Budesonide
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Pulmicort, Rhinocort, Entocort, others |
| Other names | BUD |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a608007 |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth, nasal, tracheal, rectal, inhalation |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 10-20% (first pass effect) |
| Protein binding | 85-90% |
| Metabolism | Liver CYP3A4 |
| Elimination half-life | 2.0-3.6 hours |
| Excretion | Urine, feces |
| Identifiers | |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| PDB ligand | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.051.927 |
| Chemical and physical data | |
| Formula | C25H34O6 |
| Molar mass | 430.541 g·mol−1 |
| 3D model (JSmol) | |
show
SMILES | |
show
InChI | |
| | |
Budesonide (BUD), sold under the brand name Pulmicort among others, is a medication of the corticosteroid type.[1] It is available as an inhaler, nebulization solution, pill, nasal spray, and rectal forms.[1][2] The inhaled form is used in the long-term management of asthma and chronic obstructive pulmonary disease (COPD).[1][3][4] The nasal spray is used for allergic rhinitis and nasal polyps.[2][5] The pills in a delayed release form and rectal forms may be used for inflammatory bowel disease including Crohn's disease, ulcerative colitis, and microscopic colitis.[6][7][8] Budesonide was approved in April 2021 by the UK's NHS to treat COVID-19 on a case-by-case basis.[9]
Common side effects with the inhaled form include respiratory infections, cough, and headaches.[1] Common side effects with the pills include feeling tired, vomiting, and joint pains.[1] Serious side effects include an increased risk of infection, loss of bone strength, and cataracts.[1] Long-term use of the pill form may cause adrenal insufficiency.[1] Stopping the pills suddenly following long-term use may therefore be dangerous.[1] The inhaled form is generally safe in pregnancy.[1] Budesonide chiefly acts as a glucocorticoid.[1]
Budesonide was initially patented in 1973.[10] Commercial use as an asthma medication began in 1981.[11] It is on the World Health Organization's List of Essential Medicines.[12] Some forms are available as a generic medication.[13] In 2019, generic budesonide was listed as involved in Teva's price fixing scheme in the United States.[14] In 2018, it was the 180th most commonly prescribed medication in the United States, with more than 3 million prescriptions.[15][16]
Medical uses[]
Asthma[]
Budesonide is given by metered-dose inhaler or nebulizer for maintenance and prophylactic treatment of asthma, including patients who require oral corticosteroids and those who may benefit from a systemic dose reduction.[17]
COVID-19[]
After a University of Oxford research team found in a trial with 1,700 patients that budesonide could benefit many people over 50 with COVID-19 symptoms, it was approved from 12 April 2021 by the National Health Service in the UK for general practitioners (GPs) to treat Covid on a case-by-case basis. Final results of the trial are expected in late April.[18][19]
Inhalational Budesonide has been part of the recommended treatment for mild covid cases in India since April 2021.[20][21]
Inflammatory bowel disease[]
Formulations of delayed-release budesonide are an effective treatment for mild-to-moderately active Crohn's disease involving the ileum and/or ascending colon.[22] A Cochrane review found evidence for up to three months (but not longer) of maintenance of remission in Crohn's disease.[23]
Budesonide assists in the induction of remission in people with active ulcerative colitis.[24]
Budesonide is highly effective and recommended as the drug of choice in microscopic colitis, for induction and maintenance of remission, and for both the lymphocytic colitis and collagenous colitis forms.[7]
Allergic rhinitis[]
Budesonide in the form of nasal sprays is a treatment for allergic rhinitis.[25]
Eosinophilic esophagitis[]
Topical budesonide has considerable effects in eosinophilic esophagitis.[26] For this use, it is formulated as a tablet that disperses in the mouth, and sold under the trade name Jorveza.[27]
Side effects[]
Nasal budesonide inhalers have been associated with a number of side effects.[28][29] These include nose irritation or burning, bleeding or sores in the nose, lightheadedness, upset stomach, cough, hoarseness, dry mouth, rash, sore throat, bad taste in mouth, change in mucus, and blurred vision.[30] Other symptoms which should be reported immediately include difficulty in breathing, swelling of the face, white patches in the throat, mouth, or nose, irregular menstrual periods, severe acne, and on rare occasions, behavioral changes (mostly affecting children)[28]
Contraindications[]
Budesonide is contraindicated as a primary treatment of status asthmaticus or other acute episode of asthma where intensive measures are required.[31] It is also contraindicated for patients who have hypersensitivity to budesonide.[32]
Interactions[]
Those taking tablets or capsules orally should avoid grapefruit and grapefruit juice[33][34] and echinacea.[35]: 160
- Grapefruit juice may double bioavailability of oral budesonide.[medical citation needed]
- Echinacea diminishes bioavailability.[medical citation needed]
Also, high-fat meals delay absorption but do not impede absorption.[36]
Pharmacology[]
Budesonide is an agonist of glucocorticoid receptors. Among its effects are:
- Controls the rate of protein synthesis.[37]
- Depresses the migration of polymorphonuclear leukocytes and fibroblasts.[38]
- Reverses capillary permeability and lysosomal stabilization at the cellular level to prevent or control inflammation.
