Fallopian tube
This article needs additional citations for verification. (October 2021) |
This article's lead section may be too short to adequately summarize the key points. (March 2015) |
| Fallopian tube | |
|---|---|
 Uterus and fallopian tubes | |
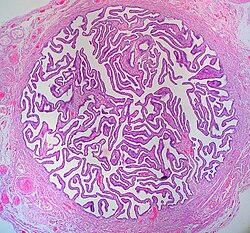 Cross-section of Fallopian tube, stained and viewed under microscope | |
| Details | |
| System | Reproductive system |
| Artery | tubal branches of ovarian artery, tubal branch of uterine artery via mesosalpinx |
| Lymph | lumbar lymph nodes |
| Identifiers | |
| Latin | Tuba uterina |
| Greek | Salpinx |
| MeSH | D005187 |
| TA98 | A09.1.02.001 |
| TA2 | 3486 |
| FMA | 18245 |
| Anatomical terminology | |
The Fallopian tubes, also known as uterine tubes, salpinges (singular salpinx), or oviducts, are tubes that stretch from the ovaries to the uterus, in the human female reproductive system. In other mammals they are called oviducts.
A fertilized egg passes through the Fallopian tubes from the ovaries to the uterus. The Fallopian tubes are lined with simple columnar epithelium with hair-like extensions called cilia which carry the fertilized egg.
The name comes from the Catholic priest and anatomist Gabriele Falloppio, for whom other anatomical structures are also named.
Structure[]
The Fallopian tube is composed of four parts. These are, described from near the ovaries to inwards near the uterus, the infundibulum with its associated fimbriae near the ovary, the ampulla that represents the major portion of the lateral tube, the isthmus, which is the narrower part of the tube that links to the uterus, and the interstitial (or intramural) part, the narrowest part of the uterine tube, that crosses the muscles of the uterine. The average length of a fallopian tube is 11-12 cm.[1] In other mammals the Fallopian tube is called the oviduct which may also be used in reference to the Fallopian tube in the human.[2][3]
Parts[]
The uterus opens into the Fallopian tube at the proximal tubal opening (also called the proximal ostium or os[4]), after the uterotubal junction, and accessible via hysteroscopy. Occlusion at this opening is referred to as proximal tubal occlusion. From there there are three named parts of the Fallopian tube; the isthmus, the ampulla, and the infundibulum. The isthmus sits next to the opening of the Fallopian tube into the uterus. It connects to the ampulla (Latin: flask), which curves over the ovary and is the most common site of human fertilization.
The ampulla connects with the infundibulum, which rests above the ovaries, and ends at the distal tubal opening (or abdominal ostium)[5] into the abdominal cavity where, in ovulation, the oocyte enters the Fallopian tube. The opening is surrounded by fimbriae, which help in the collection of the oocyte. Occlusion of this opening is referred to as distal tubal occlusion. The fimbriae (singular fimbria) is a fringe of tissue around the ostium of the Fallopian tube, in the direction of the ovary. Of all fimbriae, one fimbria is long enough to reach the ovary. It is called fimbria ovarica.[6][7]
An ovary is not directly connected to its adjacent Fallopian tube. When ovulation is about to occur, the sex hormones activate the fimbriae, causing them to swell with blood and hit the ovary in a gentle, sweeping motion. An oocyte is released from the ovary into the peritoneal cavity and the cilia of the fimbriae sweep the ovum into the Fallopian tube.
Microanatomy[]
When viewed under the microscope, the Fallopian tube has four to five layers (depending on the classification system used). From outer to inner these are the serosa, subserosa, muscularis, submucosa and innermost mucosa with lamina propria and epithelium. The serosa is derived from the visceral peritoneum. The subserosa is composed of loose adventitious tissue, blood vessels, lymphatics. The muscularis consist of outer longitudinal and inner circular smooth muscle coats. This layer is responsible for the rhythmic contraction, called peristalsis, of the Fallopian tubes.[8] The histological features of tube vary along its length. The mucosa of the ampulla contains an extensive array of complex folds, whereas the relatively narrow isthmus has a thick muscular coat and simple mucosal folds.[8]

