Restless legs syndrome
| Restless legs syndrome | |
|---|---|
| Other names | Willis–Ekbom disease (WED),[1] Wittmaack–Ekbom syndrome |
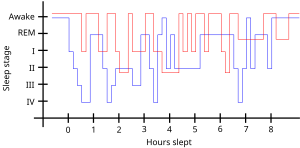 | |
| Sleep pattern of a person with restless legs syndrome (red) compared to a healthy sleep pattern (blue) | |
| Specialty | Sleep medicine |
| Symptoms | Unpleasant feeling in the legs that briefly improves with moving them[2] |
| Complications | Daytime sleepiness, low energy, irritability, sadness[2] |
| Usual onset | More common with older age[3] |
| Risk factors | Low iron levels, kidney failure, Parkinson's disease, diabetes mellitus, rheumatoid arthritis, pregnancy, certain medications[2][4][5] |
| Diagnostic method | Based on symptoms after ruling out other possible causes[6] |
| Treatment | Lifestyle changes, medication[2] |
| Medication | Levodopa, dopamine agonists, gabapentin[4] |
| Frequency | 2.5–15% (US)[4] |
Restless legs syndrome (RLS), now known as Willis-Ekbom Disease (WED), is generally a long-term disorder that causes a strong urge to move one's legs.[2][7] There is often an unpleasant feeling in the legs that improves somewhat by moving them.[2] This is often described as aching, tingling, or crawling in nature.[2] Occasionally, arms may also be affected.[2] The feelings generally happen when at rest and therefore can make it hard to sleep.[2] Due to the disturbance in sleep, people with RLS may have daytime sleepiness, low energy, irritability and a depressed mood.[2] Additionally, many have limb twitching during sleep.[8] RLS is not the same as habitual foot tapping or leg rocking.[9]
Risk factors for RLS include low iron levels, kidney failure, Parkinson's disease, diabetes mellitus, rheumatoid arthritis, pregnancy and celiac disease.[2][4][10] A number of medications may also trigger the disorder including antidepressants, antipsychotics, antihistamines, and calcium channel blockers.[5] There are two main types.[2] One is early onset RLS which starts before age 45, runs in families and worsens over time.[2] The other is late onset RLS which begins after age 45, starts suddenly, and does not worsen.[2] Diagnosis is generally based on a person's symptoms after ruling out other potential causes.[6]
Restless leg syndrome may resolve if the underlying problem is addressed.[11] Otherwise treatment includes lifestyle changes and medication.[2] Lifestyle changes that may help include stopping alcohol and tobacco use, and sleep hygiene.[11] Medications used include levodopa or a dopamine agonist such as pramipexole.[4] RLS affects an estimated 2.5–15% of the American population.[4] Females are more commonly affected than males, and it becomes increasingly common with age.[3][1]
Signs and symptoms[]
RLS sensations range from pain or an aching in the muscles, to "an itch you can't scratch", a "buzzing sensation", an unpleasant "tickle that won't stop", a "crawling" feeling, or limbs jerking while awake. The sensations typically begin or intensify during quiet wakefulness, such as when relaxing, reading, studying, or trying to sleep.[12]
It is a "spectrum" disease with some people experiencing only a minor annoyance and others having major disruption of sleep and impairments in quality of life.[13]
The sensations—and the need to move—may return immediately after ceasing movement or at a later time. RLS may start at any age, including childhood, and is a progressive disease for some, while the symptoms may remit in others.[14] In a survey among members of the Restless Legs Syndrome Foundation,[15] it was found that up to 45% of patients had their first symptoms before the age of 20 years.[16]
- "An urge to move, usually due to uncomfortable sensations that occur primarily in the legs, but occasionally in the arms or elsewhere."
- The sensations are unusual and unlike other common sensations. Those with RLS have a hard time describing them, using words or phrases such as uncomfortable, painful, 'antsy', electrical, creeping, itching, pins and needles, pulling, crawling, buzzing, and numbness. It is sometimes described similar to a limb 'falling asleep' or an exaggerated sense of positional awareness of the affected area. The sensation and the urge can occur in any body part; the most cited location is legs, followed by arms. Some people have little or no sensation, yet still, have a strong urge to move.
- "Motor restlessness, expressed as activity, which relieves the urge to move."
- Movement usually brings immediate relief, although temporary and partial. Walking is most common; however, stretching, yoga, biking, or other physical activity may relieve the symptoms. Continuous, fast up-and-down movements of the leg, and/or rapidly moving the legs toward then away from each other, may keep sensations at bay without having to walk. Specific movements may be unique to each person.
- "Worsening of symptoms by relaxation."
- Sitting or lying down (reading, plane ride, watching TV) can trigger the sensations and urge to move. Severity depends on the severity of the person's RLS, the degree of restfulness, duration of the inactivity, etc.
- "Variability over the course of the day-night cycle, with symptoms worse in the evening and early in the night."
- Some experience RLS only at bedtime, while others experience it throughout the day and night. Most people experience the worst symptoms in the evening and the least in the morning.
- "Restless legs feel similar to the urge to yawn, situated in the legs or arms."
- These symptoms of RLS can make sleeping difficult for many patients and a recent poll shows the presence of significant daytime difficulties resulting from this condition. These problems range from being late for work to missing work or events because of drowsiness. Patients with RLS who responded reported driving while drowsy more than patients without RLS. These daytime difficulties can translate into safety, social and economic issues for the patient and for society.
RLS may contribute to higher rates of depression and anxiety disorders in RLS patients.[17]
Primary and secondary[]
RLS is categorized as either primary or secondary.
- Primary RLS is considered idiopathic or with no known cause. Primary RLS usually begins slowly, before approximately 40–45 years of age and may disappear for months or even years. It is often progressive and gets worse with age. RLS in children is often misdiagnosed as growing pains.
- Secondary RLS often has a sudden onset after age 40, and may be daily from the beginning. It is most associated with specific medical conditions or the use of certain drugs (see below).