- Has a potent glucocorticoid activity and weak mineralocorticoid activity.[medical citation needed]
Pharmacokinetics[]
- Onset of action: Nebulization: 2–8 days; Inhalation: 24 hours; Nasal: 10 hours
- Peak effect: Nebulization: 4–6 weeks; Inhalation: 1–2 weeks
- Distribution: 2.2-3.9 L/kg
- Protein binding: 85% to 90%
- Metabolism: Hepatic via CYP3A4 to two metabolites: and ; minor activity
- Bioavailability: Limited by high first-pass effect; Capsule: 9% to 21%; Nebulization: 6%; Inhalation: 6% to 13%
- Half-life elimination: 2–3.6 hours
- Time to peak: Capsule: 0.5–10 hours (variable in Crohn's disease); Nebulization: 10–30 minutes; Inhalation: 1–2 hours; Tablet: 7.4-19.2 hours
- Excretion: urine (60%) and feces as metabolites.[medical citation needed]
Chemistry[]
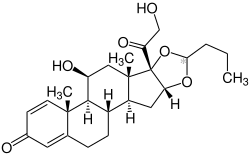
Budesonide, also known as 11β,21-dihydroxy-16α,17α-(butylidenebis(oxy))pregna-1,4-diene-3,20-dione, is a synthetic pregnane steroid and non-halogenated cyclic ketal corticosteroid.[39][40] It is the C16α hydroxyl, C16α,17α cyclic ketal with butyraldehyde derivative of prednisolone (11β,17α,21-trihydroxypregna-1,4-diene-3,20-dione).[39][40]
Stereoisomerism[]
| Budesonide (2 stereoisomers) | |
|---|---|
 (22R)-configuration |
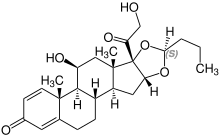 (22S)-configuration |
Society and culture[]
Brand names[]

Aeronide (TH); Aquacort (DE); B Cort (CO); Bronex (PH); Budair (MY); Budecort DP (MY); Budenofalk (DE, GB, HK, KP, PH, SG); Budeson (AR); Budeson Aqua (AR); BudeSpray (TH); Budiair (KP); Budicort Respules (IL); Budinide (KSA); Bunase (TH); Clebudan (CN); Cortiment (GB); Cycortide (HK); Denecort (PH); Duasma (TW); Eltair (MY); Entocort (AR, AT, BE, BR, CH, CZ, DK, FI, FR, GB, HK, IE, IL, IT, KP, NL, NO, PL, PT, SE, TR);[35]: 13 Giona Easyhaler (MY, SG, TH); Inflammide (PE); Miflonid (CZ); Miflonide (BE, DE, IL, IT, NZ, PT); Neumocort (PY); Novopulmon (DE, FR); Pulmicon Susp for Nebulizer (KP); Pulmicort (AT, BE, BG, BR, CH, CL, CN, CO, CR, CZ, DE, DK, DO, EE, FI, FR, GB, GR, GT, HN, ID, IN, NI, NL, NO, PA, PK, PL, PT, RU, SE, SV, TR, TW, UY, VE, ZA);[35]: 13 Pulmicort Nasal Turbohaler (CL, KE, MU, NG); Pulmicort Turbuhaler (KE, MU, NG); Rafton (FR); Rhinocort (AU); Rhinocort Aqua (HK);[41] Rhinoside (GR); Symbicort (FR, US, ZA) Uceris (US).
References[]
- ^ Jump up to: a b c d e f g h i j "Budesonide". The American Society of Health-System Pharmacists. Archived from the original on 28 November 2015. Retrieved 2 December 2015.
- ^ Jump up to: a b "Budesonide eent". The American Society of Health-System Pharmacists. Archived from the original on 8 December 2015. Retrieved 2 December 2015.
