jump up to: a b "Alexander Fleming Discovery and Development of Penicillin – Landmark". American Chemical Society. Retrieved 18 March 2019.
- ^ Jones DS, Jones JH (1 December 2014). "Sir Edward Penley Abraham CBE. 10 June 1913 – 9 May 1999". Biographical Memoirs of Fellows of the Royal Society. 60: 5–22. doi:10.1098/rsbm.2014.0002.
- ^ "Penicillin X-ray data showed that proposed β-lactam structure was right". C&EN. Retrieved 21 August 2018.
- ^ Hodgkin DC (July 1949). "The X-ray analysis of the structure of penicillin". Advancement of Science. 6 (22): 85–9. PMID 18134678.
- ^ Curtis R, Jones J (December 2007). "Robert Robinson and penicillin: an unnoticed document in the saga of its structure". Journal of Peptide Science. 13 (12): 769–75. doi:10.1002/psc.888. PMID 17890642. S2CID 11213177.
- ^ Committee on Medical Research; Medical Research Council (1945). "Chemistry of penicillin". Science. 102 (2660): 627–629. Bibcode:1945Sci...102..627M. doi:10.1126/science.102.2660.627. PMID 17788243.
- ^ Chain, E (1948). "The chemistry of penicillin". Annual Review of Biochemistry. 17 (1): 657–704. doi:10.1146/annurev.bi.17.070148.003301. PMID 18893607.
- ^ "Serie Forschung und Industrie: Sandoz". Medical Tribune (in German) (45/2005). Retrieved 2 August 2009.
- ^ Sheehan JC, H enery-Logan KR (5 March 1957). "The Total Synthesis of Penicillin V". Journal of the American Chemical Society. 79 (5): 1262–1263. doi:10.1021/ja01562a063.
- ^ Sheehan JC, Henery-Loganm KR (20 June 1959). "The Total Synthesis of Penicillin V". Journal of the American Chemical Society. 81 (12): 3089–3094. doi:10.1021/ja01521a044.
- ^ Jump up to: a b Corey EJ, Roberts JD. "Biographical Memoirs: John Clark Sheehan". The National Academy Press. Retrieved 28 January 2013.
- ^ Nicolaou KC, Vourloumis D, Winssinger N, Baran PS (January 2000). "The Art and Science of Total Synthesis at the Dawn of the Twenty-First Century". Angewandte Chemie. 39 (1): 44–122. doi:10.1002/(SICI)1521-3773(20000103)39:1<44::AID-ANIE44>3.0.CO;2-L. PMID 10649349.
- ^ Sheehan JC, Logan KR (1959). "A general synthesis of the penicillins". Journal of the American Chemical Society. 81 (21): 5838–5839. doi:10.1021/ja01530a079.
- ^ Sheehan JC, Henery-Logan KR (1962). "The Total and Partial General Syntheses of the Penicillins". Journal of the American Chemical Society. 84 (15): 2983–2990. doi:10.1021/ja00874a029.
- ^ Sheehan JC (1964). "The Synthetic Penicillins". In Schueler FW (ed.). Molecular Modification in Drug Design. Molecular Modification in Drug Design. Advances in Chemistry. 45. Washington, D.C.: American Chemical Society. pp. 15–24. doi:10.1021/ba-1964-0045.ch002. ISBN 978-0-8412-0046-3.
- ^ Jump up to: a b Hamilton-Miller JM (March 2008). "Development of the semi-synthetic penicillins and cephalosporins". International Journal of Antimicrobial Agents. 31 (3): 189–92. doi:10.1016/j.ijantimicag.2007.11.010. PMID 18248798.
- ^ Batchelor, F. R.; Doyle, F. P.; Nayler, J. H.; Rolinson, G. N. (1959). "Synthesis of penicillin: 6-aminopenicillanic acid in penicillin fermentations". Nature. 183 (4656): 257–258. Bibcode:1959Natur.183..257B. doi:10.1038/183257b0. PMID 13622762. S2CID 4268993.
- ^ Rolinson, G. N.; Geddes, A. M. (2007). "The 50th anniversary of the discovery of 6-aminopenicillanic acid (6-APA)". International Journal of Antimicrobial Agents. 29 (1): 3–8. doi:10.1016/j.ijantimicag.2006.09.003. PMID 17137753.
- ^ Harkins CP, Pichon B, Doumith M, Parkhill J, Westh H, Tomasz A, et al. (July 2017). "Methicillin-resistant Staphylococcus aureus emerged long before the introduction of methicillin into clinical practice". Genome Biology. 18 (1): 130. doi:10.1186/s13059-017-1252-9. PMC 5517843. PMID 28724393.