Causes[]
While the cause is generally unknown, it is believed to be caused by changes in the nerve transmitter dopamine[18] resulting in an abnormal use of iron by the brain.[1] RLS is often due to iron deficiency (low total body iron status).[1] Other associated conditions may include end-stage kidney disease and hemodialysis, folate deficiency, magnesium deficiency, sleep apnea, diabetes, peripheral neuropathy, Parkinson's disease, and certain autoimmune diseases, such as multiple sclerosis.[19] RLS can worsen in pregnancy, possibly due to elevated estrogen levels.[1][20] Use of alcohol, nicotine products, and caffeine may be associated with RLS.[1] A 2014 study from the American Academy of Neurology also found that reduced leg oxygen levels were strongly associated with Restless Leg Syndrome symptom severity in untreated patients.[21]
ADHD[]
An association has been observed between attention deficit hyperactivity disorder (ADHD) and RLS or periodic limb movement disorder.[22] Both conditions appear to have links to dysfunctions related to the neurotransmitter dopamine, and common medications for both conditions among other systems, affect dopamine levels in the brain.[23] A 2005 study suggested that up to 44% of people with ADHD had comorbid (i.e. coexisting) RLS, and up to 26% of people with RLS had confirmed ADHD or symptoms of the condition.[24]
Medications[]
Certain medications may cause or worsen RLS, or cause it secondarily, including:[1]
- certain antiemetics (antidopaminergic ones)[25]
- certain antihistamines (especially the sedating, first generation H1 antihistamines often in over-the-counter cold medications)[25]
- many antidepressants (both older TCAs and newer SSRIs)[1][25]
- antipsychotics and certain anticonvulsants[1]
- a rebound effect of sedative-hypnotic drugs such as a benzodiazepine withdrawal syndrome from discontinuing benzodiazepine tranquilizers or sleeping pills[1]
- alcohol withdrawal can also cause restless legs syndrome and other movement disorders such as akathisia and parkinsonism usually associated with antipsychotics[26]
- opioid withdrawal is associated with causing and worsening RLS[27]
Both primary and secondary RLS can be worsened by surgery of any kind; however, back surgery or injury can be associated with causing RLS.[28]
The cause vs. effect of certain conditions and behaviors observed in some patients (ex. excess weight, lack of exercise, depression or other mental illnesses) is not well established. Loss of sleep due to RLS could cause the conditions, or medication used to treat a condition could cause RLS.[29][30]
Genetics[]
More than 60% of cases of RLS are familial and are inherited in an autosomal dominant fashion with variable penetrance.[31]
Research and brain autopsies have implicated both dopaminergic system and iron insufficiency in the substantia nigra.[32] Iron is well understood to be an essential cofactor for the formation of L-dopa, the precursor of dopamine.
Six genetic loci found by linkage are known and listed below. Other than the first one, all of the linkage loci were discovered using an autosomal dominant model of inheritance.
- The first genetic locus was discovered in one large French Canadian family and maps to chromosome 12q.[33][34] This locus was discovered using an autosomal recessive inheritance model. Evidence for this locus was also found using a transmission disequilibrium test (TDT) in 12 Bavarian families.[35]
- The second RLS locus maps to chromosome 14q and was discovered in one Italian family.[36] Evidence for this locus was found in one French Canadian family.[37] Also, an association study in a large sample 159 trios of European descent showed some evidence for this locus.[38]
- This locus maps to chromosome 9p and was discovered in two unrelated American families.[39] Evidence for this locus was also found by the TDT in a large Bavarian family,[40] in which significant linkage to this locus was found.[41]
- This locus maps to chromosome 20p and was discovered in a large French Canadian family with RLS.[42]
- This locus maps to chromosome 2p and was found in three related families from population isolated in South Tyrol.[43]
- The sixth locus is located on chromosome 16p12.1 and was discovered by Levchenko et al. in 2008.[44]
Three genes, MEIS1, BTBD9 and MAP2K5, were found to be associated to RLS.[45] Their role in RLS pathogenesis is still unclear. More recently, a fourth gene, PTPRD was found to be associated with RLS.[46]
There is also some evidence that periodic limb movements in sleep (PLMS) are associated with BTBD9 on chromosome 6p21.2,[47][48] MEIS1, MAP2K5/SKOR1, and PTPRD.[48] The presence of a positive family history suggests that there may be a genetic involvement in the etiology of RLS.
Mechanism[]
Although it is only partly understood, pathophysiology of restless legs syndrome may involve dopamine and iron system anomalies.[49][50] There is also a commonly acknowledged circadian rhythm explanatory mechanism associated with it, clinically shown simply by biomarkers of circadian rhythm, such as body temperature.[51] The interactions between impaired neuronal iron uptake and the functions of the neuromelanin-containing and dopamine-producing cells have roles in RLS development, indicating that iron deficiency might affect the brain dopaminergic transmissions in different ways.[52]
Medial thalamic nuclei may also have a role in RLS as part as the limbic system modulated by the dopaminergic system[53] which may affect pain perception.[54] Improvement of RLS symptoms occurs in people receiving low-dose dopamine agonists.[55]
Diagnosis[]
There are no specific tests for RLS, but non-specific laboratory tests are used to rule out other causes such as vitamin deficiencies. Five symptoms are used to confirm the diagnosis:[1]
- A strong urge to move the limbs, usually associated with unpleasant or uncomfortable sensations.
- It starts or worsens during inactivity or rest.
- It improves or disappears (at least temporarily) with activity.
- It worsens in the evening or night.
- These symptoms are not caused by any medical or behavioral condition.
These symptoms are not essential, like the ones above, but occur commonly in RLS patients:[1][56]
- genetic component or family history with RLS
- good response to dopaminergic therapy
- periodic leg movements during day or sleep
- most strongly affected are people who are middle-aged or older
- other sleep disturbances are experienced
- decreased iron stores can be a risk factor and should be assessed
According to the International Classification of Sleep Disorders (ICSD-3), the main symptoms have to be associated with a sleep disturbance or impairment in order to support RLS diagnosis.[57] As stated by this classification, RLS symptoms should begin or worsen when being inactive, be relieved when moving, should happen exclusively or mostly in the evening and at night, not be triggered by other medical or behavioral conditions, and should impair one's quality of life.[57][58] Generally, both legs are affected, but in some cases there is an asymmetry.
