LGBT reproduction
| Part of a series on |
| LGBT topics |
|---|
|
|
|
LGBT reproduction refers to lesbian, gay, bisexual, and transgender (LGBT) people having biological children by means of assisted reproductive technology. It is distinct from LGBT parenting, which is a broader cultural phenomenon including LGBT adoption. In recent decades, developmental biologists have been researching and developing techniques to facilitate same-sex reproduction.[1] [2]
The obvious approaches, subject to a growing amount of activity, are female sperm and male eggs, with female sperm closer to being a reality for humans. In 2004, by altering the function of a few genes involved with imprinting, other Japanese scientists combined two mouse eggs to produce daughter mice[3] and in 2018 Chinese scientists created 29 female mice from two female mice mothers but were unable to produce viable offspring from two father mice.[4][5] One of the possibilities is obtaining sperm from skin stem cells.[6]
Gay men[]
Some gay couples decide to have a surrogate pregnancy. A surrogate is a woman carrying an egg fertilized by sperm of one of the men. Some women become surrogates for money, others for humanitarian reasons or both.[7] This allows one of the men to be the biological father while the other will be an adopted father.
Gay men who have become fathers using surrogacy have reported similar experiences to those as other couples who have used surrogacy, including their relationships both their child and their surrogate have.[8]
There is theoretical work being done on creating a zygote from two men which would enable both men to be biological fathers, but it is yet to be practically implemented.[9]
Lesbians[]
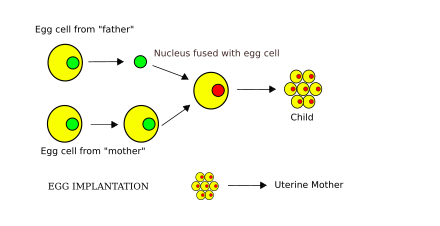
Partner-assisted reproduction, or co-IVF is a method of family building that is used by couples who both possess female reproductive organs. The method uses in vitro fertilization (IVF), a method that means eggs are removed from the ovaries, fertilized in a laboratory, and then one or more of the resulting embryos are placed in the uterus to hopefully create a pregnancy. Reciprocal IVF differs from standard IVF in that two women are involved: the eggs are taken from one partner, and the other partner carries the pregnancy.[10] In this way, the process is mechanically identical to IVF with egg donation.[11][12] Using this process ensures that each partner is a biological mother of the child according to advocates,[13] but in the strictest sense only one mother is the biological mother from a genetic standpoint and the other is a surrogate mother. However the practice has a symbolic weight greater than LGBT adoption, and may create a stronger bond between mother and child than adoption.
In a recent study, quality of infant-parent relationships was examined among egg donor families in comparison to in vitro fertilization families.[14] Infants were between the ages of 6–18 months. Through use of the Parent Development Interview (PDI) and observational assessment, the study found few differences between family types on the representational level, yet significant differences between family types on the observational level.[14] Egg donation mothers were less sensitive and structuring than IVF mothers, and egg donation infants were less emotionally responsive, and involving than IVF infants.[14]
There is theoretical work being done on creating a zygote from two women which would enable both women to be biological mothers, but it is yet to be practically implemented.[9] Creating a sperm from an egg and using it to fertilize another egg may offer a solution to this issue.[6] As is a process analogous to Somatic cell nuclear transfer involving two eggs being fused together[15]
If created, a "female sperm" cell could fertilize an egg cell, a procedure that, among other potential applications, might enable female same-sex couples to produce a child who would be the biological offspring of their two mothers. It is also claimed that production of female sperm may stimulate a woman to be both the mother and father (similar to asexual reproduction) of an offspring produced by her own sperm. Many queries, both ethical and moral, arise over these arguments.[16][17][18][19]
Transgender women[]
Many trans women want to have children.[citation needed] Some may seek to have children by using their own sperm and an egg donor or biological female partner. Fertility can be impeded in a variety of ways due to feminizing hormone therapy.
Estrogens suppress testosterone levels and at high doses can markedly disrupt sex drive and function and fertility on their own.[20][21][22][23] Moreover, disruption of gonadal function and fertility by estrogens may be permanent after extended exposure.[22][23]
Some trans women want to carry their own children through transgender pregnancy, which has its own set of issues to be overcome, because transgender women do not naturally have the anatomy needed for embryonic and fetal development. As of 2008, there were no successful cases of uterus transplantation concerning a transgender woman.[24]
Uterine transplantation, or UTx, is currently in its infancy and is not yet publicly available. As of 2019, in cisgender women, more than 42 UTx procedures had been performed, with 12 live births resulting from the transplanted uteruses as of publication.[25] The International Society of Uterine Transplantation (ISUTx) was established internationally in 2016, with 70 clinical doctors and scientists, and currently has 140 intercontinental delegates.[26] Its goal is to, "through scientific innovations, advance medical care in the field of uterus transplantation."[27]
In 2012, McGill University published the "Montreal Criteria for the Ethical Feasibility of Uterine Transplantation", a proposed set of criteria for carrying out uterine transplants, in Transplant International.[28] Under these criteria, only a cisgender woman could ethically be considered a transplant recipient. The exclusion of trans women from candidacy may lack justification.[29]
In addition, if trans women wish to conceive with a biological male partner, they face the same issues that cisgender gay couples have in creating a zygote.
