Sleep deprivation
| Sleep deprivation | |
|---|---|
| Specialty | Sleep medicine |
| Symptoms | Not enough sleep, low-quality sleep, poor memory, fatigue |
| Complications | Car and work accidents, weight gain, cardiovascular disease |
| Causes | Insomnia, sleep apnea, voluntary imposition (school, work), mood disorders |
| Treatment | Sleep hygiene, talk therapy, caffeine (to induce alertness), sleeping pills |
Sleep deprivation, also known as sleep insufficiency or sleeplessness, is the condition of not having adequate duration and/or quality of sleep to support decent alertness, performance, and health. It can be either chronic or acute and may vary widely in severity.
Acute sleep deprivation is when an individual sleeps less than usual or does not sleep at all for a short period of time – usually lasting one to two days. Chronic sleep deprivation means when an individual routinely sleeps less than an optimal amount for ideal functioning. Chronic sleep deficiency is often confused with the term insomnia. Although both chronic sleep deficiency and insomnia share decreased quantity and/or quality of sleep as well as impaired function, their difference lies on the ability to fall asleep. Sleep deprived individuals are able to fall asleep rapidly when allowed but those suffering from insomnia have difficulty falling asleep.[1]
A chronic sleep-restricted state adversely affects the brain and cognitive function.[2] However, in a subset of cases, sleep deprivation can paradoxically lead to increased energy and alertness and enhanced mood; although its long-term consequences have never been evaluated, sleep deprivation has even been used as a treatment for depression.[3][4]
Few studies have compared the effects of acute total sleep deprivation and chronic partial sleep restriction.[2] A complete absence of sleep over a long period is not frequent in humans (unless they suffer from fatal insomnia or specific issues caused by surgery); it appears that brief microsleeps cannot be avoided.[5] Long-term total sleep deprivation has caused death in lab animals.[6]
Causes[]
Insomnia[]
Insomnia, one of the six types of dyssomnia, affects 21–37% of the adult population.[7][8] Many of its symptoms are easily recognizable, including excessive daytime sleepiness; frustration or worry about sleep; problems with attention, concentration, or memory; extreme mood changes or irritability; lack of energy or motivation; poor performance at school or work; and tension headaches or stomach aches.
Insomnia can be grouped into primary and secondary, or comorbid, insomnia.[9][10][11]
Primary insomnia is a sleep disorder not attributable to a medical, psychiatric, or environmental cause.[12] There are three main types of primary insomnia. These include: psychophysiological, idiopathic insomnia, and sleep state misperception (paradoxical insomnia).[9] Psychophysiological insomnia is anxiety-induced. Idiopathic insomnia generally begins in childhood and lasts the rest of a person's life. It's suggested that idiopathic insomnia is a neurochemical problem in a part of the brain that controls the sleep-wake cycle, resulting in either under-active sleep signals or over-active wake signals. Sleep state misperception is diagnosed when people get enough sleep but inaccurately perceive that their sleep is insufficient.[13][citation needed]
Secondary insomnia, or comorbid insomnia, occurs concurrently with other medical, neurological, psychological and psychiatric conditions. Causation is not necessarily implied.[14]
Sleep is known to be cumulative. This means that the fatigue and sleep one lost as a result, for example, staying awake all night, would be carried over to the following day. Not getting enough sleep a couple days cumulatively builds up a deficiency and that's when all the symptoms of sleep deprivation come in. A well rested and healthy individual will generally spend less time in the REM stage of sleep. Studies have shown an inverse relationship between time spent in the REM stage of sleep and subsequent wakefulness during waking hours.[15]
Sleep apnea[]
Obstructive sleep apnea is often caused by collapse of the upper airway during sleep, which reduces airflow to the lungs. Those who suffer from sleep apnea may experience symptoms such as awakening gasping or choking, restless sleep, morning headaches, morning confusion or irritability and restlessness. This disorder affects between 1 and 10 percent of Americans.[16] It has many serious health outcomes if untreated. Positive airway pressure therapy using a CPAP (Continuous positive airway pressure), APAP or BPAP devices is considered to be the first line treatment option for sleep apnea.[17] Mandibular displacement devices in some cases can reposition the jaw and tongue to prevent the airway from collapsing. For some patients supplemental oxygen therapy may be indicated. Nasal problems such as a deviated septum will shut down the airway and increase swelling in the mucus lining and nasal turbinates. Corrective surgery (septoplasty) in some cases may be an appropriate choice of treatment.
Central sleep apnea is caused by a failure of the central nervous system to signal the body to breathe during sleep. Treatments similar to obstructive sleep apnea may be used as well as other treatments such as Adaptive Servo Ventilation and certain medications. Some medications such as opioids may contribute to or cause central sleep apnea.[18]
Voluntary[]
Sleep deprivation can sometimes be self-imposed due to a lack of desire to sleep or the habitual use of stimulant drugs. Sleep deprivation is also self-imposed to achieve personal fame in the context of record-breaking stunts.
Mental illness[]
The specific causal relationships between sleep loss and effects on psychiatric disorders have been most extensively studied in patients with mood disorders.[medical citation needed] Shifts into mania in bipolar patients are often preceded by periods of insomnia,[19] and sleep deprivation has been shown to induce a manic state in about 30% of patients.[20] Sleep deprivation may represent a final common pathway in the genesis of mania,[21] and manic patients usually have a continuous reduced need for sleep.[22]
The symptoms of sleep deprivation and those of schizophrenia are paralleled, including those of positive and cognitive symptoms.[23]
School[]
The National Sleep Foundation cites a 1996 paper showing that college/university-aged students got an average of less than 6 hours of sleep each night.[24] A 2018 study highlights the need for a good night's sleep for students finding that college students who averaged eight hours of sleep for the five nights of finals week scored higher on their final exams than those who didn't.[25]
In the study, 70.6% of students reported obtaining less than 8 hours of sleep, and up to 27% of students may be at risk for at least one sleep disorder.[26] Sleep deprivation is common in first year college students as they adjust to the stress and social activities of college life.
A study performed by the Department of Psychology at the National Chung Cheng University in Taiwan concluded that freshmen received the least amount of sleep during the week.[27]
Studies of later start times in schools have consistently reported benefits to adolescent sleep, health and learning using a wide variety of methodological approaches. In contrast, there are no studies showing that early start times have any positive impact on sleep, health or learning.[28] "Astronomical" data from international studies demonstrate that "synchronised" start times for adolescents are far later than the start times in the overwhelming majority of educational institutions.[29] In 1997, University of Minnesota research compared students who started school at 7:15 am with those who started at 8:40 am. They found that students who started at 8:40 got higher grades and more sleep on weekday nights than those who started earlier.[30] One in four U.S. high school students admits to falling asleep in class at least once a week.[31]
It is known that during human adolescence, circadian rhythms and therefore sleep patterns typically undergo marked changes. Electroencephalogram (EEG) studies indicate a 50% reduction of deep (stage 4) sleep and a 75% reduction in the peak amplitude of delta waves during NREM sleep in adolescence. School schedules are often incompatible with a corresponding delay in sleep offset, leading to a less than optimal amount of sleep for the majority of adolescents.[32]
Hospital stay[]
A study performed nationwide in the Netherlands found that general ward patients staying at the hospital experienced shorter total sleep (83 min. less), more night-time awakenings, and earlier awakenings compared to sleeping at home. Over 70% experienced being woken up by external causes, such as hospital staff (35.8%). Sleep disturbing factors included noise of other patients, medical devices, pain, and toilet visits.[33] Sleep deprivation is even more severe in ICU patients, where the naturally occurring nocturnal peak of melatonin secretion was found to be absent, possibly causing the disruption in the normal sleep-wake cycle.[34] However, as the personal characteristics and the clinical picture of hospital patients are so diverse, the possible solutions to improve sleep and circadian rhythmicity should be tailored to the individual and within the possibilities of the hospital ward. Multiple interventions could be considered to aid patient characteristics, improve hospital routines, or the hospital environment.[35]
Internet[]
A study published in the Journal of Economic Behavior and Organisation found out that the broadband internet connection was associated with sleep deprivation. The study concluded that the people with a broadband connection tend to sleep 25 minutes less than those without the broadband connection, hence they are less likely to get the scientifically recommended 7–9 hours of sleep.[36] Another study conducted on 435 non-medical staff at King Saud University Medical City reported that 9 out of 10 of the respondents used their smartphones at bedtime, with social media being the most used service (80.5%). The study found participants who spent more than 60 minutes using their smartphones at bedtime were 7.4 times more likely to have poor sleep quality than participants who spent less than 15 minutes.[37]
Effects and consequences[]
Brain[]
One study suggested, based on neuroimaging, that 35 hours of total sleep deprivation in healthy controls negatively affected the brain's ability to put an emotional event into the proper perspective and make a controlled, suitable response to the event.[38]
The negative effects of sleep deprivation on alertness and cognitive performance suggest decreases in brain activity and function. These changes primarily occur in two regions: the thalamus, a structure involved in alertness and attention; and the prefrontal cortex, a region sub-serving alertness, attention, and higher-order cognitive processes.[39] This was the finding of an American study in 2000. Seventeen men in their 20s were tested. Sleep deprivation was progressive with measurements of glucose (absolute regional CMRglu), cognitive performance, alertness, mood, and subjective experiences collected after 0, 24, 48, and 72 hours of sleep deprivation. Additional measures of alertness, cognitive performance, and mood were collected at fixed intervals. PET scans were used and attention was paid to the circadian rhythm of cognitive performance.[39]
A noted 2002 University of California animal study indicated that non-rapid eye movement sleep (NREM) is necessary for turning off neurotransmitters and allowing their receptors to "rest" and regain sensitivity which allows monoamines (norepinephrine, serotonin and histamine) to be effective at naturally produced levels. This leads to improved regulation of mood and increased learning ability. The study also found that rapid eye movement sleep (REM) deprivation may alleviate clinical depression because it mimics selective serotonin reuptake inhibitors (SSRIs). This is because the natural decrease in monoamines during REM is not allowed to occur, which causes the concentration of neurotransmitters in the brain, that are depleted in clinically depressed persons, to increase. Sleep outside of the REM phase may allow enzymes to repair brain cell damage caused by free radicals. High metabolic activity while awake damages the enzymes themselves preventing efficient repair. This study observed the first evidence of brain damage in rats as a direct result of sleep deprivation.[40]
Animal studies suggest that sleep deprivation increases levels of stress hormones, which may reduce new cell production in adult brains.[41]
Attention and working memory[]
Among the possible physical consequences of sleep deprivation, deficits in attention and working memory are perhaps the most important;[2] such lapses in mundane routines can lead to unfortunate results, from forgetting ingredients while cooking to missing a sentence while taking notes. Performing tasks that require attention appears to be correlated with number of hours of sleep received each night, declining as a function of hours of sleep deprivation.[42] Working memory is tested by methods such as choice-reaction time tasks.[2]
The attentional lapses also extend into more critical domains in which the consequences can be life-or-death; car crashes and industrial disasters can result from inattentiveness attributable to sleep deprivation. To empirically measure the magnitude of attention deficits, researchers typically employ the psychomotor vigilance task (PVT) which requires the subject to press a button in response to a light at random intervals. Failure to press the button in response to the stimulus (light) is recorded as an error, attributable to the microsleeps that occur as a product of sleep deprivation.[43]
Crucially, individuals' subjective evaluations of their fatigue often do not predict actual performance on the PVT. While totally sleep-deprived individuals are usually aware of the degree of their impairment, lapses from chronic (lesser) sleep deprivation can build up over time so that they are equal in number and severity to the lapses occurring from total (acute) sleep deprivation. Chronically sleep-deprived people, however, continue to rate themselves considerably less impaired than totally sleep-deprived participants.[44] Since people usually evaluate their capability on tasks like driving subjectively, their evaluations may lead them to the false conclusion that they can perform tasks that require constant attention when their abilities are in fact impaired.
