Hydroxyapatite
| Hydroxyapatite | |
|---|---|
 Hydroxyapatite crystals on matrix | |
| General | |
| Category | Phosphate mineral Apatite group |
| Formula (repeating unit) | Ca5(PO4)3(OH) |
| Strunz classification | 8.BN.05 |
| Crystal system | Hexagonal |
| Crystal class | Dipyramidal (6/m) H-M Symbol (6/m) |
| Space group | P63/m |
| Unit cell | a = 9.41 Å, c = 6.88 Å; Z = 2 |
| Identification | |
| Formula mass | 502.31 g/mol |
| Color | Colorless, white, gray, yellow, yellowish green |
| Crystal habit | As tabular crystals and as stalagmites, nodules, in crystalline to massive crusts |
| Cleavage | Poor on {0001} and {1010} |
| Fracture | Conchoidal |
| Tenacity | Brittle |
| Mohs scale hardness | 5 |
| Luster | Vitreous to subresinous, earthy |
| Streak | White |
| Diaphaneity | Transparent to translucent |
| Specific gravity | 3.14–3.21 (measured), 3.16 (calculated) |
| Optical properties | Uniaxial (-) |
| Refractive index | nω = 1.651 nε = 1.644 |
| Birefringence | δ = 0.007 |
| References | [1][2][3] |



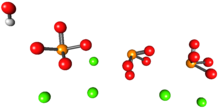
Hydroxyapatite, also called hydroxylapatite (HA), is a naturally occurring mineral form of calcium apatite with the formula Ca5(PO4)3(OH), but it is usually written Ca10(PO4)6(OH)2 to denote that the crystal unit cell comprises two entities.[4] Hydroxyapatite is the hydroxyl endmember of the complex apatite group. The OH− ion can be replaced by fluoride, chloride or carbonate, producing fluorapatite or chlorapatite. It crystallizes in the hexagonal crystal system. Pure hydroxyapatite powder is white. Naturally occurring apatites can, however, also have brown, yellow, or green colorations, comparable to the discolorations of dental fluorosis.
Up to 50% by volume and 70% by weight of human bone is a modified form of hydroxyapatite, known as bone mineral.[5] Carbonated calcium-deficient hydroxyapatite is the main mineral of which dental enamel and dentin are composed. Hydroxyapatite crystals are also found in the small calcifications, within the pineal gland and other structures, known as corpora arenacea or 'brain sand'.[6]
Chemical synthesis[]
Hydroxyapatite can be synthesized via several methods, such as wet chemical deposition, biomimetic deposition, sol-gel route (wet-chemical precipitation) or electrodeposition.[7] The hydroxyapatite nanocrystal suspension can be prepared by a wet chemical precipitation reaction following the reaction equation below:[8]
10 Ca(OH)2 + 6 H3PO4 → Ca10(PO4)6(OH)2 + 18 H2O
The ability to synthetically replicate hydroxyapatite has invaluable clinical implications, especially in dentistry. Each technique yields hydroxyapatite crystals of varied characteristics, such as size and shape.[9] These variations have a marked effect on the biological and mechanical properties of the compound, and therefore these hydroxyapatite products have different clinical uses.[10]
Calcium-deficient hydroxyapatite[]
Calcium-deficient (non-stochiometric) hydroxyapatite, Ca10−x(PO4)6−x(HPO4)x(OH)2−x (where x is between 0 and 1) has a Ca/P ratio between 1.67 and 1.5. The Ca/P ratio is often used in the discussion of calcium phosphate phases.[11] Stoichiometric apatite Ca10(PO4)6(OH)2 has a Ca/P ratio of 10:6 normally expressed as 1.67. The non-stoichiometric phases have the hydroxyapatite structure with cation vacancies (Ca2+) and anion (OH−) vacancies. The sites occupied solely by phosphate anions in stoichiometric hydroxyapatite, are occupied by phosphate or hydrogen phosphate, HPO42−, anions.[11] Preparation of these calcium-deficient phases can be prepared by precipitation from a mixture of calcium nitrate and diammonium phosphate with the desired Ca/P ratio, for example, to make a sample with a Ca/P ratio of 1.6:[12]
- 9.6 Ca(NO3)2 + 6 (NH4)2HPO4 → Ca9.6(PO4)5.6(HPO4)0.4(OH)1.6
Sintering these non-stoichiometric phases forms a solid phase which is an intimate mixture of tricalcium phosphate and hydroxyapatite, termed biphasic calcium phosphate:[13]
- Ca10−x(PO4)6−x(HPO4)x(OH)2−x → (1 − x) Ca10(PO4)6(OH)2 + 3x Ca3(PO4)2
Biological function[]
Mantis shrimp[]