Transgender men[]
Transgender men have a unique situation when it comes to LGBT reproduction as they are the only group that has a risk of unintended pregnancy in a same-gender relationship.[30][31] Pregnancy is possible for transgender men who retain a functioning vagina, ovaries, and a uterus.[32][33][34]
Testosterone therapy affects fertility, but many trans men who have become pregnant were able to do so within six months of stopping testosterone.[30] Future pregnancies can be achieved by oophyte banking, but the process may increase gender dysphoria or may not be accessible due to lack of insurance coverage.[30] Testosterone therapy is not a sufficient method of contraception, and trans men may experience unintended pregnancy,[30][31] especially if they miss doses.[30]
Many gay transgender men choose to freeze their eggs before transitioning, and choose to have a female surrogate carry their child while when the time comes, using their eggs and their cis male partner's sperm. This allows them to avoid the potentially dysphoria inducing experience of pregnancy, or cessation of HRT for collecting eggs at an older age.[35] [36]
References[]
- ^ Quick D (9 December 2010). "Breakthrough raises possibility of genetic children for same-sex couples". Retrieved 26 July 2015.
- ^ "Timeline of same-sex procreation scientific developments". samesexprocreation.com.
- ^ "Japanese scientists produce mice without using sperm". The Washington Post. Sarasota Herald-Tribune. April 22, 2004.
- ^ Blakely, Rhys (2018-10-12). "No father necessary as mice are created with two mothers". The Times. ISSN 0140-0460. Retrieved 2018-10-12.
- ^ Li, Zhi-Kun; Wang, Le-Yun; Wang, Li-Bin; Feng, Gui-Hai; Yuan, Xue-Wei; Liu, Chao; Xu, Kai; Li, Yu-Huan; Wan, Hai-Feng (2018-10-01). "Generation of Bimaternal and Bipaternal Mice from Hypomethylated Haploid ESCs with Imprinting Region Deletions". Cell Stem Cell. 23 (5): 665–676.e4. doi:10.1016/j.stem.2018.09.004. ISSN 1934-5909. PMID 30318303.
- ^ Jump up to: a b Murray I (2021). "Stem Cells and Same Sex Reproduction". Retrieved 26 July 2015.
- ^ "For Gay Men: Becoming a Parent through Surrogacy". Internet Health Resources. Retrieved 26 July 2015.
- ^ Blake L, Carone N, Slutsky J, Raffanello E, Ehrhardt AA, Golombok S (November 2016). "Gay father surrogacy families: relationships with surrogates and egg donors and parental disclosure of children's origins". Fertility and Sterility. 106 (6): 1503–1509. doi:10.1016/j.fertnstert.2016.08.013. PMC 5090043. PMID 27565261.
- ^ Jump up to: a b Ringler G (18 March 2015). "Get Ready for Embryos From Two Men or Two Women". Retrieved 4 July 2021.
- ^ Gilmour P (6 June 2018). "Shared motherhood: The amazing way lesbian couples are having babies". Cosmopolitan. Retrieved 21 March 2018.
- ^ Klatsky P (22 June 2017). "Co-Maternity And Reciprocal IVF: Empowering lesbian parents with options". Huffington Post. Retrieved 21 March 2018.
- ^ Marina S, Marina D, Marina F, Fosas N, Galiana N, Jové I (April 2010). "Sharing motherhood: biological lesbian co-mothers, a new IVF indication". Human Reproduction. 25 (4): 938–41. doi:10.1093/humrep/deq008. PMID 20145005.
- ^ Schenker JG (2011). Ethical dilemmas in assisted reproductive technologies. Berlin: De Gruyter. ISBN 978-3-11-024021-4. OCLC 763156926.
- ^ Jump up to: a b c Imrie S, Jadva V, Fishel S, Golombok S (July 2019). "Families Created by Egg Donation: Parent-Child Relationship Quality in Infancy". Child Development. 90 (4): 1333–1349. doi:10.1111/cdev.13124. PMC 6640047. PMID 30015989.
- ^ Foster H (2013-08-16). "Mommy 1 and Mommy 2: Could science end the age of Mom and Dad?". Science in the News. Retrieved 2021-07-05.
- ^ "Early-stage sperm cells created". Newcastle University. 2007-04-13. Archived from the original on 2013-11-09.
- ^ Highfield, Roger (2007-04-14). "Women may be able to grow own sperm". London: Daily Telegraph. Retrieved 2010-05-02.
- ^ Connor, Steve (2007-04-13). "The prospect of all-female conception". London: The Independent. Archived from the original on 2011-01-06. Retrieved 2010-05-02.
- ^ "Bone stem cells turned into primitive sperm cells". New Scientist. 2007-04-13.
- ^ Jones CA, Reiter L, Greenblatt E (2016). "Fertility preservation in transgender patients". International Journal of Transgenderism. 17 (2): 76–82. doi:10.1080/15532739.2016.1153992. ISSN 1553-2739. S2CID 58849546.