Mood[]
Sleep deprivation can have a negative impact on mood. Staying up all night or taking an unexpected night shift can make one feel irritable. Once one catches up on sleep, one's mood will often return to baseline or normal. Even partial sleep deprivation can have a significant impact on mood. In one study, subjects reported increased sleepiness, fatigue, confusion, tension, and total mood disturbance, which all recovered to their baseline after one to two full nights of sleep.[45][46]
Depression and sleep are in a bidirectional relationship. Poor sleep can lead to development of depression and depression can cause insomnia, hypersomnia, or obstructive sleep apnea.[47][48] About 75% of adult patients with depression can present with insomnia.[49] Sleep deprivation, whether total or not, can induce significant anxiety and longer sleep deprivations tend to result in increased level of anxiety.[50]
Sleep deprivation has also shown some positive effects on mood, and can be used to treat depression.[4] Chronotype can affect how sleep deprivation influences mood. Those with morningness (advanced sleep period or "lark") preference become more depressed after sleep deprivation while those with eveningness (delayed sleep period or "owl") preference show an improvement in mood.[51]
Mood and mental states can affect sleep as well. Increased agitation and arousal from anxiety or stress can keep one more aroused, awake, and alert.[45]
Driving ability[]
The dangers of sleep deprivation are apparent on the road; the American Academy of Sleep Medicine (AASM) reports that one in every five serious motor vehicle injuries is related to driver fatigue, with 80,000 drivers falling asleep behind the wheel every day and 250,000 accidents every year related to sleep,[52] though the National Highway Traffic Safety Administration suggests the figure for traffic accidents may be closer to 100,000.[30] The AASM recommends pulling off the road and taking a 15- or 20-minute nap to alleviate drowsiness.[52]
According to a 2000 study published in the British Medical Journal, researchers in Australia and New Zealand reported that sleep deprivation can have some of the same hazardous effects as being drunk.[53] People who drove after being awake for 17–19 hours performed worse than those with a blood alcohol level of 0.05 percent, which is the legal limit for drunk driving in most western European countries and Australia. Another study suggested that performance begins to degrade after 16 hours awake, and 21 hours awake was equivalent to a blood alcohol content of 0.08 percent, which is the blood alcohol limit for drunk driving in Canada, the U.S., and the U.K.[54]
Fatigue of drivers of goods trucks and passenger vehicles have come to the attention of authorities in many countries, where specific laws have been introduced with the aim of reducing the risk of traffic accidents due to driver fatigue. Rules concerning minimum break lengths, maximum shift lengths and minimum time between shifts are common in the driving regulations used in different countries and regions, such as the drivers' working hours regulations in the European Union and hours of service regulations in the United States.
The Exxon Valdez Oil Spill was the second largest oil spill in the United States. This accident occurred when an Exxon oil tanker struck a reef at the Prince William Sound in Alaska. Approximately 10.8 million gallons of oil spilled into the sea. The accident caused great environmental damage including the death of hundreds of thousands of birds and sea creatures. Fatigue and sleep deprivation were the major contributors to the accident. The captain of the ship was asleep after a night of heavy drinking; he was severely fatigued and had been awake for 18 hours. The entire crew was suffering from fatigue and inadequate sleep.[55]
Sleep transition[]
Sleep propensity (SP) can be defined as the readiness to transit from wakefulness to sleep, or the ability to stay asleep if already sleeping.[56] Sleep deprivation increases this propensity, which can be measured by polysomnography (PSG), as a reduction in sleep latency (the time needed to fall asleep).[57] An indicator of sleep propensity can also be seen in the shortening of transition from light stages of non-REM sleep to deeper slow-waves oscillations can also be measured as indicator of sleep propensity.[57]
On average, the latency in healthy adults decreases by a few minutes after a night without sleep, and the latency from sleep onset to slow-wave sleep is halved.[57] Sleep latency is generally measured with the multiple sleep latency test (MSLT). In contrast, the maintenance of wakefulness test (MWT) also uses sleep latency, but this time as a measure of the capacity of the participants to stay awake (when asked to) instead of falling asleep.[57]
Sleep-wake cycle[]
Research studying sleep deprivation shows its impact on mood, cognitive and motor functioning, due to dysregulation of the sleep-wake cycle and augmented sleep propensity.[57] Multiple studies that identified the role of the hypothalamus and multiple neural systems controlling circadian rhythms and homeostasis have been helpful in understanding sleep deprivation better.[57][58] To describe the temporal course of the sleep-wake cycle, the two-process model of sleep regulation can be mentioned.[57]
This model proposes a homeostatic process (Process S) and a circadian process (Process C) that interact to define the time and intensity of sleep.[59] Process S represents the drive for sleep, increasing during wakefulness and decreasing during sleep, until a defined threshold level, while Process C is the oscillator responsible for these levels. When being sleep deprived, homeostatic pressure accumulates to the point that waking functions will be degraded even at the highest circadian drive for wakefulness.[57][59]
Microsleeps[]
Microsleeps occur when a person has a significant sleep deprivation. Microsleeps usually last for a few seconds and happen most frequently when a person is trying to stay awake when they are feeling sleepy.[60] The person usually falls into microsleep while doing a monotonous task like driving, reading a book, or staring at a computer.[61] Microsleeps are similar to blackouts and a person experiencing them is not consciously aware that they are occurring.