- ^ De Coster DA, Jones M (2014). "Tailoring of corticosteroids in COPD management". Current Respiratory Care Reports. 3 (3): 121–132. doi:10.1007/s13665-014-0084-2. PMC 4113685. PMID 25089228.
- ^ Christophi GP, Rengarajan A, Ciorba MA (2016). "Rectal budesonide and mesalamine formulations in active ulcerative proctosigmoiditis: efficacy, tolerance, and treatment approach". Clinical and Experimental Gastroenterology. 9: 125–30. doi:10.2147/CEG.S80237. PMC 4876845. PMID 27274301.
- ^ Rudmik L, Schlosser RJ, Smith TL, Soler ZM (July 2012). "Impact of topical nasal steroid therapy on symptoms of nasal polyposis: a meta-analysis". The Laryngoscope. 122 (7): 1431–7. doi:10.1002/lary.23259. PMID 22410935. S2CID 25637461.
- ^ Silverman J, Otley A (July 2011). "Budesonide in the treatment of inflammatory bowel disease". Expert Review of Clinical Immunology. 7 (4): 419–28. doi:10.1586/eci.11.34. PMID 21790284. S2CID 32892611.
- ^ Jump up to: a b Pardi DS, Tremaine WJ, Carrasco-Labra A (January 2016). "American Gastroenterological Association Institute Technical Review on the Medical Management of Microscopic Colitis". Gastroenterology. 150 (1): 247–274.e11. doi:10.1053/j.gastro.2015.11.006. PMID 26584602.
- ^ British national formulary: BNF 58 (58 ed.). British Medical Association. 2009. pp. 56–57. ISBN 9780857111562.
- ^ "CAS-ViewAlert". www.cas.mhra.gov.uk. Retrieved 16 April 2021.
- ^ Domeij B (2000). Pharmaceutical patents in Europe. The Hague: Kluwer Law International. p. 278. ISBN 9789041113481. Archived from the original on 8 December 2015.
- ^ Hamley P (2015). Small Molecule Medicinal Chemistry: Strategies and Technologies. John Wiley & Sons. p. 390. ISBN 9781118771693. Archived from the original on 8 December 2015.
- ^ World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ Hamilton R (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. p. 451. ISBN 9781284057560.
- ^ Murphy H (11 May 2019). "Teva and Other Generic Drugmakers Inflated Prices Up to 1,000%, State Prosecutors Say". The New York Times. ISSN 0362-4331. Retrieved 27 May 2020.
- ^ "The Top 300 of 2021". ClinCalc. Retrieved 18 February 2021.
- ^ "Budesonide - Drug Usage Statistics". ClinCalc. Retrieved 18 February 2021.
- ^ Global Strategy for Asthma Management and Prevention, Global Initiative for Asthma (GiNA) 2011. Available at https://www.ginasthma.org Archived 2013-10-14 at the Wayback Machine
- ^ Roxby, Philippa (12 April 2021). "Covid: Asthma drug 'speeds up recovery at home'". BBC News.
- ^ Blakely, Rhys (12 April 2021). "Asthma drug Budesonide speeds up Covid recovery times". The Times. ISSN 0140-0460.
- ^ "New guidelines prescribe inhaled steroid 'Budesonide', antiparasitic drug 'Ivermectin' for mild Covid cases". The New Indian Express. 29 April 2021. Retrieved 11 July 2021.
- ^ "Clinical Management Protocol for Covid-19 (in Adults)" (PDF). Ministry of Health and Family Welfare. 24 May 2021.
- ^ Lichtenstein GR, Hanauer SB, Sandborn WJ (2009). "Management of Crohn's Disease in Adults". Am J Gastroenterol. 104 (2): 465–83. doi:10.1038/ajg.2008.168. PMID 19174807. S2CID 10176441.
- ^ Kuenzig ME, Rezaie A, Seow CH, Otley AR, Steinhart AH, Griffiths AM, et al. (2014). "Budesonide for maintenance of remission in Crohn's disease". Cochrane Database Syst Rev. 8 (8): CD002913. doi:10.1002/14651858.CD002913.pub3. PMC 7133546. PMID 25141071.
- ^ Habal FM, Huang VW (2012). "Review Article: A Decision-Making Algorithm For the Management of Pregnancy in the Inflammatory Bowel Disease Patient". Aliment Pharmacol Ther. 35 (5): 501–15. doi:10.1111/j.1365-2036.2011.04967.x. PMID 22221203. S2CID 34662981.
- ^ Stanaland BE (April 2004). "Once-daily budesonide aqueous nasal spray for allergic rhinitis: a review". Clinical Therapeutics. 26 (4): 473–92. doi:10.1016/s0149-2918(04)90050-1. PMID 15189745.