Differential diagnosis[]
The most common conditions that should be differentiated with RLS include leg cramps, positional discomfort, local leg injury, arthritis, leg edema, venous stasis, peripheral neuropathy, radiculopathy, habitual foot tapping/leg rocking, anxiety, myalgia, and drug-induced akathisia.[9]
Peripheral artery disease and arthritis can also cause leg pain but this usually gets worse with movement.[8]
There are less common differential diagnostic conditions included myelopathy, myopathy, vascular or neurogenic claudication, , orthostatic tremor, painful legs, and .[9]
Treatment[]
If RLS is not linked to an underlying cause, its frequency may be reduced by lifestyle modifications such as adopting improving sleep hygiene, regular exercise, and stopping smoking.[59] Medications used may include dopamine agonists or gabapentin in those with daily restless legs syndrome, and opioids for treatment of resistant cases.[1][27]
Treatment of RLS should not be considered until possible medical causes are ruled out. Secondary RLS may be cured if precipitating medical conditions (anemia) are managed effectively.[1]
Physical measures[]
Stretching the leg muscles can bring temporary relief.[12][60] Walking and moving the legs, as the name "restless legs" implies, brings temporary relief. In fact, those with RLS often have an almost uncontrollable need to walk and therefore relieve the symptoms while they are moving. Unfortunately, the symptoms usually return immediately after the moving and walking ceases. A vibratory counter-stimulation device has been found to help some people with primary RLS to improve their sleep.[61]
Iron[]
There is some evidence that intravenous iron supplementation moderately improves restlessness for people with RLS.[62]
Medications[]
For those whose RLS disrupts or prevents sleep or regular daily activities, medication may be useful. Evidence supports the use of dopamine agonists including: pramipexole, ropinirole, rotigotine, and cabergoline.[63][64] They reduce symptoms, improve sleep quality and quality of life.[65] Levodopa is also effective.[66] However, pergolide and cabergoline are less recommended due to their association with increased risk of valvular heart disease.[67] Ropinirole has a faster onset with shorter duration.[68] Rotigotine is commonly used as a transdermal patch which continuously provides stable plasma drug concentrations, resulting in its particular therapeutic effect on patients with symptoms throughout the day.[68] One review found pramipexole to be better than ropinirole.[69][needs update]
There are, however, issues with the use of dopamine agonists including augmentation. This is a medical condition where the drug itself causes symptoms to increase in severity and/or occur earlier in the day. Dopamine agonists may also cause rebound when symptoms increase as the drug wears off. In many cases, the longer dopamine agonists have been used the higher the risk of augmentation and rebound as well as the severity of the symptoms. Also, a recent study indicated that dopamine agonists used in restless leg syndrome can lead to an increase in compulsive gambling.[70]
- Gabapentin or pregabalin, a non-dopaminergic treatment for moderate to severe primary RLS[71]
- Opioids are only indicated in severe cases that do not respond to other measures due to their high rate of side effects, which may include constipation, fatigue and headache.[72][27]
One possible treatment for RLS is dopamine agonists, unfortunately patients can develop dopamine dysregulation syndrome, meaning that they can experience an addictive pattern of dopamine replacement therapy. Additionally, they can exhibit some behavioral disturbances such as impulse control disorders like pathologic gambling, compulsive purchasing and compulsive eating.[73] There are some indications that stopping the dopamine agonist treatment has an impact on the resolution or at least improvement of the impulse control disorder, even though some people can be particularly exposed to dopamine agonist withdrawal syndrome.[74]
Benzodiazepines, such as diazepam or clonazepam, are not generally recommended,[75] and their effectiveness is unknown.[76] They however are sometimes still used as a second line,[77] as add on agents.[76] Quinine is not recommended due to its risk of serious side effects involving the blood.[78]
Prognosis[]
RLS symptoms may gradually worsen with age, although more slowly for those with the idiopathic form of RLS than for people who also have an associated medical condition.[79] Current therapies can control the disorder, minimizing symptoms and increasing periods of restful sleep. In addition, some people have remissions, periods in which symptoms decrease or disappear for days, weeks, or months, although symptoms usually eventually reappear.[79] Being diagnosed with RLS does not indicate or foreshadow another neurological disease, such as Parkinson's disease.[79] RLS symptoms can worsen over time when dopamine-related drugs are used for therapy, an effect called "augmentation" which may represent symptoms occurring throughout the day and affect movements of all limbs.[79] There is no cure for RLS.[79]
Epidemiology[]
RLS affects an estimated 2.5–15% of the American population.[4][80] A minority (around 2.7% of the population) experience daily or severe symptoms.[81] RLS is twice as common in women as in men,[82] and Caucasians are more prone to RLS than people of African descent.[80] RLS occurs in 3% of individuals from the Mediterranean or Middle Eastern regions, and in 1–5% of those from East Asia, indicating that different genetic or environmental factors, including diet, may play a role in the prevalence of this syndrome.[80][83] RLS diagnosed at an older age runs a more severe course.[60] RLS is even more common in individuals with iron deficiency, pregnancy, or end-stage kidney disease.[84][85] The National Sleep Foundation's 1998 Sleep in America poll showed that up to 25 percent of pregnant women developed RLS during the third trimester.[86] Poor general health is also linked.[87]
There are several risk factors for RLS, including old age, family history, and uremia. The prevalence of RLS tends to increase with age, as well as its severity and longer duration of symptoms. People with uremia receiving renal dialysis have a prevalence from 20% to 57%, while those having kidney transplant improve compared to those treated with dialysis.[88]
RLS can occur at all ages, although it typically begins in the third or fourth decade.[58] Genome‐wide association studies have now identified 19 risk loci associated with RLS.[89] Neurological conditions linked to RLS include Parkinson's disease, spinal cerebellar atrophy, spinal stenosis,[specify] lumbosacral radiculopathy and Charcot–Marie–Tooth disease type 2.[80]
History[]
The first known medical description of RLS was by Sir Thomas Willis in 1672.[90] Willis emphasized the sleep disruption and limb movements experienced by people with RLS. Initially published in Latin (De Anima Brutorum, 1672) but later translated to English (The London Practice of Physick, 1685), Willis wrote:
Wherefore to some, when being abed they betake themselves to sleep, presently in the arms and legs, leapings and contractions on the tendons, and so great a restlessness and tossings of other members ensue, that the diseased are no more able to sleep, than if they were in a place of the greatest torture.