Traditionally, patients have been advised to cryopreserve sperm prior to starting cross-sex hormone therapy as there is a potential for a decline in sperm motility with high-dose estrogen therapy over time (Lubbert et al., 1992). However, this decline in fertility due to estrogen therapy is controversial due to limited studies.
- ^ Payne AH, Hardy MP (28 October 2007). The Leydig Cell in Health and Disease. Springer Science & Business Media. pp. 422–431. ISBN 978-1-59745-453-7.
Estrogens are highly efficient inhibitors of the hypothalamic-hypophyseal-testicular axis (212–214). Aside from their negative feedback action at the level of the hypothalamus and pituitary, direct inhibitory effects on the testis are likely (215,216). [...] The histology of the testes [with estrogen treatment] showed disorganization of the seminiferous tubules, vacuolization and absence of lumen, and compartmentalization of spermatogenesis.
- ^ Jump up to: a b Salam MA (2003). Principles & Practice of Urology: A Comprehensive Text. Universal-Publishers. pp. 684–. ISBN 978-1-58112-412-5.
Estrogens act primarily through negative feedback at the hypothalamic-pituitary level to reduce LH secretion and testicular androgen synthesis. [...] Interestingly, if the treatment with estrogens is discontinued after 3 yr. of uninterrupted exposure, serum testosterone may remain at castration levels for up to another 3 yr. This prolonged suppression is thought to result from a direct effect of estrogens on the Leydig cells.
- ^ Jump up to: a b Cox RL, Crawford ED (December 1995). "Estrogens in the treatment of prostate cancer". The Journal of Urology. 154 (6): 1991–8. doi:10.1016/S0022-5347(01)66670-9. PMID 7500443.
- ^ Leith W (2008-04-10). "Pregnant men: hard to stomach?". Telegraph. London.
- ^ Jones BP, Williams NJ, Saso S, Thum MY, Quiroga I, Yazbek J, et al. (January 2019). "Uterine transplantation in transgender women". BJOG. 126 (2): 152–156. doi:10.1111/1471-0528.15438. PMC 6492192. PMID 30125449.
- ^ "History of ISUTx". International Society for Uterus Transplantation (ISUTx).
- ^ "About - 'Vision'". International Society for Uterus Transplantation (ISUTx).
- ^ Lefkowitz A, Edwards M, Balayla J (April 2012). "The Montreal Criteria for the Ethical Feasibility of Uterine Transplantation". Transplant International. 25 (4): 439–47. doi:10.1111/j.1432-2277.2012.01438.x. PMID 22356169. S2CID 39516819.
- ^ Lefkowitz A, Edwards M, Balayla J (October 2013). "Ethical considerations in the era of the uterine transplant: an update of the Montreal Criteria for the Ethical Feasibility of Uterine Transplantation". Fertility and Sterility. 100 (4): 924–6. doi:10.1016/j.fertnstert.2013.05.026. PMID 23768985.
However, it certainly bears mentioning that there does not seem to be a prima facie ethical reason to reject the idea of performing uterine transplant on a male or trans patient. A male or trans patient wishing to gestate a child does not have a lesser claim to that desire than their female counterparts. The principle of autonomy is not sex-specific. This right is not absolute, but it is not the business of medicine to decide what is unreasonable to request for a person of sound mind, except as it relates to medical and surgical risk, as well as to distribution of resources. A male who identifies as a woman, for example, arguably has UFI, no functionally different from a woman who is born female with UFI. Irrespective of the surgical challenges involved, such a person's right to self-governance of her reproductive potential ought to be equal to her genetically female peers and should be respected.
- ^ Jump up to: a b c d e Berger AP, Potter EM, Shutters CM, Imborek KL (2015). "Pregnant transmen and barriers to high quality healthcare". Proceedings in Obstetrics and Gynecology. 5 (2): 1–12. doi:10.17077/2154-4751.1285.
- ^ Jump up to: a b Light A, Wang LF, Zeymo A, Gomez-Lobo V (October 2018). "Family planning and contraception use in transgender men". Contraception. 98 (4): 266–269. doi:10.1016/j.contraception.2018.06.006. PMID 29944875.
- ^ Obedin-Maliver J, Makadon HJ (March 2016). "Transgender men and pregnancy". Obstetric Medicine. 9 (1): 4–8. doi:10.1177/1753495X15612658. PMC 4790470. PMID 27030799.
- ^ Beatie T (14 March 2008). Labor of love : the story of one mans extraordinary pregnancy. Berkeley: Seal Press. ISBN 978-1-58005-300-6.
- ^ Beatie T (April 8, 2008). "Labor of Love: Is society ready for this pregnant husband?". The Advocate. p. 24.
- ^ Compton J (5 March 2019). "Transgender men, eager to have biological kids, are freezing their eggs". NBC News. Retrieved 2021-07-05.
- ^ "The T-Male: IVF and Surrogacy". www.thetransitionalmale.com. Retrieved 2021-07-05.
- Assisted reproductive technology
- Fertility medicine
- LGBT parenting
- Human reproduction
- LGBT and health care