- ^ Rawla P, Sunkara T, Thandra KC, Gaduputi V (December 2018). "Efficacy and Safety of Budesonide in the Treatment of Eosinophilic Esophagitis: Updated Systematic Review and Meta-Analysis of Randomized and Non-Randomized Studies". Drugs in R&D. 18 (4): 259–269. doi:10.1007/s40268-018-0253-9. PMC 6277325. PMID 30387081.
- ^ UK Drug Information
- ^ Jump up to: a b "GENERIC NAME: BUDESONIDE - NASAL AEROSOL INHALER (byou-DESS-oh-nide)". eMedicineHealth. Archived from the original on 6 November 2008.
- ^ "What are the possible side effects of budesonide nasal (Childrens Rhinocort Allergy, Rhinocort Allergy, Rhinocort Aqua)?". eMedicineHealth.
- ^ "Budesonide: CMDh scientific conclusions and grounds for variation, amendments to the product information and timetable for the implementation - PSUSA/00000449/201604" (PDF). European Medicines Agency (EMA). 10 March 2017. Archived (PDF) from the original on 8 September 2017. Retrieved 19 May 2017.
- ^ Todd GR, Acerini CL, Buck JJ, Murphy NP, Ross-Russell R, Warner JT, McCance DR (2002). "Acute Adrenal Crisis in Asthmatics Treated With High-Dose Fluticasone Propionate". Eur Respir J. 19 (6): 1207–9. doi:10.1183/09031936.02.00274402. PMID 12108877.
- ^ Todd GR, Acerini CL, Ross-Russell R, Zahra S, Warner JT, McCance D (2002). "Survey of Adrenal Crisis Associated With Inhaled Corticosteroids in the United Kingdom". Arch Dis Child. 87 (6): 457–61. doi:10.1136/adc.87.6.457. PMC 1755820. PMID 12456538.
- ^ Marshall JK (May 2014). "Topically Active Steroid Preparations". In Bayless TM, Hanauer SB (eds.). Advanced Therapy of Inflammatory Bowel Disease, volume 2: IBD and Crohn's Disease. PMPH-USA. p. 651. ISBN 978-1-60795-217-6.
- ^ Baily DG (2010). "Grapefruit and Other Fruit Juices Interactions with Medicines". In Boullata JI, Armenti VT (eds.). Handbook of drug-nutrient interactions (2nd ed.). New York, NY: Humana Press. p. 282. ISBN 978-1-60327-362-6.
- ^ Jump up to: a b c Kizior RJ, Hodgson BB (22 August 2014). Saunders Nursing Drug Handbook 2015 - E-Book. Elsevier Health Sciences. p. 160. ISBN 978-0-323-28018-1.
- ^ Taketomo CK, Hodding JH, Kraus DM (2009). Pediatric Dosage Handbook; Including Neonatal Dosing, Drug Administration & Extemporaneous Preparations. Lexi-Comp. ISBN 978-1-59195-267-1.
- ^ Kizior RJ, Hodgson BB (21 February 2018). Saunders Nursing Drug Handbook 2019 E-Book. Elsevier Health Sciences. p. 160. ISBN 978-0-323-61257-9.
- ^ Skidmore-Roth L, Richardson F (9 July 2020). Mosby's Canadian Nursing Drug Reference - E-Book. Elsevier Health Sciences. p. 187. ISBN 978-1-77172-084-7.
- ^ Jump up to: a b Elks J (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 186, 1011. ISBN 978-1-4757-2085-3. Archived from the original on 8 September 2017.
- ^ Jump up to: a b Lemke TL, Williams DA (2008). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 1253–. ISBN 978-0-7817-6879-5. Archived from the original on 8 September 2017.
- ^ Griffith HW (2014). Complete Guide to Prescription and Nonprescription Drugs 2015; Features an A-Z List of Conditions and the Drugs Most Commonly Used (2015 ed.). Penguin. ISBN 9780698165519.
External links[]
- "Budesonide". Drug Information Portal. U.S. National Library of Medicine.
- "Budesonide Nasal Spray". MedlinePlus.
- "Budesonide Oral Inhalation". MedlinePlus.
- Aldols
- Antiasthmatic drugs
- AstraZeneca brands
- Corticosteroid cyclic ketals
- Corticosteroids
- Cyclic acetals with aldehydes
- Diketones
- Diols
- Enones
- Glucocorticoids
- Pregnanes
- World Health Organization essential medicines
- Orphan drugs