The clubbing appendages of the Odontodactylus scyllarus (peacock mantis shrimp) are made of an extremely dense form of the mineral which has a higher specific strength; this has led to its investigation for potential synthesis and engineering use.[14] Their dactyl appendages have excellent impact resistance due to the impact region being composed of mainly crystalline hydroxyapatite, which offers significant hardness. A periodic layer underneath the impact layer composed of hydroxyapatite with lower calcium and phosphorus content (thus resulting in a much lower modulus) inhibits crack growth by forcing new cracks to change directions. This periodic layer also reduces the energy transferred across both layers due to the large difference in modulus, even reflecting some of the incident energy.[15]
Mammal/primate/human[]
Hydroxyapatite is present in bone and teeth; bone is made primarily of HA crystals interspersed in a collagen matrix—65 to 70% of the mass of bone is HA. Similarly HA is 70 to 80% of the mass of dentin and enamel in teeth. In enamel, the matrix for HA is formed by amelogenins and enamelins instead of collagen.[16]
Hydroxyapatite deposits in tendons around joints results in the medical condition calcific tendinitis.[17]
Hydroxyapatite in remineralisation of tooth enamel[]
Remineralisation of tooth enamel involves the reintroduction of mineral ions into demineralised enamel.[18] Hydroxyapatite is the main mineral component of enamel in teeth.[19] During demineralisation, calcium and phosphorus ions are drawn out from the hydroxyapatite.The mineral ions introduced during remineralisation restore the structure of the hydroxyapatite[19] crystals.
Use in dentistry[]
As of 2019, the use of hydroxyapatite, or its synthetically manufactured form, nano-hydroxyapatite, is not yet common practice. Some studies suggest it is useful in counteracting dentine hypersensitivity, preventing sensitivity after teeth bleaching procedures and caries prevention.[20][21][22] Avian eggshell hydroxyapatite can be a viable filler material in bone regeneration procedures in oral surgery. [23]
Dentine sensitivity[]
Nano-hydroxyapatite possesses bioactive components which can prompt the mineralisation process of teeth, remedying hypersensitivity. Hypersensitivity of teeth is thought to be regulated by fluid within dentinal tubules.[20] The movement of this fluid as a result of different stimuli is said to excite receptor cells in the pulp and trigger sensations of pain.[20] The physical properties of the nano-hydroxyapatite can penetrate and seal the tubules, stopping the circulation of the fluid and therefore the sensations of pain from stimuli.[21] Nano-hydroxyapatite would be preferred as it parallels the natural process of surface remineralisation.[22]
In comparison to alternative treatments for dentine hypersensitivity relief nano-hydroxyapatite containing treatment has been shown to perform better clinically. Nano-hydroxyapatite was proven to be better than other treatments at reducing sensitivity against evaporative stimuli, such as an air blast, and tactile stimuli, such as tapping the tooth with a dental instrument. However, no difference was seen between nano-hydroxyapatite and other treatments for cold stimuli.[24] Hydroxyapatite has shown significant medium and long-term desensitizing effects on dentine hypersensitivity using evaporative stimuli and the visual analogue scale (alongside potassium nitrate, arginine, glutaraldehyde with hydroxyethyl methacrylate, hydroxyapatite, adhesive systems, glass ionomer cements and laser).[25]
Co-agent for bleaching[]
Teeth bleaching agents release reactive oxygen species which can degrade enamel.[21] To prevent this, nano-hydroxyapatite can be added to the bleaching solution to reduce the impact of the bleaching agent by blocking pores within the enamel.[21] This reduces sensitivity after the bleaching process.[22]
Caries prevention[]
Nano-hydroxyapatite possesses a remineralising effect on teeth and can be used to prevent damage from carious attacks.[22] In the event of an acid attack by cariogenic bacteria, nano-hydroxyapatite particles can infiltrate pores on the tooth surface to form a protective layer.[21] Furthermore, nano-hydroxyapatite may have the capacity to reverse damage from carious assaults by either directly replacing deteriorated surface minerals or acting as a binding agent for lost ions.[21]