The term "fidgets in the legs" has also been used as early as the early nineteenth century.[91]
Subsequently, other descriptions of RLS were published, including those by François Boissier de Sauvages (1763), Magnus Huss (1849), Theodur Wittmaack (1861), George Miller Beard (1880), Georges Gilles de la Tourette (1898), Hermann Oppenheim (1923) and Frederick Gerard Allison (1943).[90][92] However, it was not until almost three centuries after Willis, in 1945, that Karl-Axel Ekbom (1907–1977) provided a detailed and comprehensive report of this condition in his doctoral thesis, Restless legs: clinical study of hitherto overlooked disease.[93] Ekbom coined the term "restless legs" and continued work on this disorder throughout his career. He described the essential diagnostic symptoms, differential diagnosis from other conditions, prevalence, relation to anemia, and common occurrence during pregnancy.[94][95]
Ekbom's work was largely ignored until it was rediscovered by Arthur S. Walters and Wayne A. Hening in the 1980s. Subsequent landmark publications include 1995 and 2003 papers, which revised and updated the diagnostic criteria.[12][96] Journal of Parkinsonism and RLS is the first peer-reviewed, online, open access journal dedicated to publishing research about Parkinson's disease and was founded by a Canadian neurologist Dr. Abdul Qayyum Rana.
Nomenclature[]
For decades the most widely used name for the disease was restless legs syndrome, and it is still the most commonly used. In 2013 the Restless Legs Syndrome Foundation renamed itself the Willis–Ekbom Disease Foundation,[97] and it encourages the use of the name Willis–Ekbom disease; its reasons are quoted as follows:[97]
The name Willis–Ekbom disease:
- Eliminates incorrect descriptors—the condition often involves parts of the body other than legs
- Promotes cross-cultural ease of use
- Responds to trivialization of the disease and humorous treatment in the media
- Acknowledges the first known description by Sir Thomas Willis in 1672 and the first detailed clinical description by Dr. Karl Axel Ekbom in 1945.[97]
A point of confusion is that RLS and delusional parasitosis are entirely different conditions that have both been called "Ekbom syndrome", as both syndromes were described by the same person, Karl-Axel Ekbom.[98] Today, calling WED/RLS "Ekbom syndrome" is outdated usage, as the unambiguous names (WED or RLS) are preferred for clarity.
Controversy[]
Some doctors express the view that the incidence of restless leg syndrome is exaggerated by manufacturers of drugs used to treat it.[99] Others believe it is an underrecognized and undertreated disorder.[80] Further, GlaxoSmithKline ran advertisements that, while not promoting off-licence use of their drug (ropinirole) for treatment of RLS, did link to the Ekbom Support Group website. That website contained statements advocating the use of ropinirole to treat RLS. The ABPI ruled against GSK in this case.[100]
Research[]
Different measurements have been used to evaluate treatments in RLS. Most of them are based on subjective rating scores, such as IRLS rating scale (IRLS), Clinical Global Impression (CGI), Patient Global Impression (PGI), and Quality of life (QoL).[101] These questionnaires provide information about the severity and progress of the disease, as well as the person's quality of life and sleep.[101] Polysomnography (PSG) and actigraphy (both related to sleep parameters) are more objective resources that provide evidences of sleep disturbances associated with RLS symptoms.[101]
See also[]
References[]
- ^ Jump up to: a b c d e f g h i j k l m n "Restless Legs Syndrome Fact Sheet | National Institute of Neurological Disorders and Stroke". Ninds.nih.gov. Retrieved 7 July 2019.
- ^ Jump up to: a b c d e f g h i j k l m n o "What Is Restless Legs Syndrome?". NHLBI. November 1, 2010. Archived from the original on 21 August 2016. Retrieved 19 August 2016.
- ^ Jump up to: a b "Who Is at Risk for Restless Legs Syndrome?". NHLBI. November 1, 2010. Archived from the original on 26 August 2016. Retrieved 19 August 2016.
- ^ Jump up to: a b c d e f g Ramar, K; Olson, EJ (Aug 15, 2013). "Management of common sleep disorders". American Family Physician. 88 (4): 231–8. PMID 23944726.
- ^ Jump up to: a b "What Causes Restless Legs Syndrome?". NHLBI. November 1, 2010. Archived from the original on 20 August 2016. Retrieved 19 August 2016.
- ^ Jump up to: a b "How Is Restless Legs Syndrome Diagnosed?". NHLBI. November 1, 2010. Archived from the original on 27 August 2016. Retrieved 19 August 2016.
- ^ "Restless Legs Syndrome Information Page | National Institute of Neurological Disorders and Stroke". Ninds.nih.gov. Retrieved 7 July 2019.
- ^ Jump up to: a b "What Are the Signs and Symptoms of Restless Legs Syndrome?". NHLBI. November 1, 2010. Archived from the original on 27 August 2016. Retrieved 19 August 2016.
- ^ Jump up to: a b c Allen, Richard P.; Picchietti, Daniel L.; Garcia-Borreguero, Diego; Ondo, William G.; Walters, Arthur S.; Winkelman, John W.; Zucconi, Marco; Ferri, Raffaele; Trenkwalder, Claudia (2014-08-01). "Restless legs syndrome/Willis–Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria – history, rationale, description, and significance". Sleep Medicine. 15 (8): 860–873. doi:10.1016/j.sleep.2014.03.025. ISSN 1389-9457. PMID 25023924.
- ^ Zis P, Hadjivassiliou M (2019). "Treatment of Neurological Manifestations of Gluten Sensitivity and Coeliac Disease". Curr Treat Options Neurol (Review). 21 (3): 10. doi:10.1007/s11940-019-0552-7. PMID 30806821.
- ^ Jump up to: a b "How Is Restless Legs Syndrome Treated?". NHLBI. November 1, 2010. Archived from the original on 27 August 2016. Retrieved 19 August 2016.
- ^ Jump up to: a b c Allen, R; Picchietti, D; Hening, WA; Trenkwalder, C; Walters, AS; Montplaisi, J; Restless Legs Syndrome Diagnosis Epidemiology workshop at the National Institutes of Health; International Restless Legs Syndrome Study Group (2003). "Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health". Sleep Medicine. 4 (2): 101–19. doi:10.1016/S1389-9457(03)00010-8. PMID 14592341.
- ^ Earley, Christopher J.; Silber, Michael H. (2010). "Restless legs syndrome: Understanding its consequences and the need for better treatment". Sleep Medicine. 11 (9): 807–15. doi:10.1016/j.sleep.2010.07.007. PMID 20817595.