An even lighter type of sleep has been seen in rats that have been kept awake for long periods of time. In a process known as local sleep, specific localized brain regions went into periods of short (~80 ms) but frequent (~40/min) NREM-like states. Despite the on and off periods where neurons shut off, the rats appeared to be awake, although they performed poorly at tests.[62]
Cardiovascular morbidity[]
Decreased sleep duration is associated with many adverse cardiovascular consequences.[63][64][65][66] The American Heart Association has stated that sleep restriction is a risk factor for adverse cardiometabolic profiles and outcomes. The organization recommends healthy sleep habits for ideal cardiac health along with other well known factors like blood pressure, cholesterol, diet, glucose, weight, smoking, and physical activity.[67] The Centers for Disease Control and Prevention has noted that adults who sleep less than 7 hours per day are more likely to have chronic health conditions including heart attack, coronary heart disease, and stroke compared to those with adequate amount of sleep.[68]
In a study that followed over 160,000 healthy, non-obese adults, the subjects who self-reported sleep duration less than 6 hours a day were at an increased risk for developing multiple cardiometabolic risk factors. They presented with increased central obesity, elevated fasting glucose, hypertension, low high-density lipoprotein, hypertriglyceridemia, and metabolic syndrome. The presence or lack of insomnia symptoms did not modify the effects of sleep duration in this study.[69]
The United Kingdom Biobank studied nearly 500,000 adults who had no cardiovascular disease, and the subjects who slept less than 6 hours a day were associated with a 20 percent increase in the risk of developing myocardial infarction (MI) over 7 years of follow-up period. Interestingly, long sleep duration of more than 9 hours a night was also a risk factor.[70]
Immunosuppression[]
Among the myriad of health consequences that sleep deprivation can cause, disruption of the immune system is one of them. While it is not clearly understood, researchers believe that sleep is essential to providing sufficient energy for the immune system to work and allow inflammation to take place during sleep. Also, just as sleep can reinforce memory in a person's brain, it can help consolidate the memory of the immune system or adaptive immunity.[71][72]
An adequate amount of sleep improves effects of vaccines that utilize adaptive immunity. When vaccines expose the body to a weakened or deactivated antigen, the body initiates an immune response. The immune system learns to recognize that antigen and attacks it when exposed again in the future. Studies have found that people who don't sleep the night after getting a vaccine were less likely to develop a proper immune response to the vaccine and sometimes even required a second dose. People who are sleep deprived in general also do not provide their bodies with sufficient time for an adequate immunological memory to form, and thus, can fail to benefit from vaccination.[71]
People who sleep less than 6 hours a night are more prone to infection and are more likely to catch a cold or flu. A lack of sleep can also prolong the recovery time in patients in intensive care unit (ICU).[71][73][74]
Weight gain[]
A lack of sleep can cause an imbalance in several hormones that are critical in weight gain. Sleep deprivation increases the level of ghrelin (hunger hormone) and decreases the level of leptin (fullness hormone), resulting in an increased feeling of hunger and desire for high-calorie foods.[75][76][77] Sleep loss is also associated with decreased growth hormone and elevated cortisol levels, which are connected to obesity. People who do not get sufficient sleep can also feel sleepy and fatigued during the day and get less exercise. Obesity can cause poor sleep quality as well. Individuals who are overweight or obese can experience obstructive sleep apnea, gastroesophageal reflux disease (GERD), depression, asthma, and osteoarthritis which all can disrupt a good night's sleep.[78]
In rats, prolonged, complete sleep deprivation increased both food intake and energy expenditure with a net effect of weight loss and ultimately death.[79] This study hypothesizes that the moderate chronic sleep debt associated with habitual short sleep is associated with increased appetite and energy expenditure with the equation tipped towards food intake rather than expenditure in societies where high-calorie food is freely available.[80]
Type 2 diabetes[]
It has been suggested that people experiencing short-term sleep restrictions process glucose more slowly than individuals receiving a full 8 hours of sleep, increasing the likelihood of developing type 2 diabetes.[81] Poor sleep quality is linked to high blood sugar levels in diabetic and prediabetic patients but the causal relationship is not clearly understood. Researchers suspect that sleep deprivation affects insulin, cortisol, and oxidative stress, which subsequently influence blood sugar levels. Sleep deprivation can increase the level of ghrelin and decrease the level of leptin. People who get insufficient amount of sleep are more likely to crave food in order to compensate for the lack of energy. This habit can raise blood sugar and put them at risk of obesity and diabetes.[82]
In 2005, a study of over 1400 participants showed that participants who habitually slept few hours were more likely to have associations with type 2 diabetes.[83] However, because this study was merely correlational, the direction of cause and effect between little sleep and diabetes is uncertain. The authors point to an earlier study which showed that experimental rather than habitual restriction of sleep resulted in impaired glucose tolerance (IGT).[84]
Other effects[]
The National Sleep Foundation identifies several warning signs that a driver is dangerously fatigued. These include rolling down the window, turning up the radio, trouble keeping eyes open, head-nodding, drifting out of their lane, and daydreaming. At particular risk are lone drivers between midnight and 6:00am.[85]
Sleep deprivation can negatively impact overall performance, and has led to major fatal accidents. Due largely to the February 2009 crash of Colgan Air Flight 3407, which killed 50 people and was partially attributed to pilot fatigue, the FAA reviewed its procedures to ensure that pilots are sufficiently rested. Air traffic controllers were under scrutiny when in 2010 there were 10 incidents of controllers falling asleep while on shift. The common practice of turn-around shifts caused sleep deprivation and was a contributing factor to all air traffic control incidents. The FAA reviewed its practices of shift changes and the findings saw that controllers were not well rested.[86] A 2004 study also found medical residents with less than four hours of sleep a night made more than twice as many errors as the 11% of surveyed residents who slept for more than seven hours a night.[87]
Twenty-four hours of continuous sleep deprivation results in the choice of less difficult math tasks without decreases in subjective reports of effort applied to the task. Naturally caused sleep loss affects the choice of everyday tasks such that low effort tasks are mostly commonly selected. Adolescents who experience less sleep show a decreased willingness to engage in sports activities that require effort through fine motor coordination and attention to detail.[88][89]
Great sleep deprivation mimics psychosis: distorted perceptions can lead to inappropriate emotional and behavioral responses.[90]
Astronauts have reported performance errors and decreased cognitive ability during periods of extended working hours and wakefulness as well as due to sleep loss caused by circadian rhythm disruption and environmental factors.[91]
One study has found that a single night of sleep deprivation may cause tachycardia (in the following day).[92]
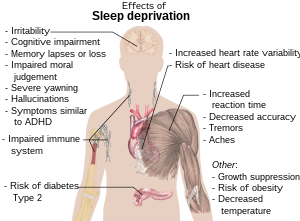
Generally, sleep deprivation may facilitate or intensify:[93]
- aching muscles[94]
- confusion, memory lapses or loss[95]
- depression[95]
- development of false memory
- hypnagogic and hypnopompic hallucinations during falling asleep and waking, which are entirely normal[96]
- hand tremor[97]
- headaches
- malaise
- stye
- periorbital puffiness, commonly known as "bags under eyes" or eye bags
- increased blood pressure[98]
- increased stress hormone levels[98]
- increased risk of Type 2 diabetes[98]
- lowering of immunity, increased susceptibility to illness[99]
- increased risk of fibromyalgia[100]
- irritability[93]
- nystagmus (rapid involuntary rhythmic eye movement)[101]
- obesity[98]
- seizures[102]
- temper tantrums in children[93]
- violent behavior[103]
- yawning[93]
- mania[104]
- Sleep inertia[105]
- symptoms similar to:
Assessment[]
Patients suffering from sleep deprivation may present with complaints of symptoms and signs of insufficient sleep such as fatigue, sleepiness, drowsy driving, and cognitive difficulties. Sleep insufficiency can easily go unrecognized and undiagnosed unless patients are specifically asked about it by their clinicians.[109]
Several questions are critical in evaluating sleep duration and quality, as well as the cause of sleep deprivation. Sleep patterns (typical bed time or rise time on weekdays and weekends), shift work, and frequency of naps can reveal the direct cause of poor sleep, and quality of sleep should be discussed to rule out any diseases such as obstructive sleep apnea and restless leg syndrome.[109]
Sleep diaries are useful in providing detailed information about sleep patterns. They are inexpensive, readily available, and easy to use. The diaries can be as simple as a 24-hour log to note the time of being asleep or can be detailed to include other relevant information.[110][111] Sleep questionnaires such as the Sleep Timing Questionnaire (STQ) can be used instead of sleep diaries if there is any concern for patient adherence.[112]
Actigraphy is a useful, objective wrist-worn tool if the validity of self-reported sleep diaries or questionnaires is questionable. Actigraphy works by recording movements and using computerized algorithms to estimate total sleep time, sleep onset latency, the amount of wake after sleep onset, and sleep efficiency. Some devices have light sensors to detect light exposure.[113][114][115][116]
Management[]
Although there are numerous causes of sleep deprivation, there are some fundamental measures that promote quality sleep as suggested by organizations such as Centers for Disease Control and Prevention, the National Institute of Health, the National Institute of Aging, and the American Academy of Family Physicians. The key is to implement healthier sleep habits, also known as sleep hygiene.[117] Sleep hygiene recommendations include setting a fixed sleep schedule, taking naps with caution, maintaining a sleep environment that promotes sleep (cool temperature, limited exposure to light and noise, comfortable mattress and pillows), exercising daily, avoiding alcohol, cigarettes, caffeine, and heavy meals in the evening, winding down and avoiding electronic use or physical activities close to bedtime, and getting out of bed if unable to fall asleep.[118]