The innermost layer of the tube is an epithelium composed of a single layer of column-shaped cells. The columnar cells have microscopic hair-like filaments called cilia throughout the tube, most numerous in the infundibulum and ampulla. Estrogen increases the formation of cilia on these cells. Between the ciliated cells are peg cells, which contain apical granules and produce tubular fluid. This fluid contains nutrients for spermatozoa, oocytes, and zygotes. The secretions also promote capacitation of the sperm by removing glycoproteins and other molecules from the plasma membrane of the sperm. Progesterone increases the number of peg cells, while estrogen increases their height and secretory activity. Fluid flows through the tubes towards the ovaries, the opposite direction to the action of the cilia.
Development[]

Embryos develop a urogenital ridge that forms at their tail end and eventually forms the basis for the urinary system and reproductive tracts. Either side and to the front of this tract, around the sixth week develops a duct called the paramesonephric duct, also called the Müllerian duct.[9] A second duct, the mesonephric duct, develops adjacent to this. Both ducts become longer over the next two weeks, and the paramesonephric ducts around the eighth week cross to meet in the midline and fuse.[9] One duct then regresses, with this depending on whether the embryo is genetically female or male. In females, the paramesonephric duct remains, and eventually forms the female reproductive tract.[9] The portions of the paramesonephric duct which are more cranial - that is, further from the tail-end, end up forming the fallopian tubes.[9] In males, because of the presence of the Y sex chromosome, anti-mullerian hormone is produced. This leads to the degeneration of the paramesonephric duct.[9]
As the uterus develops, the part of the fallopian tubes closer to the uterus, the ampulla, becomes larger. Extensions from the fallopian tubes, the fimbriae, develop over time.
Apart from the presence of sex chromosomes, specific genes associated with the development of the fallopian tubes include the Wnt and Hox groups of genes, , , and .[9]
Embryos have two pairs of ducts to let gametes out of the body; one pair (the Müllerian ducts) develops in females into the fallopian tubes, uterus, and vagina, while the other pair (the Wolffian ducts) develops in males into the epididymis and vas deferens.
The homologous organ in the male is the rudimentary appendix testis.[citation needed]
Function[]
Fertilization[]
The fallopian tube allows the passage of an egg from the ovary to the uterus. When an oocyte is developing in an ovary, it is surrounded by a spherical collection of cells known as an ovarian follicle. Just before ovulation, the primary oocyte completes meiosis I to form the first polar body and a secondary oocyte which is arrested in metaphase of meiosis II.
At the time of ovulation in the menstrual cycle, the secondary oocyte is released from the ovary. The follicle and the ovary's wall rupture, allowing the secondary oocyte to escape. The secondary oocyte is caught by the fimbriated end of the fallopian tube and travels to the ampulla. Here, the egg is able to become fertilized with sperm. The ampulla is typically where the sperm are met and fertilization occurs; meiosis II is promptly completed. After fertilization, the ovum is now called a zygote and travels towards the uterus with the aid of the hair-like cilia and the activity of the muscle of the fallopian tube. The early embryo requires critical development in the fallopian tube.[10] After about five days the new embryo enters the uterine cavity and on about the sixth day implants on the wall of the uterus.
The release of an oocyte does not alternate between the two ovaries and seems to be random. After removal of an ovary, the remaining one produces an egg every month.[11]
Clinical significance[]
Inflammation[]
Salpingitis is inflammation of the fallopian tubes and may be found alone, or as part of pelvic inflammatory disease (PID). A thickening of the fallopian tube at its narrow portion, due to inflammation, is known as salpingitis isthmica nodosa. Like PID and endometriosis, it may lead to fallopian tube obstruction. Fallopian tube obstruction may be a cause of infertility or ectopic pregnancy.[12]
Cancer[]
Fallopian tube cancer, which typically arises from the epithelial lining of the fallopian tube, has historically been considered to be a very rare malignancy. Recent evidence suggests it probably represents a significant portion of what has been classified as ovarian cancer in the past.[13] While tubal cancers may be misdiagnosed as ovarian cancer, it is of little consequence as the treatment of both ovarian and fallopian tube cancer is similar.[citation needed]
Implantation[]