- ^ Xiong, L.; Montplaisir, J.; Desautels, A.; Barhdadi, A.; Turecki, G.; Levchenko, A.; Thibodeau, P.; Dubé, M. P.; Gaspar, C.; Rouleau, GA (2010). "Family Study of Restless Legs Syndrome in Quebec, Canada: Clinical Characterization of 671 Familial Cases". Archives of Neurology. 67 (5): 617–22. doi:10.1001/archneurol.2010.67. PMID 20457962.
- ^ "Willis–Ekbom Disease Foundation Reverts to Original Name" (PDF). 2013. Archived from the original (PDF) on 2015-09-24.
- ^ Walters, A. S.; Hickey, K.; Maltzman, J.; Verrico, T.; Joseph, D.; Hening, W.; Wilson, V.; Chokroverty, S. (1996). "A questionnaire study of 138 patients with restless legs syndrome: The 'Night-Walkers' survey". Neurology. 46 (1): 92–5. doi:10.1212/WNL.46.1.92. PMID 8559428. S2CID 25278952.
- ^ Becker, PM; Sharon, D (July 2014). "Mood disorders in restless legs syndrome (Willis–Ekbom disease)". The Journal of Clinical Psychiatry. 75 (7): e679–94. doi:10.4088/jcp.13r08692. PMID 25093484.
- ^ St. Louis E.K. (2014). New evidence for reduced leg oxygen levels in restless legs syndrome. Neurology, 82, e185. https://doi.org/10.1212/WNL.0000000000000513
- ^ "Restless legs syndrome". MedlinePlus, US National Library of Medicine, National Institutes of Health. 7 August 2017. Retrieved 23 June 2019.
- ^ Gupta, R.; Dhyani, M.; Kendzerska, T.; Pandi-Perumal, S. R.; BaHammam, A. S.; Srivanitchapoom, P.; Pandey, S.; Hallett, M. (19 October 2015). "Restless legs syndrome and pregnancy: prevalence, possible pathophysiological mechanisms and treatment". Acta Neurologica Scandinavica. 133 (5): 320–329. doi:10.1111/ane.12520. ISSN 0001-6314. PMC 5562408. PMID 26482928.
- ^ St. Louis E.K. (2014). New evidence for reduced leg oxygen levels in restless legs syndrome. Neurology, 82, e185. https://doi.org/10.1212/WNL.0000000000000513
- ^ Walters, A. S.; Silvestri, R; Zucconi, M; Chandrashekariah, R; Konofal, E (2008). "Review of the Possible Relationship and Hypothetical Links Between Attention Deficit Hyperactivity Disorder (ADHD) and the Simple Sleep Related Movement Disorders, Parasomnias, Hypersomnias, and Circadian Rhythm Disorders". Journal of Clinical Sleep Medicine. 4 (6): 591–600. doi:10.5664/jcsm.27356. PMC 2603539. PMID 19110891.
- ^ "Attention deficit hyperactivity disorder – Other Disorders Associated with ADHD". University of Maryland Medical Center. Check
|archive-url=value (help) - ^ Cortese, S; Konofal, E; Lecendreux, M; Arnulf, I; Mouren, MC; Darra, F; Dalla Bernardina, B (2005). "Restless legs syndrome and attention-deficit/hyperactivity disorder: A review of the literature". Sleep. 28 (8): 1007–13. doi:10.1093/sleep/28.8.1007. PMID 16218085.
- ^ Jump up to: a b c Buchfuhrer, MJ (October 2012). "Strategies for the treatment of restless legs syndrome". Neurotherapeutics (Review). 9 (4): 776–90. doi:10.1007/s13311-012-0139-4. PMC 3480566. PMID 22923001.
- ^ Neiman, J; Lang, AE; Fornazzari, L; Carlen, PL (May 1990). "Movement disorders in alcoholism: a review". Neurology. 40 (5): 741–6. doi:10.1212/wnl.40.5.741. PMID 2098000. S2CID 8940680.
- ^ Jump up to: a b c Trenkwalder, Claudia; Zieglgänsberger, Walter; Ahmedzai, Sam H.; Högl, Birgit (2017). "Pain, opioids, and sleep: implications for restless legs syndrome treatment". Sleep Medicine. 31: 78–85. doi:10.1016/j.sleep.2016.09.017. ISSN 1389-9457. PMID 27964861.
- ^ Crotti, Francesco Maria; Carai, A.; Carai, M.; Sgaramella, E.; Sias, W. (2005). "Entrapment of crural branches of the common peroneal nerve". Advanced Peripheral Nerve Surgery and Minimal Invasive Spinal Surgery. Acta Neurochirurgica. 97. pp. 69–70. doi:10.1007/3-211-27458-8_15. ISBN 978-3-211-23368-9. PMID 15830971.
- ^ "Exercise and Restless Legs Syndrome". Archived from the original on 2015-08-06. Retrieved 2008-05-28.
- ^ Phillips, Barbara A.; Britz, Pat; Hening, Wayne (October 31, 2005). The NSF 2005 Sleep in American poll and those at risk for RLS. Chest 2005. Lay summary – ScienceDaily (October 31, 2005).
- ^ Lavigne, GJ; Montplaisir, JY (1994). "Restless legs syndrome and sleep bruxism: prevalence and association among Canadians". Sleep. 17 (8): 739–43. PMID 7701186.
- ^ Connor, J.R.; Boyer, P.J.; Menzies, S.L.; Dellinger, B.; Allen, R.P.; Ondo, W.G.; Earley, C.J. (2003). "Neuropathological examination suggests impaired brain iron acquisition in restless legs syndrome". Neurology. 61 (3): 304–9. doi:10.1212/01.WNL.0000078887.16593.12. PMID 12913188. S2CID 44703083.
- ^ Desautels, Alex; Turecki, Gustavo; Montplaisir, Jacques; Sequeira, Adolfo; Verner, Andrei; Rouleau, Guy A. (2001). "Identification of a Major Susceptibility Locus for Restless Legs Syndrome on Chromosome 12q". The American Journal of Human Genetics. 69 (6): 1266–70. doi:10.1086/324649. PMC 1235538. PMID 11704926.