For long term involuntary sleep deprivation, cognitive behavioral therapy for Insomnia (CBT-i) is commonly recommended as a first-line treatment, after exclusion of physical diagnosis (f.e. sleep apnea). CBT-i contains five different components: cognitive therapy, stimulus control, sleep restriction, sleep hygiene, and relaxation. These components together have shown to be effective in adults, with clinical meaningful effect sizes. As this approach has minimal adverse effects, and long-term benefits, it is often preferred to (chronic) drug therapy.[119]
There are several strategies that help increase alertness and counteract the effects of sleep deprivation. Caffeine is often used over short periods to boost wakefulness when acute sleep deprivation is experienced; however, caffeine is less effective if taken routinely.[120] Other strategies recommended by the American Academy of Sleep Medicine include prophylactic sleep before deprivation, naps, other stimulants, and combinations thereof. However, the only sure and safe way to combat sleep deprivation is to increase nightly sleep time.[121]
Uses[]
To facilitate abusive control[]
Sleep deprivation can be used to disorientate abuse victims to help set them up for abusive control.[122][123]
Interrogation[]
Sleep deprivation can be used as a means of interrogation, which has resulted in court trials over whether or not the technique is a form of torture.[124]
Under one interrogation technique, a subject might be kept awake for several days and when finally allowed to fall asleep, suddenly awakened and questioned. Menachem Begin, the Prime Minister of Israel from 1977 to 1983, described his experience of sleep deprivation as a prisoner of the NKVD in Soviet Union as follows:
In the head of the interrogated prisoner, a haze begins to form. His spirit is wearied to death, his legs are unsteady, and he has one sole desire: to sleep... Anyone who has experienced this desire knows that not even hunger and thirst are comparable with it.[125]
Sleep deprivation was one of the five techniques used by the British government in the 1970s. The European Court of Human Rights ruled that the five techniques "did not occasion suffering of the particular intensity and cruelty implied by the word torture ... [but] amounted to a practice of inhuman and degrading treatment", in breach of the European Convention on Human Rights.[126]
The United States Justice Department released four memos in August 2002 describing interrogation techniques used by the Central Intelligence Agency. They first described 10 techniques used in the interrogation of Abu Zubaydah, described as a terrorist logistics specialist, including sleep deprivation. Memos signed by Steven G. Bradbury in May 2005 claimed that forced sleep deprivation for up to 180 hours (7+1⁄2 days)[127][128] by shackling a diapered prisoner to the ceiling did not constitute torture,[129] nor did the combination of multiple interrogation methods (including sleep deprivation) constitute torture under United States law.[130][131] These memoranda were repudiated and withdrawn during the first months of the Obama administration.[127]
The question of extreme use of sleep deprivation as torture has advocates on both sides of the issue. In 2006, Australian Federal Attorney-General Philip Ruddock argued that sleep deprivation does not constitute torture.[132] Nicole Bieske, a spokeswoman for Amnesty International Australia, has stated the opinion of her organization thus: "At the very least, sleep deprivation is cruel, inhumane and degrading. If used for prolonged periods of time it is torture."[133]
Treating depression[]
Studies show that sleep restriction has some potential in treating depression.[4] Those who suffer from depression tend to have earlier occurrences of REM sleep with an increased number of rapid eye movements; therefore, monitoring patients' EEG and awakening them during occurrences of REM sleep appear to have a therapeutic effect, alleviating depressive symptoms.[134] This kind of treatment is known as wake therapy. Although as many as 60% of patients show an immediate recovery when sleep-deprived, most patients relapse the following night. The effect has been shown to be linked to an increase in the brain-derived neurotrophic factor (BDNF).[135] A comprehensive evaluation of the human metabolome in sleep deprivation in 2014 found that 27 metabolites are increased after 24 waking hours and suggested serotonin, tryptophan, and taurine may contribute to the antidepressive effect.[136]
The incidence of relapse can be decreased by combining sleep deprivation with medication or a combination of light therapy and phase advance (going to bed substantially earlier than one's normal time).[137][138] Many tricyclic antidepressants suppress REM sleep, providing an additional evidence for a link between mood and sleep.[139] Similarly, tranylcypromine has been shown to completely suppress REM sleep at adequate doses.
Treating insomnia[]
Sleep deprivation can be implemented for a short period of time in the treatment of insomnia. Some common sleep disorders have been shown to respond to cognitive behavioral therapy for insomnia. One of the components is a controlled regime of "sleep restriction" in order to restore the homeostatic drive to sleep and encourage normal "sleep efficiency".[140] The main goal of stimulus control and sleep restriction therapy is to create an association between bed and sleep. Although sleep restriction therapy shows efficacy when applied as an element of cognitive-behavioral therapy, its efficacy is yet to be proven when used alone.[141][119]
Changes in American sleep habits[]
The examples and perspective in this section may not represent a worldwide view of the subject. (December 2010) |
National Geographic Magazine has reported that the demands of work, social activities, and the availability of 24-hour home entertainment and Internet access have caused people to sleep less now than in premodern times.[142] USA Today reported in 2007 that most adults in the USA get about an hour less than the average sleep time 40 years ago.[143]
Other researchers have questioned these claims. A 2004 editorial in the journal Sleep stated that according to the available data, the average number of hours of sleep in a 24-hour period has not changed significantly in recent decades among adults. Furthermore, the editorial suggests that there is a range of normal sleep time required by healthy adults, and many indicators used to suggest chronic sleepiness among the population as a whole do not stand up to scientific scrutiny.[144]
A comparison of data collected from the Bureau of Labor Statistics' American Time Use Survey from 1965–1985 and 1998–2001 has been used to show that the median amount of sleep, napping, and resting done by the average adult American has changed by less than 0.7%, from a median of 482 minutes per day from 1965 through 1985, to 479 minutes per day from 1998 through 2001.[145][146]
Longest periods without sleep[]
Randy Gardner holds the scientifically documented record for the longest period of time a human being has intentionally gone without sleep not using stimulants of any kind. Gardner stayed awake for 264 hours (11 days), breaking the previous record of 260 hours held by Tom Rounds of Honolulu.[90] LCDR John J. Ross of the U.S. Navy Medical Neuropsychiatric Research Unit later published an account of this event, which became well known among sleep-deprivation researchers.[90][147][148]
The Guinness World Record stands at 449 hours (18 days, 17 hours), held by Maureen Weston, of Peterborough, Cambridgeshire in April 1977, in a rocking-chair marathon.[147]
Claims of total sleep deprivation lasting years have been made several times,[149][150][151] but none are scientifically verified.[152] Claims of partial sleep deprivation are better documented. For example, Rhett Lamb of St. Petersburg, Florida was initially reported to not sleep at all, but actually had a rare condition permitting him to sleep only one to two hours per day in the first three years of his life. He had a rare abnormality called an Arnold–Chiari malformation where brain tissue protrudes into the spinal canal and the skull puts pressure on the protruding part of the brain. The boy was operated on at All Children's Hospital in St. Petersburg in May 2008. Two days after surgery he slept through the night.[153][154]
French sleep expert Michel Jouvet and his team reported the case of a patient who was quasi-sleep-deprived for four months, as confirmed by repeated polygraphic recordings showing less than 30 minutes (of stage-1 sleep) per night, a condition they named "agrypnia". The 27-year-old man was suffering from Morvan's fibrillary chorea, a rare disease that leads to involuntary movements, and in this particular case, extreme insomnia. The researchers found that treatment with 5-HTP restored almost normal sleep stages. However some months after this recovery the patient died during a relapse which was unresponsive to 5-HTP. The cause of death was pulmonary edema. Despite the extreme insomnia, psychological investigation showed no sign of cognitive deficits, except for some hallucinations.[155]
Fatal insomnia is a neurodegenerative disease eventually resulting in a complete inability to go past stage 1 of NREM sleep. In addition to insomnia, patients may experience panic attacks, paranoia, phobias, hallucinations, rapid weight loss, and dementia. Death usually occurs between 7 and 36 months from onset.
See also[]
- Insomnia
- Effects of sleep deprivation on cognitive performance
- Narcolepsy
- Polyphasic sleep
- Sleep medicine
- Sleep onset latency
- Wake therapy
- Tony Wright, who claims to hold the world record for sleep deprivation
- Foreign Correspondent, a 1940 film depicting interrogation by sleep deprivation
References[]
- ^ International Classification of Sleep Disorders (3 ed.). Darien, IL: American Academy of Sleep Medicine. 2014.
- ^ Jump up to: a b c d Alhola, Paula; Päivi Polo-Kantola (October 2007). "Sleep deprivation: Impact on cognitive performance". Neuropsychiatr. Dis. Treat. 3 (5): 553–567. PMC 2656292. PMID 19300585.
Although both conditions [total and partial SD] induce several negative effects including impairments in cognitive performance, the underlying mechanisms seem to be somewhat different.
- ^ Nykamp K, Rosenthal L, Folkerts M, Roehrs T, Guido P, Roth, T (September 1998). "The effects of REM sleep deprivation on the level of sleepiness/alertness". Sleep. 21 (6): 609–614. doi:10.1093/sleep/21.6.609. PMID 9779520.
- ^ Jump up to: a b c Riemann D, Berger M, Voderholzer U (July–August 2001). "Sleep and depression - results from psychobiological studies: an overview". Biological Psychology. 57 (1–3): 67–103. doi:10.1016/s0301-0511(01)00090-4. PMID 11454435. S2CID 31725861.
- ^ Kushida (2005). Sleep deprivation. Informa Health Care. pp. 1–2. ISBN 978-0-8247-5949-0.
- ^ Rechtschaffen A, Bergmann B (1995). "Sleep deprivation in the rat by the disk-over-water method". Behavioural Brain Research. 69 (1–2): 55–63. doi:10.1016/0166-4328(95)00020-T. PMID 7546318. S2CID 4042505.
- ^ Morphy, Hannah; Dunn, Kate M.; Lewis, Martyn; Boardman, Helen F.; Croft, Peter R. (2007). "Epidemiology of Insomnia: a Longitudinal Study in a UK Population". Sleep. 30 (3): 274–80. PMID 17425223. Archived from the original on 22 December 2015. Retrieved 13 December 2015.
- ^ Kim, K; Uchiyama, M; Okawa, M; Liu, X; Ogihara, R (1 February 2000). "An epidemiological study of insomnia among the Japanese general population". Sleep. 23 (1): 41–7. doi:10.1093/sleep/23.1.1a. PMID 10678464.
- ^ Jump up to: a b "Dyssomnias" (PDF). WHO. pp. 7–11. Archived (PDF) from the original on 18 March 2009. Retrieved 25 January 2009.
