Lymphocytic colitis
| Lymphocytic colitis | |
|---|---|
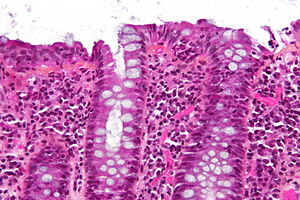 | |
| Micrograph of lymphocytic colitis. HPS stain. | |
| Specialty | Gastroenterology |
Lymphocytic colitis is a subtype of microscopic colitis, a condition characterized by chronic non-bloody watery diarrhea.[1][2]
Causes[]
No definite cause has been determined. The peak incidence of lymphocytic colitis is in persons over age 50; the disease affects women and men equally. Some reports have implicated long-term usage of NSAIDs, proton pump inhibitors, and selective serotonin reuptake inhibitors, and other drugs. Associations with other autoimmune disorders suggests that overactive immune responses occur.[3]
Diagnosis[]
The colonoscopy is normal but histology of the mucosal biopsy reveals an accumulation of lymphocytes in the colonic epithelium and connective tissue (lamina propria). Collagenous colitis shares this feature but additionally shows a distinctive thickening of the subepithelial collagen table.[1][2]
Treatment[]
Budesonide, in colonic release preparations, has been shown in randomized controlled trials to be effective in treating this disorder.[4][5] It helps control the diarrheal symptoms and treatment is usually given for several weeks. Sometimes it is used to prevent frequent relapses.
Over-the-counter antidiarrheal drugs may be effective for some people with lymphocytic colitis. Anti-inflammatory drugs, such as salicylates, mesalazine, and systemic corticosteroids may be prescribed for people who do not respond to other drug treatment. The long-term prognosis for this disease is good with a proportion of people suffering relapses which respond to treatment.[1]
History[]
Lymphocytic colitis was first described in 1989.[6]
See also[]
References[]
- ^ a b c Münch A, Aust D, Bohr J, Bonderup O, Fernández Bañares F, Hjortswang H, et al. (2012). "Microscopic colitis: Current status, present and future challenges: statements of the European Microscopic Colitis Group". J Crohns Colitis. 6 (9): 932–45. doi:10.1016/j.crohns.2012.05.014. PMID 22704658.
- ^ a b Rasmussen MA, Munck LK (2012). "Systematic review: are lymphocytic colitis and collagenous colitis two subtypes of the same disease - microscopic colitis?". Aliment Pharmacol Ther. 36 (2): 79–90. doi:10.1111/j.1365-2036.2012.05166.x. PMID 22670660. S2CID 24040089.
- ^ Park, T; Cave, D; Marshall, C (7 August 2015). "Microscopic colitis: A review of etiology, treatment and refractory disease". World Journal of Gastroenterology. 21 (29): 8804–10. doi:10.3748/wjg.v21.i29.8804. PMC 4528022. PMID 26269669.
- ^ Chande, N; Al Yatama, N; Bhanji, T; Nguyen, TM; McDonald, JW; MacDonald, JK (13 July 2017). "Interventions for treating lymphocytic colitis". The Cochrane Database of Systematic Reviews. 7 (11): CD006096. doi:10.1002/14651858.CD006096.pub4. PMC 6483541. PMID 28702956.
- ^ Fernández-Bañares F, Salas A, Esteve M, Espinós J, Forné M, Viver J (2003). "Collagenous and lymphocytic colitis. evaluation of clinical and histological features, response to treatment, and long-term follow-up". Am J Gastroenterol. 98 (2): 340–7. PMID 12591052.
- ^ Lazenby AJ, Yardley JH, Giardiello FM, Jessurun J, Bayless TM (1989). "Lymphocytic ("microscopic") colitis: a comparative histopathologic study with particular reference to collagenous colitis". Hum. Pathol. 20 (1): 18–28. doi:10.1016/0046-8177(89)90198-6. PMID 2912870.
External links[]
- Inflammations
- Colitis
- Steroid-responsive inflammatory conditions