- ^ Desautels, A.; Turecki, G; Montplaisir, J; Xiong, L; Walters, AS; Ehrenberg, BL; Brisebois, K; Desautels, AK; Gingras, Y; Johnson, WG; Lugaresi, E; Coccagna, G; Picchietti, DL; Lazzarini, A; Rouleau, GA (2005). "Restless Legs Syndrome: Confirmation of Linkage to Chromosome 12q, Genetic Heterogeneity, and Evidence of Complexity". Archives of Neurology. 62 (4): 591–6. doi:10.1001/archneur.62.4.591. PMID 15824258.
- ^ Winkelmann, Juliane; Lichtner, Peter; Pütz, Benno; Trenkwalder, Claudia; Hauk, Stephanie; Meitinger, Thomas; Strom, Tim; Muller-Myhsok, Bertram (2006). "Evidence for further genetic locus heterogeneity and confirmation of RLS-1 in restless legs syndrome". Movement Disorders. 21 (1): 28–33. doi:10.1002/mds.20627. PMID 16124010. S2CID 25736900.
- ^ Bonati, M. T. (2003). "Autosomal dominant restless legs syndrome maps on chromosome 14q". Brain. 126 (6): 1485–92. doi:10.1093/brain/awg137. PMID 12764067.
- ^ Levchenko, Anastasia; Montplaisir, Jacques-Yves; Dubé, Marie-Pierre; Riviere, Jean-Baptiste; St-Onge, Judith; Turecki, Gustavo; Xiong, Lan; Thibodeau, Pascale; Desautels, Alex; Verlaan, Dominique J.; Rouleau, Guy A. (2004). "The 14q restless legs syndrome locus in the French Canadian population". Annals of Neurology. 55 (6): 887–91. doi:10.1002/ana.20140. PMID 15174026. S2CID 31001901.
- ^ Kemlink, David; Polo, Olli; Montagna, Pasquale; Provini, Federica; Stiasny-Kolster, Karin; Oertel, Wolfgang; De Weerd, Al; Nevsimalova, Sona; Sonka, Karel; Högl, Birgit; Frauscher, Birgit; Poewe, Werner; Trenkwalder, Claudia; Pramstaller, Peter P.; Ferini-Strambi, Luigi; Zucconi, Marco; Konofal, Eric; Arnulf, Isabelle; Hadjigeorgiou, Georgios M.; Happe, Svenja; Klein, Christine; Hiller, Anja; Lichtner, Peter; Meitinger, Thomas; Müller-Myshok, Betram; Winkelmann, Juliane (2007). "Family-based association study of the restless legs syndrome loci 2 and 3 in a European population". Movement Disorders. 22 (2): 207–12. doi:10.1002/mds.21254. PMID 17133505. S2CID 34801702.
- ^ Chen, Shenghan; Ondo, William G.; Rao, Shaoqi; Li, Lin; Chen, Qiuyun; Wang, Qing (2004). "Genomewide Linkage Scan Identifies a Novel Susceptibility Locus for Restless Legs Syndrome on Chromosome 9p". The American Journal of Human Genetics. 74 (5): 876–885. doi:10.1086/420772. PMC 1181982. PMID 15077200.
- ^ Liebetanz, K. M.; Winkelmann, J; Trenkwalder, C; Pütz, B; Dichgans, M; Gasser, T; Müller-Myhsok, B (2006). "RLS3: Fine-mapping of an autosomal dominant locus in a family with intrafamilial heterogeneity". Neurology. 67 (2): 320–321. doi:10.1212/01.wnl.0000224886.65213.b5. PMID 16864828. S2CID 20796797.
- ^ Lohmann-Hedrich, K.; Neumann, A.; Kleensang, A.; Lohnau, T.; Muhle, H.; Djarmati, A.; König, I. R.; Pramstaller, P. P.; Schwinger, E.; Kramer, P. L.; Ziegler, A.; Stephani, U.; Klein, C. (2008). "Evidence for linkage of restless legs syndrome to chromosome 9p: Are there two distinct loci?". Neurology. 70 (9): 686–694. doi:10.1212/01.wnl.0000282760.07650.ba. PMID 18032746. S2CID 24889954.
- ^ Levchenko, A.; Provost, S; Montplaisir, JY; Xiong, L; St-Onge, J; Thibodeau, P; Rivière, JB; Desautels, A; Turecki, G; Dubé, M. P.; Rouleau, G. A. (2006). "A novel autosomal dominant restless legs syndrome locus maps to chromosome 20p13". Neurology. 67 (5): 900–901. doi:10.1212/01.wnl.0000233991.20410.b6. PMID 16966564. S2CID 20555259.
- ^ Pichler, Irene; Marroni, Fabio; Beu Volpato, Claudia; Gusella, James F.; Klein, Christine; Casari, Giorgio; De Grandi, Alessandro; Pramstaller, Peter P. (2006). "Linkage Analysis Identifies a Novel Locus for Restless Legs Syndrome on Chromosome 2q in a South Tyrolean Population Isolate". The American Journal of Human Genetics. 79 (4): 716–23. doi:10.1086/507875. PMC 1592574. PMID 16960808.
- ^ Levchenko, Anastasia; Montplaisir, Jacques-Yves; Asselin, GéRaldine; Provost, Sylvie; Girard, Simon L.; Xiong, Lan; Lemyre, Emmanuelle; St-Onge, Judith; Thibodeau, Pascale; Desautels, Alex; Turecki, Gustavo; Gaspar, Claudia; Dubé, Marie-Pierre; Rouleau, Guy A. (2009). "Autosomal-dominant locus for restless legs syndrome in French-Canadians on chromosome 16p12.1". Movement Disorders. 24 (1): 40–50. doi:10.1002/mds.22263. PMID 18946881. S2CID 7796597.
- ^ Winkelmann, Juliane; Schormair, Barbara; Lichtner, Peter; Ripke, Stephan; Xiong, Lan; Jalilzadeh, Shapour; Fulda, Stephany; Pütz, Benno; Eckstein, Gertrud; Hauk, Stephanie; Trenkwalder, Claudia; Zimprich, Alexander; Stiasny-Kolster, Karin; Oertel, Wolfgang; Bachmann, Cornelius G; Paulus, Walter; Peglau, Ines; Eisensehr, Ilonka; Montplaisir, Jacques; Turecki, Gustavo; Rouleau, Guy; Gieger, Christian; Illig, Thomas; Wichmann, H-Erich; Holsboer, Florian; Müller-Myhsok, Bertram; Meitinger, Thomas (2007). "Genome-wide association study of restless legs syndrome identifies common variants in three genomic regions". Nature Genetics. 39 (8): 1000–6. doi:10.1038/ng2099. PMID 17637780. S2CID 10606410.