- ^ Buysse, Daniel J. (2008). "Chronic Insomnia". Am. J. Psychiatry. 165 (6): 678–86. doi:10.1176/appi.ajp.2008.08010129. PMC 2859710. PMID 18519533.
For this reason, the NIH conference [of 2005] commended the term "comorbid insomnia" as a preferable alternative to the term "secondary insomnia."
- ^ Erman, Milton K. (2007). "Insomnia: Comorbidities and Consequences". Primary Psychiatry. 14 (6): 31–35. Archived from the original on 15 July 2011.
Two general categories of insomnia exist, primary insomnia and comorbid insomnia.
- ^ World Health Organization (2007). "Quantifying burden of disease from environmental noise" (PDF). p. 20. Archived (PDF) from the original on 23 November 2010. Retrieved 22 September 2010.
- ^ Chunhua L, Hongzhong Q (15 June 2017). "Paradoxical Insomnia: Misperception of Sleep Can Be a Tormenting Experience". American Family Physician. 95 (12): 770. PMID 28671423. Retrieved 10 May 2020.
- ^ Biological Rhythms, Sleep and Hypnosis by Simon Green
- ^ Plaford, Gary R. (2009). Sleep and learning : the magic that makes us healthy and smart. Lanham. ISBN 9781607090915. OCLC 310224798.
- ^ Zammit, Gary K. (1997). Good nights : how to stop sleep deprivation, overcome insomnia, and get the sleep you need. Zanca, Jane A. Kansas City: Andrews and McMeel. ISBN 0-8362-2188-5. OCLC 35849087.
- ^ Spicuzza L, Caruso D, Di Maria G. Obstructive sleep apnoea syndrome and its management. Therapeutic Advances in Chronic Disease. 2015;6(5):273-285. doi:10.1177/2040622315590318.
- ^ Muza RT (2015). "Central sleep apnoea—a clinical review". Journal of Thoracic Disease. 7 (5): 930–937. doi:10.3978/j.issn.2072-1439.2015.04.45. PMC 4454847. PMID 26101651.
- ^ McKenna BS, Eyler LT (November 2012). "Overlapping prefrontal systems involved in cognitive and emotional processing in euthymic bipolar disorder and following sleep deprivation: a review of functional neuroimaging studies". Clin Psychol Rev. 32 (7): 650–663. doi:10.1016/j.cpr.2012.07.003. PMC 3922056. PMID 22926687.
- ^ Young, JW; Dulcis, D (15 July 2015). "Investigating the mechanism(s) underlying switching between states in bipolar disorder". European Journal of Pharmacology. 759: 151–62. doi:10.1016/j.ejphar.2015.03.019. PMC 4437855. PMID 25814263.
- ^ Wehr, TA (1987). "Sleep reduction as a final common pathway in the genesis of mania". Am. J. Psychiatry. 144 (2): 201–204. doi:10.1176/ajp.144.2.201. PMID 3812788.
- ^ American Psychiatry Association (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington: American Psychiatric Publishing. pp. 123–154. ISBN 978-0-89042-555-8.
- ^ Pocivavsek, A; Rowland, LM (13 January 2018). "Basic Neuroscience Illuminates Causal Relationship Between Sleep and Memory: Translating to Schizophrenia". Schizophrenia Bulletin. 44 (1): 7–14. doi:10.1093/schbul/sbx151. PMC 5768044. PMID 29136236.
- ^ "National Sleep Foundation Key Messages/Talking Points" (PDF). Archived (PDF) from the original on 18 April 2016. Retrieved 18 April 2016.
- ^ Schroeder, Jackson (7 December 2018). "Students Who Sleep 8 Hours Score Higher On Final Exams". The University Network. Retrieved 10 December 2018.
- ^ Shelley D Hershner; Ronald D Chervin (23 June 2014). "Causes and consequences of sleepiness among college students". Nature and Science of Sleep. 6: 73–84. doi:10.2147/NSS.S62907. PMC 4075951. PMID 25018659.
- ^ Tsai LL, Li SP; Li (2004). "Sleep patterns in college students; Gender and grade differences". J. Psychosom. Res. 56 (2): 231–7. doi:10.1016/S0022-3999(03)00507-5. PMID 15016583. Archived from the original on 20 December 2008.
- ^ Kelley, Paul; Lockley, Steven; Foster, Russel; Kelley, Jonathan (1 August 2014). "Synchronizing education to adolescent biology: 'let teens sleep, start school later'". Learning, Media and Technology. 40 (2): 220. doi:10.1080/17439884.2014.942666.
- ^ Kelley, P.; Lockley, S. W. (27 April 2013). "Synchronizing Education to Healthy Adolescent Brain Development: Sleep and Circadian Rhythms". Cite journal requires
|journal=(help) - ^ Jump up to: a b Carpenter, Siri (2001). "Sleep deprivation may be undermining teen health". Monitor on Psychology. 32 (9): 42. Archived from the original on 6 October 2006.
- ^ Randolph E. Schmid (28 March 2006). "Sleep-deprived teens dozing off at school". ABC News. Associated Press. Archived from the original on 8 December 2006.
- ^ Giedd JN (October 2009). "Linking adolescent sleep, brain maturation, and behavior". Journal of Adolescent Health. 45 (4): 319–320. doi:10.1016/j.jadohealth.2009.07.007. PMC 3018343. PMID 19766933.
- ^ Wesselius, Hilde M.; van den Ende, Eva S.; Alsma, Jelmer; ter Maaten, Jan C.; Schuit, Stephanie C. E.; Stassen, Patricia M.; de Vries, Oscar J.; Kaasjager, Karin H. A. H.; Haak, Harm R.; van Doormaal, Frederiek F.; Hoogerwerf, Jacobien J. (1 September 2018). "Quality and Quantity of Sleep and Factors Associated With Sleep Disturbance in Hospitalized Patients". JAMA Internal Medicine. 178 (9): 1201–1208. doi:10.1001/jamainternmed.2018.2669. ISSN 2168-6106. PMC 6142965. PMID 30014139.
- ^ Shilo, L.; Dagan, Y.; Smorjik, Y.; Weinberg, U.; Dolev, S.; Komptel, B.; Balaum, H.; Shenkman, L. (May 1999). "Patients in the Intensive Care Unit Suffer from Severe Lack of Sleep Associated with Loss of Normal Melatonin Secretion Pattern". The American Journal of the Medical Sciences. 317 (5): 278–281. doi:10.1016/s0002-9629(15)40528-2. ISSN 0002-9629. PMID 10334113.
- ^ Tan, Xiao; van Egmond, Lieve; Partinen, Markku; Lange, Tanja; Benedict, Christian (1 July 2019). "A narrative review of interventions for improving sleep and reducing circadian disruption in medical inpatients". Sleep Medicine. 59: 42–50. doi:10.1016/j.sleep.2018.08.007. ISSN 1389-9457. PMID 30415906.
- ^ "Broadband internet causes sleep deprivation, a new study finds". ScienceDaily. Retrieved 10 August 2018.
- ^ Alshobaili, Fahdah; AlYousefi, Nada (26 June 2019). "The effect of smartphone usage at bedtime on sleep quality among Saudi non- medical staff at King Saud University Medical City". J Family Med Prim Care. 8 (6): 1953–1957. doi:10.4103/jfmpc.jfmpc_269_19. PMC 6618184. PMID 31334161. Retrieved 18 August 2021.
- ^ Yoo, Seung-Schik; Gujar, Ninad; Hu, Peter; Jolesz, Ferenc; Walker, Matthew (2007). "The human emotional brain without sleep- a prefrontal amygdala disconnect". Current Biology. 17 (20): R877–R878. doi:10.1016/j.cub.2007.08.007. PMID 17956744. S2CID 9008816.
- ^ Jump up to: a b Thomas, M., Sing, H., Belenky, G., Holcomb, H., Mayberg, H., Dannals, R., Wagner JR., H., Thorne, D., Popp, K., Rowland, L., Welsh, A., Balwinski, S. and Redmond, D. (2000). "Neural basis of alertness and cognitive performance impairments during sleepiness. I. Effects of 24 h of sleep deprivation on waking human regional brain activity". Journal of Sleep Research. 9 (4): 335–52. doi:10.1046/j.1365-2869.2000.00225.x. PMID 11123521. S2CID 35893889.CS1 maint: multiple names: authors list (link)
- ^ Siegel, Jerome M. (November 2003). "Why We Sleep" (PDF). Scientific American. Archived (PDF) from the original on 3 December 2008. Retrieved 3 April 2008.
- ^ No sleep means no new brain cells Archived 11 February 2007 at the Wayback Machine. BBC (10 February 2007)
- ^ Kolb, Bryan; Whishaw, Ian (2014). An Introduction to Brain and Behavior (4th ed.). New York, New York: Worth Publishers. pp. 468–469. ISBN 9781429242288.
- ^ Innes, Carrie R. H.; Poudel, Govinda R.; Jones, Richard D. (1 November 2013). "Efficient and Regular Patterns of Nighttime Sleep are Related to Increased Vulnerability to Microsleeps Following a Single Night of Sleep Restriction". Chronobiology International. 30 (9): 1187–1196. doi:10.3109/07420528.2013.810222. ISSN 0742-0528. PMID 23998288. S2CID 4682794.