Occasionally the embryo implants into the fallopian tube instead of the uterus, creating an ectopic pregnancy, commonly known as a "tubal pregnancy".
Blockage or narrowing[]
While full testing of tubal functions in patients with infertility is not possible, testing of whether the tubes are open, called patency, is important as tubal obstruction is a major cause of infertility. A hysterosalpingogram, laparoscopy and dye, or hysterocontrast sonography will demonstrate whether the tubes are open. Tubal insufflation is a standard procedure for testing patency. During surgery, the condition of the tubes may be inspected and a dye such as methylene blue can be injected into the uterus and shown to pass through the tubes when the cervix is occluded. As tubal disease is often related to Chlamydia infection, testing for Chlamydia antibodies has become a cost-effective screening device for tubal pathology.[14]
Surgery[]

The surgical removal of a fallopian tube is called a salpingectomy. To remove both tubes is a bilateral salpingectomy. An operation that combines the removal of a fallopian tube with the removal of at least one ovary is a salpingo-oophorectomy. An operation to remove a fallopian tube obstruction is called a tuboplasty.
Other[]
It is possible for the Fallopian tube to prolapse into the vaginal canal following a hysterectomy, if the vaginal cuff is open. Given the beefy-red appearance of the tubes, it is possible to mistake the tube for either a tumor or granulation tissue at the vaginal cuff. [15]
History[]
The Fallopian tubes are named after the 16th-century Italian anatomist Gabriele Falloppio, the first person to provide a detailed description of the tubes.[16][17] He thought they resembled trumpets, tube in Italian, which was misunderstood and became the English "tube".[18]
Though the name Fallopian tube is eponymous, it is often spelt with a lower case f from the assumption that the adjective fallopian has been absorbed into modern English as the de facto name for the structure.[citation needed]
Additional images[]

2: Medial surface
3: Lateral surface
4: Free border
5: Mesovarial margin
6: Tubal extremity
7: Uterine extremity
8: Fallopian tube
9: Distal opening of the Fallopian tube
10: Infundibulum of the Fallopian tube
11: Fimbriae of the Fallopian tube
12: Ovarian fimbria
13: Ampulla of the Fallopian tube
14: Isthmus of the Fallopian tube
15: Uterine part of the Fallopian tube
16: Proximal opening of the Fallopian tube

24. Fallopian tube: 25. Isthmus; 26. Ampulla; 27. Infundibulum; 28. Fimbria (with 29. Fimbria ovarica)
30. Ovary
31. Visceral pelvic peritoneum: 32. Broad ligament (with 33. Mesosalpinx;
Ligaments: 36. Round; 37. Ovarian; 38. Suspensory of ovary
Blood vessels: 39. Ovarian artery and vein; 40. Uterine artery and veins
Other: 48. Abdominal cavity

Image showing the right Fallopian tube (here labeled the uterine tube) seen from behind. The uterus, ovaries and right broad ligament are labeled.

