Chronic mucocutaneous candidiasis
| Chronic mucocutaneous candidiasis | |
|---|---|
| Other names | CMC[1] |
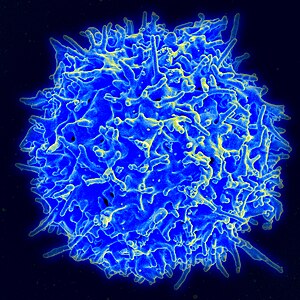 | |
| This condition is due to T-cells(immune) disorder | |
| Specialty | Infectious diseases, dermatology |
| Symptoms | Skin ulcer[2] |
| Types | CANDF1,2,3,4,5,6,7,8 and 9j |
| Diagnostic method | Thyroid function test, Liver function test[3][4] |
| Treatment | Systemic antifungal therapy[4] |
Chronic mucocutaneous candidiasis is an immune disorder of T cells,[4] it is characterized by chronic infections with Candida that are limited to mucosal surfaces, skin, and nails.[5]: 310 It can also be associated with other types of infections, such as human papilloma virus. An association with chromosome 2 has been identified.[medical citation needed]
Symptoms and signs[]
The symptoms of this condition are hyperkeratosis, skin ulcer, dyspareunia, endocardium abnormality, vision problems, hepatitis, seizures, hematuria and meningitis.[2]
Associated Diseases or Conditions[]
There are a number of disorders associated with chronic mucocutaneous candidiasis including endocrine dysfunctions, vitiligo, malabsorption syndromes, neoplasms and others. In most patients, chronic mucocutaneous candidiasis is correlated to abnormalities in cell mediated immunity (T-lymphocyte mediated response)[citation needed]. The T-lymphocytes fail to produce the necessary cytokines that are required for immunity against Candida. Current effective treatments include antifungal drugs and, for long term remissions, restoration of cellular immunity.[6]
Chronic autoimmune endocrinopathies are sometimes linked to chronic mucocutaneous candidiasis, but rarely cause systemic disease or septicemia[citation needed] Patients with autosomal-dominant mucocutaneous candidiasis may be at risk for epidermoid esophageal cancer due to the nitrosamine compounds produced by chronic candida infection.[citation needed][7]
Cause[]
Chronic mucocutaneous candidiasis can be inherited either autosomal dominant or autosomal recessive.[1] There are 9 types of this condition with the first CANDF1 being located at 2p22.3-p21 (cytogenetically).[8]
Mechanism[]
The mechanism of the human immune system has it normally fighting in an infection (like Candida). Initially Th17 cells are made by the immune system, which in turn produces interleukin-17 (IL-17). Inflammation is induced and white blood cells confront infection.[9]
Chronic mucocutaneous candidiasis mutations affect IL-17 by inhibiting its pathway. This in turn affects the human immune systems ability to fight infection, in total there are 9 possible types of this condition.[9][10]
Diagnosis[]
Chronic mucocutaneous candidiasis can be diagnosed in an affected individual via the following methods/tests:[3][4]
- Thyroid function test
- Liver function test
- Cellular immunity test
- Skin biopsy
- Genetic testing

Types[]

| Type | OMIMα | Gene | Locus |
|---|---|---|---|
| CANDF1 | 114580 | - | 2p |
| CANDF2 | 212050 | CARD9 | 9q34.3 |
| CANDF3 | 607644 | - | 11 |
| CANDF4 | 613108 | CLEC7A | 12p13.2-p12.3 |
| CANDF5 | 613953 | IL17RA | 22q11 |
| CANDF6 | 613956 | IL17F | 6p12 |
| CANDF7 | 614162 | STAT1 | 2q32 |
| CANDF8 | 615527 | TRAF3IP2 | 6q21 |
| CANDF9 | 616445 | IL17RC | 3q25 |
Treatment[]

Management for an individual with chronic mucocutaneous candidiasis consists of the following (relapse occurs once treatment is ceased, in many cases):[4][11]
- Systemic antifungal therapy(e.g. Fluconazole)
- Transfer factor
- Combination therapy
- Screening (annually)
See also[]
- Candidiasis
- List of cutaneous conditions
Notes[]
^ Indicates 9 references to specific, numbered pages in the Online Mendelian Inheritance in Man database.
References[]
- ^ Jump up to: a b RESERVED, INSERM US14 -- ALL RIGHTS. "Orphanet: Chronic mucocutaneous candidiasis". www.orpha.net. Retrieved 2017-06-09.
- ^ Jump up to: a b "Candidiasis familial chronic mucocutaneous, autosomal recessive | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 2017-06-09.
- ^ Jump up to: a b "Familial chronic mucocutaneous candidiasis - Conditions - GTR - NCBI". www.ncbi.nlm.nih.gov. Retrieved 2017-06-09.
- ^ Jump up to: a b c d e "Chronic Mucocutaneous Candidiasis: Background, Pathophysiology, Epidemiology". Medscape. 3 May 2017. Retrieved 8 June 2017.
- ^ James, William D.; Berger, Timothy G. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 978-0-7216-2921-6.
- ^ Kirkpatrick, Charles H. (February 2001). "Chronic mucocutaneous candidiasis". The Pediatric Infectious Disease Journal. 20 (2): 197–206. doi:10.1097/00006454-200102000-00017. PMID 11224843.
- ^ Rosa DD, Pasqualotto AC, Denning DW. Chronic mucocutaneous candidiasis and oesophageal cancer. Med Mycol. 2008 Feb;46(1):85-91. doi: 10.1080/13693780701616023. PMID: 17852718.
- ^ "OMIM Entry - % 114580 - CANDIDIASIS, FAMILIAL, 1; CANDF1". omim.org. Retrieved 9 June 2017.
- ^ Jump up to: a b Reference, Genetics Home. "familial candidiasis". Genetics Home Reference. Retrieved 2017-06-09.
- ^ Smeekens, Sanne P; van de Veerdonk, Frank L; Kullberg, Bart Jan; Netea, Mihai G (2013). "Genetic susceptibility to Candida infections". EMBO Molecular Medicine. 5 (6): 805–813. doi:10.1002/emmm.201201678. ISSN 1757-4676. PMC 3779444. PMID 23629947.
- ^ Teng, Joyce; Marqueling, Ann L.; Benjamin, Latanya (2016-12-15). Therapy in Pediatric Dermatology: Management of Pediatric Skin Disease. Springer. p. 265. ISBN 9783319436302.
Further reading[]
- Kauffman, Carol A.; Pappas, Peter G.; Sobel, Jack D.; Dismukes, William E. (2011). Essentials of Clinical Mycology. Springer Science & Business Media. ISBN 9781441966407. Retrieved 9 June 2017.
- Ostler, H. Bruce (2004). Diseases of the Eye and Skin: A Color Atlas. Lippincott Williams & Wilkins. ISBN 9780781749992. Retrieved 9 June 2017.
External links[]
| Classification | |
|---|---|
| External resources |
| Scholia has a topic profile for Chronic mucocutaneous candidiasis. |
- Mycosis-related cutaneous conditions
- Defects in innate immunity
- IUIS-PID table 3 immunodeficiencies