In the future, there are possibilities for using nano-hydroxyapatite for tissue engineering and repair. The main and most advantageous feature of nano-hydroxyapatite is its biocompatibility.[26] It is chemically similar to naturally occurring hydroxyapatite and can mimic the structure and biological function of the structures found in the resident extracellular matrix.[27] Therefore, it can be used as a scaffold for engineering tissues such as bone and cementum.[21] It may be used to restore cleft lips and palates and refine existing practices such as preservation of alveolar bone after extraction for better implant placement.[21]
As a dental material[]
Hydroxyapatite is widely used within dentistry and oral and maxillofacial surgery, due to its chemical similarity to hard tissue.[28]
In some toothpaste hydroxyapatite can be found in the form of nanocrystals (as these are easily dissolved). In recent years, hydroxyapatite nanocrystals (nHA) have been used in toothpaste to combat dental hypersensitivity. They aid in the repair and remineralisation of the enamel, thus helping to prevent tooth sensitivity. Tooth enamel can become demineralised due to various factors, including acidic erosion and dental caries. If left untreated this can lead to the exposure of dentin and subsequent exposure of the dental pulp. In various studies the use of nano hydroxyapatite in toothpaste showed positive results in aiding the remineralisation of dental enamel.[29]
Synthetic hydroxyapatite (SHA) is proven to provide successful outcomes in alveolar socket preservation. Socket grafting using synthetic hydroxyapatite can result in successful bone regeneration.[30]
Safety concerns[]
The European Commission's Scientific Committee on Consumer Safety (SCCS) issued an official opinion in 2021, where it considered whether the nanomaterial hydroxyapatite was safe when used in leave-on and rinse-off dermal and oral cosmetic products, taking into account reasonably foreseeable exposure conditions. It stated:[31]
Having considered the data provided, and other relevant information available in scientific literature, the SCCS cannot conclude on the safety of the hydroxyapatite composed of rod–shaped nanoparticles for use in oral-care cosmetic products at the maximum concentrations and specifications given in this Opinion. This is because the available data/information is not sufficient to exclude concerns over the genotoxic potential of HAP-nano.
Chromatography[]
This section does not cite any sources. (November 2020) |
The mechanism of hydroxyapatite chromatography is complicated and has been described as "mixed-mode". It involves ionic interactions between positively charged groups on a biomolecule (often a protein) and the phosphate groups in hydroxyapatite, and metal chelation between hydroxyapatite calcium ions and negatively charged phosphate and/or carboxyl groups on the biomolecule. It may be difficult to predict the effectiveness of hydroxyapatite chromatography based on physical and chemical properties of the desired protein to be purified. For elution, a buffer with increasing phosphate and/or neutral salt concentration is typically used.
Use in archaeology[]
In archaeology, hydroxyapatite from human and animal remains can be analysed to reconstruct ancient diets, migrations and paleoclimate. The mineral fractions of bone and teeth act as a reservoir of trace elements, including carbon, oxygen and strontium. Stable isotope analysis of human and faunal hydroxyapatite can be used to indicate whether a diet was predominantly terrestrial or marine in nature (carbon, strontium);[32] the geographical origin and migratory habits of an animal or human (oxygen, strontium)[33] and to reconstruct past temperatures and climate shifts (oxygen).[34] Post-depositional alteration of bone can contribute to the degradation of bone collagen, the protein required for stable isotope analysis.[35]
Defluoridation[]
Hydroxyapatite is a potential adsorbent for the defluoridation of drinking water, as it forms fluorapatite in a three step process. Hydroxyapatite removes F− from the water to replace OH− forming fluorapatite. However, during the defluoridation process the hydroxyapatite dissolves, and increases the pH and phosphate ion concentration which makes the defluoridated water unfit for drinking.[36] Recently, a ″calcium amended-hydroxyapatite″ defluoridation technique was suggested to overcome the phosphate leaching from hydroxyapatite.[36] This technique can also affect fluorosis reversal by providing calcium-enriched alkaline drinking water to fluorosis affected areas.