Isthmus of the Fallopian tube seen arising from the uterus in a cadaveric specimen
See also[]
References[]
![]() This article incorporates text in the public domain from page 1257 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 1257 of the 20th edition of Gray's Anatomy (1918)
- ^ Eddy, Carlton A; Pauerstein, Carl J (December 1980). "Anatomy and physiology of the fallopian tube". Clinical Obstetrics and Gynecology. 23 (4): 1177–93. doi:10.1097/00003081-198012000-00023. PMID 7004702. S2CID 42445339.
- ^ Li, S; Winuthayanon, W (January 2017). "Oviduct: roles in fertilization and early embryo development". The Journal of Endocrinology. 232 (1): R1–R26. doi:10.1530/JOE-16-0302. PMID 27875265.
- ^ Harris, EA; Stephens, KK; Winuthayanon, W (5 November 2020). "Extracellular Vesicles and the Oviduct Function". International Journal of Molecular Sciences. 21 (21): 8280. doi:10.3390/ijms21218280. PMC 7663821. PMID 33167378.
- ^ Thurmond AS, Brandt KR, Gorrill MJ (March 1999). "Tubal Obstruction after Ligation Reversal Surgery: Results of Catheter Recanalization". Radiology. 210 (3): 747–750. doi:10.1148/radiology.210.3.r99mr10747. PMID 10207477. Archived from the original on 2013-04-15. Retrieved 2010-05-28.
- ^ EI-Mowafi DM, Diamond MM. "Fallopian Tube". Geneva Foundation for Medical Education and Research. Retrieved 2010-05-28.
- ^ Cancerweb- ovarian fimbria
- ^ Daftary, Shirish; Chakravarti, Sudip (2011). Manual of Obstetrics, 3rd Edition. Elsevier. pp. 1-16. ISBN 9788131225561.
- ^ a b Daftary, Shirish; Chakravarti, Sudip (2011). Manual of Obstetrics (3rd ed.). Elsevier. pp. 1–16. ISBN 978-81-312-2556-1.
- ^ a b c d e f Blausteins 2011, pp. 530–531.
- ^ Li, Shuai; Winuthayanon, Wipawee (January 2017). "Oviduct: roles in fertilization and early embryo development". Journal of Endocrinology. 232 (1): R1–R26. doi:10.1530/JOE-16-0302. PMID 27875265.
- ^ "Menstrual Cycle: Biology of the Female Reproductive System: Merck Manual Home Health Handbook". Merck.com. Retrieved 2011-03-06.
- ^ Salpingitis at eMedicine
- ^ Hirst, Jane E.; Gard, Gregory B.; McIllroy, Kirsty; Nevell, David; Field, Michael (July 2009). "High Rates of Occult Fallopian Tube Cancer Diagnosed at Prophylactic Bilateral Salpingo-Oophorectomy". International Journal of Gynecological Cancer. 19 (5): 826–829. doi:10.1111/IGC.0b013e3181a1b5dc. PMID 19574767. S2CID 6496116.
- ^ Kodaman PH, Arici A, Seli E (June 2004). "Evidence-based diagnosis and management of tubal factor infertility". Current Opinion in Obstetrics and Gynecology. 16 (3): 221–9. doi:10.1097/00001703-200406000-00004. PMID 15129051. S2CID 43312882.
- ^ "Benign Neoplasms of the Vagina | GLOWM". www.glowm.com. Retrieved 2018-03-11.
- ^ Falloppii, Gabrielis (1561). Observationes Anatomicae Ad Petrum Mannam Medicum Cremonensem. Venetiis, M. A. Ulmum.
- ^ Blausteins 2011, p. 530.
- ^ "A Medley of Maladies". QI. Series M. Episode 1. 16 October 2015. 0:38:37 minutes in. BBC Two. Transcript from Subsaga.com. Retrieved 2 July 2017.
He thought they reminded him of what were in those days rather long musical instruments with an end like a trumpet's bell, these were tubas. And so he called them tubas. And if you have a tuba, if you have a word ending in A in Italian, how do you pluralise it? What is two tuba? ... Tube. With an E on the end, spelled T-U-B-E. So, when it went around the world as his tube, his tubas, people saw the word tube. But, in fact, he had called them tubas.
Books[]
- Kurman, Robert J.; Ellenson, Lora Hedrick; Ronnett, Brigitte M., eds. (2011). "Diseases of the Fallopian Tube and Paratubal Region". Blaustein's pathology of the female genital tract (6th. ed.). Springer. ISBN 9781441904881.
External links[]
| Wikimedia Commons has media related to Fallopian tube. |
- Histology image: 18501loa – Histology Learning System at Boston University
- Menstrual Cycle - Merck
- Wikipedia articles incorporating text from the 20th edition of Gray's Anatomy (1918)
- Pelvis
- Human female reproductive system


