Lateral meningocele syndrome
| Lateral meningocele syndrome | |
|---|---|
| Other names | Lehman syndrome[1] |
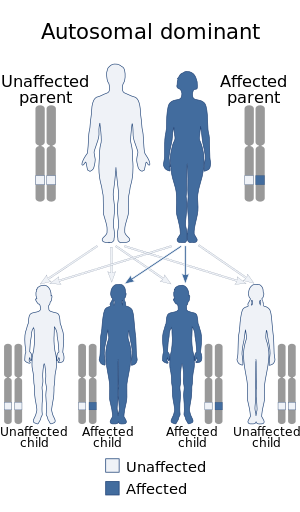 | |
| Lateral meningocele syndrome is inherited in an autosomal dominant manner | |
Lateral meningocele syndrome, also known as Lehman syndrome,[2] is a very rare skeletal disorder with facial anomalies, hypotonia and meningocele-related neurologic dysfunction.[3]
Presentation[]
Facial features found in this syndrome include
- dolichocephaly
- hypertelorism
- ptosis
- high arched palate
- long flat philtrum
- low set ears
Non facial features of this syndrome include
- hypotonia
- lateral meningoceles
- bladder dysfunction and neuropathy
The lateral meningoceles are a common finding in this syndrome. They may be associated with neurological abnormalities and result in and neuropathy. Diagnosis is based on a presentation concurrent with previous clinical reports, as well as a heterozygous pathogenic variant in the NOTCH3 gene.[4]
Genetics[]
This syndrome appears to be inherited in an autosomal dominant fashion; however, X-linked inheritance has not been completely ruled out.[citation needed]
Molecular analyses suggest that the causative mutations cause a truncation of the protein. These mutations result in the loss of PEST sequence in the protein. This loss is associated with a prolonged half life of the protein.[citation needed]
Mutations in Notch 3 were found to be associated with this syndrome.[5]
Treatment[]
Rarely, surgical intervention is required for neurologic manifestations. Some patient benefit from chronic pain management, rehabilitation medicine, and physiotherapy, as well as routine management of "cleft palate, hearing loss, congenital cardiac defects, GU abnormalities, feeding difficulties."[6]
History[]
This syndrome was first described by Lehman et al. in 1977.[7] This paper described a 14-year-old girl with a number of unusual findings. Her mother shared some of the same findings. Since then over a dozen additional cases have been reported.
References[]
- ^ RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Lateral meningocele syndrome". www.orpha.net. Retrieved 20 October 2019.
- ^ RESERVED, INSERM US14-- ALL RIGHTS. "Orphanet: Lehman syndrome". www.orpha.net. Retrieved 2021-04-21.
- ^ Pamir, M. Memet Ö̈zek, Giuseppe Cinalli, Wirginia J. Maixner; forewords by C. Sainte-Rose, C. di Rocco; preface by M. Necmettin, ed. (2008). Spina bifida : management and outcome. Milan: Springer. p. 432. ISBN 9788847006508.
- ^ Ejaz, Resham; Carter, Melissa; Gripp, Karen (1993), Adam, Margaret P.; Ardinger, Holly H.; Pagon, Roberta A.; Wallace, Stephanie E. (eds.), "Lateral Meningocele Syndrome", GeneReviews®, Seattle (WA): University of Washington, Seattle, PMID 27336130, retrieved 2021-04-21
- ^ Gripp, K. W.; Robbins, K. M.; Sobreira, N. L.; Witmer, P. D.; Bird, L. M.; Avela, K; Makitie, O; Alves, D; Hogue, J. S.; Zackai, E. H.; Doheny, K. F.; Stabley, D. L.; Sol-Church, K (2014). "Truncating mutations in the last exon of NOTCH3 cause lateral meningocele syndrome". American Journal of Medical Genetics Part A. 167A (2): 271–81. doi:10.1002/ajmg.a.36863. PMC 5589071. PMID 25394726.
- ^ Ejaz, Resham; Carter, Melissa; Gripp, Karen (1993), Adam, Margaret P.; Ardinger, Holly H.; Pagon, Roberta A.; Wallace, Stephanie E. (eds.), "Lateral Meningocele Syndrome", GeneReviews®, Seattle (WA): University of Washington, Seattle, PMID 27336130, retrieved 2021-04-21
- ^ Lehman RAW, Stears JC, Wesenberg RL, Nusbaum ED (1977) Familial osteosclerosis with abnormalities of the nervous system and meninges. J Pediat 90: 49-54
External links[]
| Classification | |
|---|---|
| External resources |
- Syndromes with craniofacial abnormalities
- Syndromes affecting the nervous system
- Disease stubs
- Human reproduction stubs
- Genetic disorder stubs