See also[]
References[]
- ^ Hydroxylapatite on Mindat
- ^ Hydroxylapatite on Webmineral
- ^ Anthony, John W.; Bideaux, Richard A.; Bladh, Kenneth W.; Nichols, Monte C., eds. (2000). "Hydroxylapatite". Handbook of Mineralogy (PDF). IV (Arsenates, Phosphates, Vanadates). Chantilly, VA, US: Mineralogical Society of America. ISBN 978-0962209734. Archived (PDF) from the original on 2018-09-29. Retrieved 2010-08-29.
- ^ Singh, Anamika; Tiwari, Atul; Bajpai, Jaya; Bajpai, Anil K. (2018-01-01), Tiwari, Atul (ed.), "3 - Polymer-Based Antimicrobial Coatings as Potential Biomaterials: From Action to Application", Handbook of Antimicrobial Coatings, Elsevier, pp. 27–61, doi:10.1016/b978-0-12-811982-2.00003-2, ISBN 978-0-12-811982-2, retrieved 2020-11-18
- ^
Junqueira, Luiz Carlos; José Carneiro (2003). Foltin, Janet; Lebowitz, Harriet; Boyle, Peter J. (eds.). Basic Histology, Text & Atlas (10th ed.). McGraw-Hill Companies. p. 144. ISBN 978-0-07-137829-1.
Inorganic matter represents about 50% of the dry weight of bone ... crystals show imperfections and are not identical to the hydroxyapatite found in the rock minerals
- ^ Angervall, Lennart; Berger, Sven; Röckert, Hans (2009). "A Microradiographic and X-Ray Crystallographic Study of Calcium in the Pineal Body and in Intracranial Tumours". Acta Pathologica et Microbiologica Scandinavica. 44 (2): 113–19. doi:10.1111/j.1699-0463.1958.tb01060.x. PMID 13594470.
- ^ Ferraz, M. P.; Monteiro, F. J.; Manuel, C. M. (2004). "Hydroxyapatite nanoparticles: A review of preparation methodologies". Journal of Applied Biomaterials & Biomechanics. 2 (2): 74–80. PMID 20803440.
- ^ Bouyer, E.; Gitzhofer, F.; Boulos, M. I. (2000). "Morphological study of hydroxyapatite nanocrystal suspension". Journal of Materials Science: Materials in Medicine. 11 (8): 523–31. doi:10.1023/A:1008918110156. PMID 15348004. S2CID 35199514.
- ^ Mohd Pu'ad, N. A. S.; Abdul Haq, R. H.; Mohd Noh, H.; Abdullah, H. Z.; Idris, M. I.; Lee, T. C. (2020-01-01). "Synthesis method of hydroxyapatite: A review". Materials Today: Proceedings. 4th Advanced Materials Conference 2018, 4th AMC 2018, 27th & 28th November 2018, Hilton Kuching Hotel, Kuching, Sarawak, Malaysia. 29: 233–39. doi:10.1016/j.matpr.2020.05.536. ISSN 2214-7853.
- ^ Cox, Sophie C.; Walton, Richard I.; Mallick, Kajal K. (2015-03-01). "Comparison of techniques for the synthesis of hydroxyapatite". Bioinspired, Biomimetic and Nanobiomaterials. 4 (1): 37–47. doi:10.1680/bbn.14.00010. ISSN 2045-9858.
- ^ Jump up to: a b Rey, C.; Combes, C.; Drouet, C.; Grossin, D. (2011). "1.111 – Bioactive Ceramics: Physical Chemistry". In Ducheyne, Paul (ed.). Comprehensive Biomaterials. 1. Elsevier. pp. 187–281. doi:10.1016/B978-0-08-055294-1.00178-1. ISBN 978-0-08-055294-1.
- ^ Raynaud, S.; Champion, E.; Bernache-Assollant, D.; Thomas, P. (2002). "Calcium phosphate apatites with variable Ca/P atomic ratio I. Synthesis, characterisation and thermal stability of powders". Biomaterials. 23 (4): 1065–72. doi:10.1016/S0142-9612(01)00218-6. PMID 11791909.
- ^ Valletregi, M. (1997). "Synthesis and characterisation of calcium deficient apatite". Solid State Ionics. 101–103: 1279–85. doi:10.1016/S0167-2738(97)00213-0.