- ^ Van Dongen HA (2002). "The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation" (PDF). Sleep. 26 (2): 117–26. doi:10.1093/sleep/26.2.117. PMID 12683469. Archived (PDF) from the original on 18 July 2011.
- ^ Jump up to: a b "Sleep and Mood | Need Sleep". healthysleep.med.harvard.edu. Retrieved 21 January 2021.
- ^ Dinges, D. F.; Pack, F.; Williams, K.; Gillen, K. A.; Powell, J. W.; Ott, G. E.; Aptowicz, C.; Pack, A. I. Date=April 1997 (1997). "Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4-5 hours per night". Sleep. 20 (4): 267–277. ISSN 0161-8105. PMID 9231952.
- ^ "Depression and Sleep". Sleep Foundation. Retrieved 21 January 2021.
- ^ Franzen, Peter L.; Buysse, Daniel J. (2008). "Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications". Dialogues in Clinical Neuroscience. 10 (4): 473–481. doi:10.31887/DCNS.2008.10.4/plfranzen. ISSN 1294-8322. PMC 3108260. PMID 19170404.
- ^ Nutt, David; Wilson, Sue; Paterson, Louise (2008). "Sleep disorders as core symptoms of depression". Dialogues in Clinical Neuroscience. 10 (3): 329–336. doi:10.31887/DCNS.2008.10.3/dnutt. ISSN 1294-8322. PMC 3181883. PMID 18979946.
- ^ Pires, Gabriel Natan; Bezerra, Andreia Gomes; Tufik, Sergio; Andersen, Monica Levy (August 2016). "Effects of acute sleep deprivation on state anxiety levels: a systematic review and meta-analysis". Sleep Medicine. 24: 109–118. doi:10.1016/j.sleep.2016.07.019. ISSN 1878-5506. PMID 27810176.
- ^ Selvi, Yavuz; Mustafa Gulec; Mehmet Yucel Agargun; Lutfullah Besiroglu (2007). "Mood changes after sleep deprivation in morningness–eveningness chronotypes in healthy individuals" (PDF). Journal of Sleep Research. 16 (3): 241–4. doi:10.1111/j.1365-2869.2007.00596.x. PMID 17716271. S2CID 42338269. Archived (PDF) from the original on 15 December 2014.
- ^ Jump up to: a b "Drowsy Driving Fact Sheet" (PDF). American Academy of Sleep Medicine. 2 December 2009. Archived (PDF) from the original on 18 July 2011.
- ^ Williamson AM, Feyer AM (2000). "Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication". Occup. Environ. Med. 57 (10): 649–55. doi:10.1136/oem.57.10.649. PMC 1739867. PMID 10984335.
- ^ Dawson, Drew; Kathryn Reid (1997). "Fatigue, alcohol and performance impairment". Nature. 388 (6639): 235. Bibcode:1997Natur.388..235D. doi:10.1038/40775. PMID 9230429. S2CID 4424846.
- ^ ProQuest 2092623770
- ^ Schulz, H., Bes, E., Jobert, M. (1997). Modelling Sleep Propensity and Sleep Disturbances. In: Meier-Ewert K., Okawa M. (eds) Sleep—Wake Disorders. Springer. doi:10.1007/978-1-4899-0245-0_2
- ^ Jump up to: a b c d e f g h Durmer JS, Dinges DF (2005). "Neurocognitive Consequences of Sleep Deprivation". Semin Neurol. 25 (1): 117–129. doi:10.1055/s-2005-867080. PMC 3564638. PMID 15798944.
- ^ Saper CB, Chou TC, Scammell TE (2001). "The sleep switch: hypothalamic control of sleep and wakefulness". Trends Neurosci. 24 (12): 726–731. doi:10.1016/S0166-2236(00)02002-6. PMID 11718878. S2CID 206027570.
- ^ Jump up to: a b Borbély AA, Daan S, Wirz-Justice A (2016). "The two‐process model of sleep regulation: a reappraisal". J Sleep Res. 25 (2): 131–143. doi:10.1111/jsr.12371. PMID 26762182.
- ^ "Glossary K-M". Get Sleep. Harvard Medical School. 2012. Archived from the original on 2 April 2015.
- ^ "Microsleep | Microsleeps". www.sleepdex.org. Archived from the original on 3 March 2016. Retrieved 14 February 2016.
- ^ Vyazovskiy VV, Olcese U, Hanlon EC, Nir Y, Cirelli C, Tononi G (2011). "Local sleep in awake rats". Nature. 472 (7344): 443–447. Bibcode:2011Natur.472..443V. doi:10.1038/nature10009. PMC 3085007. PMID 21525926.
- ^ "CDC - Sleep and Chronic Disease - Sleep and Sleep Disorders". www.cdc.gov. 13 February 2019. Retrieved 21 January 2021.
- ^ Knutson, Kristen L.; Van Cauter, Eve; Rathouz, Paul J.; Yan, Lijing L.; Hulley, Stephen B.; Liu, Kiang; Lauderdale, Diane S. (8 June 2009). "Association between sleep and blood pressure in midlife: the CARDIA sleep study". Archives of Internal Medicine. 169 (11): 1055–1061. doi:10.1001/archinternmed.2009.119. ISSN 1538-3679. PMC 2944774. PMID 19506175.
- ^ King, Christopher Ryan; Knutson, Kristen L.; Rathouz, Paul J.; Sidney, Steve; Liu, Kiang; Lauderdale, Diane S. (24 December 2008). "Short sleep duration and incident coronary artery calcification". JAMA. 300 (24): 2859–2866. doi:10.1001/jama.2008.867. ISSN 1538-3598. PMC 2661105. PMID 19109114.
- ^ Sabanayagam, Charumathi; Shankar, Anoop (August 2010). "Sleep duration and cardiovascular disease: results from the National Health Interview Survey". Sleep. 33 (8): 1037–1042. doi:10.1093/sleep/33.8.1037. ISSN 0161-8105. PMC 2910533. PMID 20815184.
- ^ St-Onge, Marie-Pierre; Grandner, Michael A.; Brown, Devin; Conroy, Molly B.; Jean-Louis, Girardin; Coons, Michael; Bhatt, Deepak L. (1 November 2016). "Sleep Duration and Quality: Impact on Lifestyle Behaviors and Cardiometabolic Health: A Scientific Statement From the American Heart Association". Circulation. 134 (18): e367–e386. doi:10.1161/CIR.0000000000000444. ISSN 1524-4539. PMC 5567876. PMID 27647451.
- ^ "CDC - Data and Statistics - Sleep and Sleep Disorders". www.cdc.gov. 5 March 2019. Retrieved 21 January 2021.
- ^ Deng, Han-Bing; Tam, Tony; Zee, Benny Chung-Ying; Chung, Roger Yat-Nork; Su, Xuefen; Jin, Lei; Chan, Ta-Chien; Chang, Ly-Yun; Yeoh, Eng-Kiong; Lao, Xiang Qian (1 October 2017). "Short Sleep Duration Increases Metabolic Impact in Healthy Adults: A Population-Based Cohort Study". Sleep. 40 (10). doi:10.1093/sleep/zsx130. ISSN 1550-9109. PMID 28977563.
- ^ Daghlas, Iyas; Dashti, Hassan S.; Lane, Jacqueline; Aragam, Krishna G.; Rutter, Martin K.; Saxena, Richa; Vetter, Céline (10 September 2019). "Sleep Duration and Myocardial Infarction". Journal of the American College of Cardiology. 74 (10): 1304–1314. doi:10.1016/j.jacc.2019.07.022. ISSN 1558-3597. PMC 6785011. PMID 31488267.
- ^ Jump up to: a b c "Sleep & Immunity: Can a Lack of Sleep Make You Sick?". Sleep Foundation. Retrieved 21 January 2021.
- ^ Irwin, Michael R. (November 2019). "Sleep and inflammation: partners in sickness and in health". Nature Reviews. Immunology. 19 (11): 702–715. doi:10.1038/s41577-019-0190-z. ISSN 1474-1741. PMID 31289370. S2CID 195847558.
- ^ Prather, Aric A.; Janicki-Deverts, Denise; Hall, Martica H.; Cohen, Sheldon (1 September 2015). "Behaviorally Assessed Sleep and Susceptibility to the Common Cold". Sleep. 38 (9): 1353–1359. doi:10.5665/sleep.4968. ISSN 1550-9109. PMC 4531403. PMID 26118561.
- ^ Pisani, Margaret A.; Friese, Randall S.; Gehlbach, Brian K.; Schwab, Richard J.; Weinhouse, Gerald L.; Jones, Shirley F. (1 April 2015). "Sleep in the intensive care unit". American Journal of Respiratory and Critical Care Medicine. 191 (7): 731–738. doi:10.1164/rccm.201411-2099CI. ISSN 1535-4970. PMC 5447310. PMID 25594808.
- ^ Van Cauter E, Spiegel K (1999). "Sleep as a mediator of the relationship between socioeconomic status and health: a hypothesis". Ann. N. Y. Acad. Sci. 896 (1): 254–61. Bibcode:1999NYASA.896..254V. doi:10.1111/j.1749-6632.1999.tb08120.x. PMID 10681902. S2CID 36513336.
- ^ Taheri, Shahrad; Lin, Ling; Austin, Diane; Young, Terry; Mignot, Emmanuel (2004). "Short Sleep Duration Is Associated with Reduced Leptin, Elevated Ghrelin, and Increased Body Mass Index". PLOS Medicine. 1 (3): e62. doi:10.1371/journal.pmed.0010062. PMC 535701. PMID 15602591.