- ^ Ding, Li; Getz, Gad; Wheeler, David A.; Mardis, Elaine R.; McLellan, Michael D.; Cibulskis, Kristian; Sougnez, Carrie; Greulich, Heidi; Muzny, Donna M.; Morgan, Margaret B.; Fulton, Lucinda; Fulton, Robert S.; Zhang, Qunyuan; Wendl, Michael C.; Lawrence, Michael S.; Larson, David E.; Chen, Ken; Dooling, David J.; Sabo, Aniko; Hawes, Alicia C.; Shen, Hua; Jhangiani, Shalini N.; Lewis, Lora R.; Hall, Otis; Zhu, Yiming; Mathew, Tittu; Ren, Yanru; Yao, Jiqiang; Scherer, Steven E.; Clerc, Kerstin (2008). "Somatic mutations affect key pathways in lung adenocarcinoma". Nature. 455 (7216): 1069–75. Bibcode:2008Natur.455.1069D. doi:10.1038/nature07423. PMC 2694412. PMID 18948947.
- ^ Stefansson, Hreinn; Rye, David B.; Hicks, Andrew; Petursson, Hjorvar; Ingason, Andres; Thorgeirsson, Thorgeir E.; Palsson, Stefan; Sigmundsson, Thordur; Sigurdsson, Albert P.; Eiriksdottir, Ingibjorg; Soebech, Emilia; Bliwise, Donald; Beck, Joseph M.; Rosen, Ami; Waddy, Salina; Trotti, Lynn M.; Iranzo, Alex; Thambisetty, Madhav; Hardarson, Gudmundur A.; Kristjansson, Kristleifur; Gudmundsson, Larus J.; Thorsteinsdottir, Unnur; Kong, Augustine; Gulcher, Jeffrey R.; Gudbjartsson, Daniel; Stefansson, Kari (2007). "A Genetic Risk Factor for Periodic Limb Movements in Sleep". New England Journal of Medicine. 357 (7): 639–47. doi:10.1056/NEJMoa072743. PMID 17634447. S2CID 44726156.
- ^ Jump up to: a b Moore, H; Winkelmann, J; Lin, L; Finn, L; Peppard, P; Mignot, E (2014). "Periodic leg movements during sleep are associated with polymorphisms in BTBD9, TOX3/BC034767, MEIS1, MAP2K5/SKOR1, and PTPRD". Sleep. 37 (9): 1535–1542. doi:10.5665/sleep.4006. PMC 4153066. PMID 25142570.
- ^ Allen, R (2004). "Dopamine and iron in the pathophysiology of restless legs syndrome (RLS)". Sleep Medicine. 5 (4): 385–91. doi:10.1016/j.sleep.2004.01.012. PMID 15222997.
- ^ Clemens, S.; Rye, D; Hochman, S (2006). "Restless legs syndrome: Revisiting the dopamine hypothesis from the spinal cord perspective". Neurology. 67 (1): 125–130. doi:10.1212/01.wnl.0000223316.53428.c9. PMID 16832090. S2CID 40963114.
- ^ Barrière, G.; Cazalets, J. R.; Bioulac, B.; Tison, F.; Ghorayeb, I. (2005-10-01). "The restless legs syndrome". Progress in Neurobiology. 77 (3): 139–165. doi:10.1016/j.pneurobio.2005.10.007. ISSN 0301-0082. PMID 16300874. S2CID 9327680.
- ^ Dauvilliers, Yves; Winkelmann, Juliane (2013-11-01). "Restless legs syndrome: update on pathogenesis". Current Opinion in Pulmonary Medicine. 19 (6): 594–600. doi:10.1097/MCP.0b013e328365ab07. ISSN 1070-5287. PMID 24048084. S2CID 20370566.
- ^ Klein, Marianne O.; Battagello, Daniella S.; Cardoso, Ariel R.; Hauser, David N.; Bittencourt, Jackson C.; Correa, Ricardo G. (2019-01-01). "Dopamine: Functions, Signaling, and Association with Neurological Diseases". Cellular and Molecular Neurobiology. 39 (1): 31–59. doi:10.1007/s10571-018-0632-3. ISSN 1573-6830. PMID 30446950. S2CID 53567202.
- ^ Garcia-Borreguero, Diego; Williams, Anne-Marie (2014-08-01). "An update on restless legs syndrome (Willis-Ekbom disease): clinical features, pathogenesis and treatment". Current Opinion in Neurology. 27 (4): 493–501. doi:10.1097/WCO.0000000000000117. ISSN 1350-7540. PMID 24978636.
- ^ Paulus, Walter; Trenkwalder, Claudia (2006-10-01). "Less is more: pathophysiology of dopaminergic-therapy-related augmentation in restless legs syndrome". The Lancet Neurology. 5 (10): 878–886. doi:10.1016/S1474-4422(06)70576-2. ISSN 1474-4422. PMID 16987735. S2CID 43111931.
- ^ Allen, Richard P.; Montplaisir, Jacques; Walters, Arthur Scott; Ferini-Strambi, Luigi; Högl, Birgit (2017), "Restless Legs Syndrome and Periodic Limb Movements During Sleep", Principles and Practice of Sleep Medicine, Elsevier, pp. 923–934.e6, doi:10.1016/b978-0-323-24288-2.00095-7, ISBN 9780323242882
- ^ Jump up to: a b Sateia, Michael J (November 2014). "International Classification of Sleep Disorders-Third Edition". Chest. 146 (5): 1387–1394. doi:10.1378/chest.14-0970. PMID 25367475.
- ^ Jump up to: a b Breen, DP; Högl, B; Fasano, A; Trenkwalder, C; Lang, AE (July 2018). "Sleep-related motor and behavioral disorders: Recent advances and new entities". Movement Disorders. 33 (7): 1042–1055. doi:10.1002/mds.27375. PMID 29756278. S2CID 21672153.
- ^ "Restless legs syndrome—Treatment". National Health Service. 6 August 2018.