- ^ Weaver, J. C.; Milliron, G. W.; Miserez, A.; Evans-Lutterodt, K.; Herrera, S.; Gallana, I.; Mershon, W. J.; Swanson, B.; Zavattieri, P.; Dimasi, E.; Kisailus, D. (2012). "The Stomatopod Dactyl Club: A Formidable Damage-Tolerant Biological Hammer". Science. 336 (6086): 1275–80. Bibcode:2012Sci...336.1275W. doi:10.1126/science.1218764. PMID 22679090. S2CID 8509385. Archived from the original on 2020-09-13. Retrieved 2017-12-02.
- ^ Tanner, K. E. (2012). "Small but Extremely Tough". Science. 336 (6086): 1237–38. Bibcode:2012Sci...336.1237T. doi:10.1126/science.1222642. PMID 22679085. S2CID 206541609.
- ^ Habibah, TU; Salisbury, HG (January 2018). "Biomaterials, Hydroxyapatite". PMID 30020686. Archived from the original on 2020-03-28. Retrieved 2018-08-12. Cite journal requires
|journal=(help) - ^ Carcia, CR; Scibek, JS (March 2013). "Causation and management of calcific tendonitis and periarthritis". Current Opinion in Rheumatology. 25 (2): 204–09. doi:10.1097/bor.0b013e32835d4e85. PMID 23370373. S2CID 36809845.
- ^ Abou Neel, Ensanya Ali; Aljabo, Anas; Strange, Adam; Ibrahim, Salwa; Coathup, Melanie; Young, Anne M.; Bozec, Laurent; Mudera, Vivek (2016). "Demineralization-remineralization dynamics in teeth and bone". International Journal of Nanomedicine. 11: 4743–63. doi:10.2147/IJN.S107624. ISSN 1178-2013. PMC 5034904. PMID 27695330.
- ^ Jump up to: a b Pepla, Erlind; Besharat, Lait Kostantinos; Palaia, Gaspare; Tenore, Gianluca; Migliau, Guido (July 2014). "Nano-hydroxyapatite and its applications in preventive, restorative and regenerative dentistry: a review of literature". Annali di Stomatologia. 5 (3): 108–14. ISSN 1824-0852. PMC 4252862. PMID 25506416.
- ^ Jump up to: a b c de Melo Alencar, Cristiane; de Paula, Brennda Lucy Freitas; Guanipa Ortiz, Mariangela Ivette; Baraúna Magno, Marcela; Martins Silva, Cecy; Cople Maia, Lucianne (March 2019). "Clinical efficacy of nano-hydroxyapatite in dentin hypersensitivity: A systematic review and meta-analysis". Journal of Dentistry. 82: 11–21. doi:10.1016/j.jdent.2018.12.014. ISSN 1879-176X. PMID 30611773.
- ^ Jump up to: a b c d e f g h Bordea, Ioana Roxana; Candrea, Sebastian; Alexescu, Gabriela Teodora; Bran, Simion; Băciuț, Mihaela; Băciuț, Grigore; Lucaciu, Ondine; Dinu, Cristian Mihail; Todea, Doina Adina (2020-04-02). "Nano-hydroxyapatite use in dentistry: a systematic review". Drug Metabolism Reviews. 52 (2): 319–32. doi:10.1080/03602532.2020.1758713. ISSN 0360-2532. PMID 32393070. S2CID 218598747.
- ^ Jump up to: a b c d Pepla, Erlind; Besharat, Lait Kostantinos; Palaia, Gaspare; Tenore, Gianluca; Migliau, Guido (2014-11-20). "Nano-hydroxyapatite and its applications in preventive, restorative and regenerative dentistry: a review of literature". Annali di Stomatologia. 5 (3): 108–14. ISSN 1824-0852. PMC 4252862. PMID 25506416.
- ^ Opris, H., Bran, S., Dinu, C., Baciut, M., Prodan, D. A., Mester, A., & Baciut, G. (2020). Clinical applications of avian eggshell-derived hydroxyapatite. Bosnian journal of basic medical sciences, 20(4), 430–37. https://doi.org/10.17305/bjbms.2020.4888
- ^ de Melo Alencar, Cristiane; de Paula, Brennda Lucy Freitas; Guanipa Ortiz, Mariangela Ivette; Baraúna Magno, Marcela; Martins Silva, Cecy; Cople Maia, Lucianne (March 2019). "Clinical efficacy of nano-hydroxyapatite in dentin hypersensitivity: A systematic review and meta-analysis". Journal of Dentistry. 82: 11–21. doi:10.1016/j.jdent.2018.12.014. PMID 30611773.