- ^ US 2442141, Moyer AJ, "Method for Production of Penicillin", issued 25 March 1948, assigned to US Agriculture
- ^ US 2443989, Moyer AJ, "Method for Production of Penicillin", issued 22 June 1948, assigned to US Agriculture
- ^ US 2476107, Moyer AJ, "Method for Production of Penicillin", issued 12 July 1949, assigned to US Agriculture
- ^ Jump up to: a b Acred P, Brown DM, Turner DH, Wilson MJ (April 1962). "Pharmacology and chemotherapy of ampicillin--a new broad-spectrum penicillin". British Journal of Pharmacology and Chemotherapy. 18 (2): 356–69. doi:10.1111/j.1476-5381.1962.tb01416.x. PMC 1482127. PMID 13859205.
- ^ Colley EW, Mcnicol MW, Bracken PM (March 1965). "Methicillin-Resistant Staphylococci in a General Hospital". Lancet. 1 (7385): 595–7. doi:10.1016/S0140-6736(65)91165-7. PMID 14250094.
- ^ James CW, Gurk-Turner C (January 2001). "Cross-reactivity of beta-lactam antibiotics". Proceedings. 14 (1): 106–7. doi:10.1080/08998280.2001.11927741. PMC 1291320. PMID 16369597.
- ^ de Sousa Coelho, F.; Mainardi, J.-L. (5 January 2021). "The multiple benefits of second-generation β-lactamase inhibitors in treatment of multidrug-resistant bacteria". Infectious Diseases Now. online. doi:10.1016/j.idnow.2020.11.007. PMID 33870896.
- ^ Croydon, E. A.; Sutherland, R. (1970). "α-amino-p-hydroxybenzylpenicillin (BRL 2333), a new semisynthetic penicillin: absorption and excretion in man". Antimicrobial Agents and Chemotherapy. 10: 427–430. PMID 5521362.
- ^ Sutherland, R.; Rolinson, G. N. (1970). "α-amino-p-hydroxybenzylpenicillin (BRL 2333), a new semisynthetic penicillin: in vitro evaluation". Antimicrobial Agents and Chemotherapy. 10: 411–415. doi:10.1128/AAC.10.3.411. PMC 429762. PMID 5000265.
- ^ Burch, D. G. S.; Sperling, D. (2018). "Amoxicillin-current use in swine medicine". Journal of Veterinary Pharmacology and Therapeutics. 41 (3): 356–368. doi:10.1111/jvp.12482.
- ^ Aberer, Werner; Macy, Eric (2017). "Moving toward optimizing testing for penicillin allergy". The Journal of Allergy and Clinical Immunology. In Practice. 5 (3): 684–685. doi:10.1016/j.jaip.2017.03.020. PMID 28483319.
- ^ Fleming, A. (1945). "The Nobel Prize in Physiology or Medicine 1945 -Penicillin: Nobel Lecture". NobelPrize.org. Retrieved 17 October 2020.
- ^ Abraham EP, Chain E (1940). "An enzyme from bacteria able to destroy penicillin". Nature. 146 (3713): 837. Bibcode:1940Natur.146..837A. doi:10.1038/146837a0. S2CID 4070796.
- ^ Abraham EP, Chain E (1940). "An enzyme from bacteria able to destroy penicillin". Nature. 10 (4): 677–8. Bibcode:1940Natur.146..837A. doi:10.1038/146837a0. PMID 3055168. S2CID 4070796.
- ^ Lowy FD (May 2003). "Antimicrobial resistance: the example of Staphylococcus aureus". The Journal of Clinical Investigation. 111 (9): 1265–73. doi:10.1172/JCI18535. PMC 154455. PMID 12727914.
Further reading[]
- Bud R (2007). Penicillin: Triumph and Tragedy. Oxford: Oxford University Press. ISBN 9780199254064.
- Brown KW (2004). Penicillin man: Alexander Fleming and the antibiotic revolution. Scarborough, Ont: Sutton Pub. ISBN 978-0-7509-3152-6. (St Mary's Trust Archivist and Alexander Fleming Laboratory Museum Curator)
External links[]
- History of Antibiotics, archived from the original on 14 May 2002, retrieved 6 August 2013, from a course offered at Princeton University
- Debate in the House of Commons on the history and the future of the discovery.
- History of pharmacy
- Penicillins
- Microbiology
- History of medicine