- ^ Taheri S, Lin L, Austin D, Young T, Mignot E (December 2004). "Short Sleep Duration Is Associated with Reduced Leptin, Elevated Ghrelin, and Increased Body Mass Index". PLOS Med. 1 (3): e62. doi:10.1371/journal.pmed.0010062. PMC 535701. PMID 15602591.
- ^ "The Link Between Obesity and Sleep Deprivation". Sleep Foundation. Retrieved 21 January 2021.
- ^ Everson CA, Bergmann BM, Rechtschaffen A (February 1989). "Sleep deprivation in the rat: III. Total sleep deprivation". Sleep. 12 (1): 13–21. doi:10.1093/sleep/12.1.13. PMID 2928622.
- ^ Taheri S, Lin L, Austin D, Young T, Mignot E (December 2004). "Short Sleep Duration Is Associated with Reduced Leptin, Elevated Ghrelin, and Increased Body Mass Index". PLOS Med. 1 (3): e62. doi:10.1371/journal.pmed.0010062. PMC 535701. PMID 15602591.
- ^ "Sleep and Disease Risk". Healthy Sleep. Harvard Medical School. 2007. Archived from the original on 25 March 2016.
- ^ "Diabetes and Sleep: Sleep Disturbances & Coping". Sleep Foundation. Retrieved 21 January 2021.
- ^ Gottlieb DJ, Punjabi NM, Newman AB (April 2005). "Association of sleep time with diabetes mellitus and impaired glucose tolerance". Arch. Intern. Med. 165 (8): 863–7. doi:10.1001/archinte.165.8.863. PMID 15851636.
- ^ Spiegel, K.; R. Leproult; E. Van Cauter (23 October 1999). "Impact of sleep debt on metabolic and endocrine function". The Lancet. 354 (9188): 1435–9. doi:10.1016/S0140-6736(99)01376-8. PMID 10543671. S2CID 3854642.
- ^ "Drowsy Driving:Key Messages and Talking Points" (PDF). National Sleep Foundation. 2 December 2009. Archived (PDF) from the original on 26 November 2013.
- ^ "Fact Sheet – Pilot Fatigue". Federal Aviation Administration. 10 September 2010. Archived from the original on 5 October 2016.
- ^ Baldwinn, DeWitt C. Jr.; Steven R. Daugherty (2004). "Sleep Deprivation and Fatigue in Residency Training: Results of a National Survey of First- and Second-Year Residents". Sleep. 27 (2): 217–223. doi:10.1093/sleep/27.2.217. PMID 15124713.
- ^ Engle-Friedman, Mindy; Suzanne Riela; Rama Golan; Ana M. Ventuneac2; Christine M. Davis1; Angela D. Jefferson; Donna Major (June 2003). "The effect of sleep loss on next day effort". Journal of Sleep Research. 12 (2): 113–124. doi:10.1046/j.1365-2869.2003.00351.x. PMID 12753348. S2CID 13519528.
- ^ Engle Friedman, Mindy; Palencar, V; Riela, S (2010). "Sleep and effort in adolescent athletes". J. Child Health Care. 14 (2): 131–41. doi:10.1177/1367493510362129. PMID 20435615. S2CID 7680316.
- ^ Jump up to: a b c Coren, Stanley (1 March 1998). "Sleep Deprivation, Psychosis and Mental Efficiency". Psychiatric Times. 15 (3). Archived from the original on 4 September 2009. Retrieved 25 November 2009.
- ^ Whitmire, A.M.; Leveton, L.B; Barger, L.; Brainard, G.; Dinges, D.F.; Klerman, E.; Shea, C. "Risk of Performance Errors due to Sleep Loss, Circadian Desynchronization, Fatigue, and Work Overload" (PDF). Human Health and Performance Risks of Space Exploration Missions: Evidence reviewed by the NASA Human Research Program. Archived (PDF) from the original on 15 February 2012. Retrieved 25 June 2012.
- ^ Rangaraj VR, Knutson KL (February 2016). "Association between sleep deficiency and cardiometabolic disease: implications for health disparities". Sleep Med. 18: 19–35. doi:10.1016/j.sleep.2015.02.535. PMC 4758899. PMID 26431758.
- ^ Jump up to: a b c d e "Sleep deprivation". betterhealth.vic.gov.au. Archived from the original on 20 August 2009.
- ^ Morin, Charles M. (2003). Insomnia. New York: Kluwer Academic/Plenum Publ. p. 28 death. ISBN 978-0-306-47750-8.
- ^ Jump up to: a b National Institute of Neurological Disorders and Stroke – Brain Basics: Understanding Sleep Archived 11 October 2007 at the Wayback Machine. ninds.nih.gov
- ^ Jump up to: a b Ohayon, M.M.; R.G. Priest; M. Caulet; C. Guilleminault (October 1996). "Hypnagogic and hypnopompic hallucinations: pathological phenomena?". British Journal of Psychiatry. 169 (4): 459–67. doi:10.1192/bjp.169.4.459. PMID 8894197. Retrieved 21 October 2006.
- ^ Smith, Andrew P. (1992). Handbook of Human Performance. London: Acad. Press. p. 240. ISBN 978-0-12-650352-4.
- ^ Jump up to: a b c d "Harvard Heart Letter examines the costs of not getting enough sleep – Harvard Health Publications". Health.harvard.edu. 31 May 2012. Archived from the original on 9 May 2011. Retrieved 13 August 2012.
- ^ Olson, Eric (9 June 2015). "Lack of sleep: Can it make you sick?". Mayo Clinic. Retrieved 26 August 2018.
- ^ "The Role of Magnesium in Fibromyalgia". Web.mit.edu. Archived from the original on 29 July 2012. Retrieved 13 August 2012.
- ^ Citek, K; Ball, B; Rutledge, DA (2003). "Nystagmus testing in intoxicated individuals" (PDF). Optometry. 74 (11): 695–710. PMID 14653658. Archived from the original (PDF) on 16 July 2011.
- ^ Engel, Jerome; Pedley, Timothy A.; Aicardi, Jean (2008). Epilepsy: A Comprehensive Textbook - Google Books. ISBN 9780781757775. Retrieved 30 January 2015.
- ^ Vaughn, Michael G.; Salas-Wright, Christopher P.; White, Norman A.; Kremer, Kristen P. (2015). "Poor sleep and reactive aggression: Results from a national sample of African American adults". Journal of Psychiatric Research. 66–67: 54–59. doi:10.1016/j.jpsychires.2015.04.015. PMID 25940021.
- ^ T A Wehr (1 October 1991). "Sleep-loss as a possible mediator of diverse causes of mania". British Journal of Psychiatry. Bjp.rcpsych.org. 159 (4): 576–578. doi:10.1192/bjp.159.4.576. PMID 1751874.
- ^ "Sleep deprivation - Better Health Channel". 20 August 2009. Archived from the original on 20 August 2009. Retrieved 24 October 2019.
- ^ Neural Link Between Sleep Loss And Psychiatric Disorders Archived 28 February 2009 at the Wayback Machine. ts-si.org (24 October 2007)
- ^ Chan-Ob, T.; V. Boonyanaruthee (September 1999). "Meditation in association with psychosis". Journal of the Medical Association of Thailand. 82 (9): 925–930. PMID 10561951.
- ^ Devillieres, P.; M. Opitz; P. Clervoy; J. Stephany (May–June 1996). "Delusion and sleep deprivation". L'Encéphale. 22 (3): 229–31. PMID 8767052.
- ^ Jump up to: a b "UpToDate". www.uptodate.com. Retrieved 28 January 2021.
- ^ Carney, Colleen E.; Buysse, Daniel J.; Ancoli-Israel, Sonia; Edinger, Jack D.; Krystal, Andrew D.; Lichstein, Kenneth L.; Morin, Charles M. (1 February 2012). "The consensus sleep diary: standardizing prospective sleep self-monitoring". Sleep. 35 (2): 287–302. doi:10.5665/sleep.1642. ISSN 1550-9109. PMC 3250369. PMID 22294820.
- ^ "Sleep Deprivation: Causes, Symptoms, & Treatment". Sleep Foundation. Retrieved 21 January 2021.
- ^ Monk, Timothy H.; Buysse, Daniel J.; Kennedy, Kathy S.; Pods, Jaime M.; DeGrazia, Jean M.; Miewald, Jean M. (15 March 2003). "Measuring sleep habits without using a diary: the sleep timing questionnaire". Sleep. 26 (2): 208–212. doi:10.1093/sleep/26.2.208. ISSN 0161-8105. PMID 12683481.
- ^ "Actigraphy". stanfordhealthcare.org. Retrieved 21 January 2021.
- ^ Morgenthaler, Timothy; Alessi, Cathy; Friedman, Leah; Owens, Judith; Kapur, Vishesh; Boehlecke, Brian; Brown, Terry; Chesson, Andrew; Coleman, Jack; Lee-Chiong, Teofilo; Pancer, Jeffrey (April 2007). "Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007". Sleep. 30 (4): 519–529. doi:10.1093/sleep/30.4.519. ISSN 0161-8105. PMID 17520797.