- ^ Marto, Carlos Miguel; Paula, Anabela Baptista; Nunes, Tiago; Pimenta, Miguel; Abrantes, Ana Margarida; Pires, Ana Salomé; Laranjo, Mafalda; Coelho, Ana; Donato, Helena; Botelho, Maria Filomena; Ferreira, Manuel Marques (2019). "Evaluation of the efficacy of dentin hypersensitivity treatments—A systematic review and follow-up analysis". Journal of Oral Rehabilitation. 46 (10): 952–90. doi:10.1111/joor.12842. hdl:10400.4/2240. ISSN 1365-2842. PMID 31216069.
- ^ Shepherd, J. H.; Friederichs, R. J.; Best, S. M. (2015-01-01), Mucalo, Michael (ed.), "11 – Synthetic hydroxyapatite for tissue engineering applications", Hydroxyapatite (Hap) for Biomedical Applications, Woodhead Publishing Series in Biomaterials, Woodhead Publishing, pp. 235–67, ISBN 978-1-78242-033-0, retrieved 2021-03-06
- ^ Zhou, Hongjian; Lee, Jaebeom (2011-07-01). "Nanoscale hydroxyapatite particles for bone tissue engineering". Acta Biomaterialia. 7 (7): 2769–81. doi:10.1016/j.actbio.2011.03.019. ISSN 1742-7061. PMID 21440094.
- ^ Habibah, Tutut Ummul; Amlani, Dharanshi V.; Brizuela, Melina (2021), "Hydroxyapatite Dental Material", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30020686, retrieved 2021-03-11
- ^ Pajor, Kamil; Pajchel, Lukasz; Kolmas, Joanna (January 2019). "Hydroxyapatite and Fluorapatite in Conservative Dentistry and Oral Implantology – A Review". Materials. 12 (17): 2683. Bibcode:2019Mate...12.2683P. doi:10.3390/ma12172683. PMC 6747619. PMID 31443429.
- ^ Kattimani VS, Prathigudupu RS, Jairaj A, Khader MA, Rajeev K, Khader AA. Role of Synthetic Hydroxyapatite-In Socket Preservation: A Systematic Review and Meta-analysis. J Contemp Dent Pract. 2019 Aug 1;20(8):987–93. PMID 31797859.
- ^ European Commission Scientific Committee on Consumer Safety, Opinion on Hydroxyapatite (nano), SCCS/1624/20 – 30–31 March 2021
- ^ Richards, M. P.; Schulting, R. J.; Hedges, R. E. M. (2003). "Archaeology: Sharp shift in diet at onset of Neolithic" (PDF). Nature. 425 (6956): 366. Bibcode:2003Natur.425..366R. doi:10.1038/425366a. PMID 14508478. S2CID 4366155. Archived from the original (PDF) on 2011-03-07. Retrieved 2015-08-28.
- ^ Britton, K.; Grimes, V.; Dau, J.; Richards, M. P. (2009). "Reconstructing faunal migrations using intra-tooth sampling and strontium and oxygen isotope analyses: A case study of modern caribou (Rangifer tarandus granti)". Journal of Archaeological Science. 36 (5): 1163–72. doi:10.1016/j.jas.2009.01.003.
- ^ Daniel Bryant, J.; Luz, B.; Froelich, P. N. (1994). "Oxygen isotopic composition of fossil horse tooth phosphate as a record of continental paleoclimate". Palaeogeography, Palaeoclimatology, Palaeoecology. 107 (3–4): 303–16. Bibcode:1994PPP...107..303D. doi:10.1016/0031-0182(94)90102-3.
- ^ Van Klinken, G. J. (1999). "Bone Collagen Quality Indicators for Palaeodietary and Radiocarbon Measurements". Journal of Archaeological Science. 26 (6): 687–95. doi:10.1006/jasc.1998.0385. Archived from the original on 2020-09-13. Retrieved 2017-12-02.
External links[]
![]() Media related to Hydroxylapatite at Wikimedia Commons
Media related to Hydroxylapatite at Wikimedia Commons
- Calcium minerals
- Phosphate minerals
- Ceramic materials
- Biomaterials
- Hexagonal minerals
- Minerals in space group 176