- ^ Smith, Michael T.; McCrae, Christina S.; Cheung, Joseph; Martin, Jennifer L.; Harrod, Christopher G.; Heald, Jonathan L.; Carden, Kelly A. (15 July 2018). "Use of Actigraphy for the Evaluation of Sleep Disorders and Circadian Rhythm Sleep-Wake Disorders: An American Academy of Sleep Medicine Clinical Practice Guideline". Journal of Clinical Sleep Medicine. 14 (7): 1231–1237. doi:10.5664/jcsm.7230. ISSN 1550-9397. PMC 6040807. PMID 29991437.
- ^ Smith, Michael T.; McCrae, Christina S.; Cheung, Joseph; Martin, Jennifer L.; Harrod, Christopher G.; Heald, Jonathan L.; Carden, Kelly A. (15 July 2018). "Use of Actigraphy for the Evaluation of Sleep Disorders and Circadian Rhythm Sleep-Wake Disorders: An American Academy of Sleep Medicine Systematic Review, Meta-Analysis, and GRADE Assessment". Journal of Clinical Sleep Medicine. 14 (7): 1209–1230. doi:10.5664/jcsm.7228. ISSN 1550-9397. PMC 6040804. PMID 29991438.
- ^ "How to Sleep Better". Sleep Foundation. Retrieved 14 January 2021.
- ^ "CDC - Sleep Hygiene Tips - Sleep and Sleep Disorders". www.cdc.gov. 13 February 2019. Retrieved 21 April 2020.
- ^ Jump up to: a b Trauer, James M.; Qian, Mary Y.; Doyle, Joseph S.; Rajaratnam, Shantha M.W.; Cunnington, David (4 August 2015). "Cognitive Behavioral Therapy for Chronic Insomnia: A Systematic Review and Meta-analysis". Annals of Internal Medicine. 163 (3): 191–204. doi:10.7326/M14-2841. ISSN 0003-4819. PMID 26054060. S2CID 21617330.
- ^ "Sleep Deprivation" (PDF). American Academy of Sleep Medicine. 2008. Archived (PDF) from the original on 26 February 2015. Retrieved 25 March 2015.
- ^ "Sleep Deprivation Fact Sheet" (PDF). American Academy of Sleep Medicine. 2 December 2009. Archived (PDF) from the original on 26 February 2015.
- ^ Sleep Deprivation Used as Abuse Tactic
- ^ Family and Domestic Violence - Healthy Work Healthy Living Tip Sheet
- ^ "Binyam Mohamed torture appeal lost by UK government..." BBC News. 2 October 2009. Archived from the original on 11 February 2010.
- ^ Begin, Menachem (1979). White nights: the story of a prisoner in Russia. San Francisco: Harper & Row. ISBN 978-0-06-010289-0.
- ^ Ireland v. the United Kingdom Archived 14 May 2011 at the Wayback Machine paragraph 102
- ^ Jump up to: a b Miller, Greg; Meyer, Josh (17 April 2009). "Obama assures intelligence officials they won't be prosecuted over interrogations". Los Angeles Times. Retrieved 10 July 2016.
- ^ Bradbury, Steven G. (10 May 2005). "Memorandum for John Rizzo" (PDF). ACLU. p. 14. Archived from the original (PDF) on 6 November 2011. Retrieved 24 October 2011.
- ^ Scherer, Michael (21 April 2009). "Scientists Claim CIA Misused Work on Sleep Deprivation". Time. Retrieved 2 February 2017.
- ^ "Explaining and Authorizing Specific Interrogation Techniques". The New York Times. 17 April 2009. Archived from the original on 19 October 2017.
- ^ Department of Justice Office of Professional Responsibility (29 July 2009). Investigation into the Office of Legal Counsel's Memoranda Concerning Issues Relating to the Central Intelligence Agency's Use of "Enhanced Interrogation Techniques" on Suspected Terrorists (PDF) (Report). United States Department of Justice. pp. 133–138. Retrieved 29 May 2017.
- ^ Hassan T (3 October 2006). "Sleep deprivation remains red-hot question". PM. abc.net.au. Archived from the original on 11 October 2007.
- ^ "Sleep deprivation is torture: Amnesty". The Sydney Morning Herald. AAP. 3 October 2006. Archived from the original on 27 October 2007.
- ^ Carlson, Neil (2013). Physiology of Behavior (11th ed.). Boston: Pearson. pp. 578–579. ISBN 9780205239399.
- ^ Gorgulu Y, Caliyurt O; Caliyurt (September 2009). "Rapid antidepressant effects of sleep deprivation therapy correlates with serum BDNF changes in major depression". Brain Res. Bull. 80 (3): 158–62. doi:10.1016/j.brainresbull.2009.06.016. PMID 19576267. S2CID 7672556.
- ^ Davies, S. K.; Ang, J. E.; Revell, V. L.; Holmes, B; Mann, A; Robertson, F. P.; Cui, N; Middleton, B; Ackermann, K; Kayser, M; Thumser, A. E.; Raynaud, F. I.; Skene, D. J. (22 July 2014). "Effect of sleep deprivation on the human metabolome". Proc Natl Acad Sci USA. 111 (29): 10761–6. Bibcode:2014PNAS..11110761D. doi:10.1073/pnas.1402663111. PMC 4115565. PMID 25002497.
- ^ Wirz-Justice A, Van den Hoofdakker RH; Van Den Hoofdakker (August 1999). "Sleep deprivation in depression: what do we know, where do we go?". Biol. Psychiatry. 46 (4): 445–53. doi:10.1016/S0006-3223(99)00125-0. PMID 10459393. S2CID 15428567.
- ^ WIRZ-JUSTICE, ANNA; BENEDETTI, FRANCESCO; BERGER, MATHIAS; LAM, RAYMOND W.; MARTINY, KLAUS; TERMAN, MICHAEL; WU, JOSEPH C. (10 March 2005). "Chronotherapeutics (light and wake therapy) in affective disorders". Psychological Medicine. 35 (7): 939–944. doi:10.1017/S003329170500437X. PMID 16045060.
- ^ Disorders That Disrupt Sleep (Parasomnias) Archived 22 December 2005 at the Wayback Machine. eMedicineHealth
- ^ Miller, CB; et al. (October 2014). "The evidence base of sleep restriction therapy for treating insomnia disorder". Sleep Medicine Reviews. 18 (5): 415–24. doi:10.1016/j.smrv.2014.01.006. PMID 24629826.
- ^ Miller, Christopher B.; Espie, Colin A.; Epstein, Dana R.; Friedman, Leah; Morin, Charles M.; Pigeon, Wilfred R.; Spielman, Arthur J.; Kyle, Simon D. (October 2014). "The evidence base of sleep restriction therapy for treating insomnia disorder". Sleep Medicine Reviews. 18 (5): 415–424. doi:10.1016/j.smrv.2014.01.006. PMID 24629826.
- ^ "U.S. Racking Up Huge "Sleep Debt"" Archived 10 December 2006 at the Wayback Machine, National Geographic Magazine, 24 February 2005
- ^ Fackelmann, Kathleen (25 November 2007). "Study: Sleep deficit may be impossible to make up". USA Today. Archived from the original on 28 June 2012.
- ^ Horne, Jim (September 2004). "Is there a sleep debt?". Sleep. 27 (6): 1047–9. PMID 15532195.
- ^ "National Time Use Studies (1965–1985)". umd.edu. Archived from the original on 7 September 2006.
- ^ "National Time Use Studies (1998 - 2001)". umd.edu. Archived from the original on 7 September 2006.
- ^ Jump up to: a b Alex Boese (5 November 2007). "Eleven days awake". Elephants on Acid: And Other Bizarre Experiments. Harvest Books. pp. 90–93. ISBN 978-0-15-603135-6. Archived from the original on 19 September 2014.
- ^ Ross J (1965). "Neurological Findings After Prolonged Sleep Deprivation". Archives of Neurology. 12 (4): 399–403. doi:10.1001/archneur.1965.00460280069006. PMID 14264871.
- ^ Thao, Vu Phuong. "Vietnam man handles three decades without sleep". Thanh Nien Daily. Vietnam National Youth Federation. Archived from the original on 13 May 2008. Retrieved 26 May 2008.
- ^ "Ukrainian man has been lacking sleep for 20 years". 15 January 2005. Archived from the original on 5 October 2016. Retrieved 5 October 2016.
- ^ Dan Childs (30 March 2009). "11 Baffling Medical Conditions". ABC News. The Boy Who Couldn't Sleep.
- ^ "Matters of dispute – Sleepless in Ukraine". The Guardian. 10 February 2005. Archived from the original on 4 March 2014. Retrieved 11 May 2010.
- ^ "Boy, 3, Sleeps for First Time After Experimental Surgery". FoxNews.com. 16 May 2008. Archived from the original on 5 October 2016.
- ^ Canning, Andrea (23 January 2009). "Mystery of Sleepless Boy Solved: Boy Who Couldn't Sleep Undergoes Risky, Life-Changing Operation". ABC News.
- ^ Fischer-Perroudon C, Mouret J, Jouvet M (1974). "One case of agrypnia (4 months without sleep) in a morvan disease, favourable action of 5-hydroxytryptophane". Electroencephalography and Clinical Neurophysiology. 36 (1): 1–18. doi:10.1016/0013-4694(74)90132-1. PMID 4128428. Archived from the original on 30 January 2011.
- Sleep medicine
- Sleeplessness and sleep deprivation
- Nursing diagnoses
- Psychological torture techniques
- Physical torture techniques
- Disorders causing seizures