- ^ Jump up to: a b Allen, Richard P.; Earley, Christopher J. (2001). "Restless Legs Syndrome". Journal of Clinical Neurophysiology. 18 (2): 128–47. doi:10.1097/00004691-200103000-00004. PMID 11435804. S2CID 34082653.
- ^ Foy, Jonette. "Regulation Name: Vibratory counter-stimulation device" (PDF). Food and Drug Administration. Archived (PDF) from the original on 24 October 2014. Retrieved 17 October 2014.
- ^ Trotti, Lynn M; Becker, Lorne A (2019). "Iron for the treatment of restless legs syndrome". Cochrane Database of Systematic Reviews (Systematic review). 1: CD007834. doi:10.1002/14651858.CD007834.pub3. ISSN 1465-1858. PMC 6353229. PMID 30609006.
- ^ Zintzaras, E; Kitsios, GD; Papathanasiou, AA; Konitsiotis, S; Miligkos, M; Rodopoulou, P; Hadjigeorgiou, GM (Feb 2010). "Randomized trials of dopamine agonists in restless legs syndrome: a systematic review, quality assessment, and meta-analysis". Clinical Therapeutics. 32 (2): 221–37. doi:10.1016/j.clinthera.2010.01.028. PMID 20206780.
- ^ Winkelman, JW; Armstrong, MJ; Allen, RP; Chaudhuri, KR; Ondo, W; Trenkwalder, C; Zee, PC; Gronseth, GS; Gloss, D; Zesiewicz, T (13 December 2016). "Practice guideline summary: Treatment of restless legs syndrome in adults: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology". Neurology. 87 (24): 2585–2593. doi:10.1212/wnl.0000000000003388. PMC 5206998. PMID 27856776.
- ^ Scholz, H.; Trenkwalder, C.; Kohnen, R.; Riemann, D.; Kriston, L.; Hornyak, M. (2011). Hornyak, Magdolna (ed.). "Dopamine agonists for restless legs syndrome". Cochrane Database Syst Rev (3): CD006009. doi:10.1002/14651858.CD006009.pub2. PMID 21412893.
- ^ Scholz, H; Trenkwalder, C; Kohnen, R; Riemann, D; Kriston, L; Hornyak, M (Feb 16, 2011). "Levodopa for restless legs syndrome". The Cochrane Database of Systematic Reviews (2): CD005504. doi:10.1002/14651858.CD005504.pub2. PMID 21328278.
- ^ Zanettini, Renzo; Antonini, Angelo; Gatto, Gemma; Gentile, Rosa; Tesei, Silvana; Pezzoli, Gianni (2007-01-04). "Valvular Heart Disease and the Use of Dopamine Agonists for Parkinson's Disease". New England Journal of Medicine. 356 (1): 39–46. doi:10.1056/NEJMoa054830. ISSN 0028-4793. PMID 17202454.
- ^ Jump up to: a b Mackie, Susan; Winkelman, John W. (2015-05-01). "Long-Term Treatment of Restless Legs Syndrome (RLS): An Approach to Management of Worsening Symptoms, Loss of Efficacy, and Augmentation". CNS Drugs. 29 (5): 351–357. doi:10.1007/s40263-015-0250-2. ISSN 1179-1934. PMID 26045290.
- ^ Quilici, S; Abrams, KR; Nicolas, A; Martin, M; Petit, C; Lleu, PL; Finnern, HW (Oct 2008). "Meta-analysis of the efficacy and tolerability of pramipexole versus ropinirole in the treatment of restless legs syndrome". Sleep Medicine. 9 (7): 715–26. doi:10.1016/j.sleep.2007.11.020. PMID 18226947.
- ^ Tippmann-Peikert, M.; Park, J. G.; Boeve, B. F.; Shepard, J. W.; Silber, M. H. (2007). "Pathologic gambling in patients with restless legs syndrome treated with dopaminergic agonists". Neurology. 68 (4): 301–3. doi:10.1212/01.wnl.0000252368.25106.b6. PMID 17242339. S2CID 26183000. Lay summary – ScienceDaily (February 9, 2007).
- ^ Nagandla, K; De, S (July 2013). "Restless legs syndrome: pathophysiology and modern management". Postgraduate Medical Journal. 89 (1053): 402–10. doi:10.1136/postgradmedj-2012-131634. PMID 23524988.
- ^ de Oliveira CO; Carvalho LB; Carlos K; Conti C; de Oliveira MM; Prado LB; Prado GF (29 June 2016). "Opioids for restless legs syndrome". Cochrane Database of Systematic Reviews. 6 (6): CD006941. doi:10.1002/14651858.CD006941.pub2. PMC 6885031. PMID 27355187.
- ^ Rosenberg, Richard S.; Tracy, Sharon L.; Lamm, Carin I.; Casey, Kenneth R.; Zak, Rochelle S.; Rowley, James A.; Bista, Sabin R.; Kristo, David A.; Aurora, R. Nisha (2012-08-01). "The Treatment of Restless Legs Syndrome and Periodic Limb Movement Disorder in Adults—An Update for 2012: Practice Parameters with an Evidence-Based Systematic Review and Meta-AnalysesAn American Academy of Sleep Medicine Clinical Practice Guideline". Sleep. 35 (8): 1039–1062. doi:10.5665/sleep.1988. ISSN 0161-8105. PMC 3397811. PMID 22851801.
- ^ Rosenberg, Richard S.; Tracy, Sharon L.; Lamm, Carin I.; Casey, Kenneth R.; Zak, Rochelle S.; Rowley, James A.; Bista, Sabin R.; Kristo, David A.; Aurora, R. Nisha (2012-08-01). "The Treatment of Restless Legs Syndrome and Periodic Limb Movement Disorder in Adults—An Update for 2012: Practice Parameters with an Evidence-Based Systematic Review and Meta-AnalysesAn American Academy of Sleep Medicine Clinical Practice Guideline". Sleep. 35 (8): 1039–1062. doi:10.5665/sleep.1988. ISSN 0161-8105. PMC 3397811. PMID 22851801.
- ^ Trenkwalder, C; Winkelmann, J; Inoue, Y; Paulus, W (August 2015). "Restless legs syndrome-current therapies and management of augmentation". Nature Reviews. Neurology. 11 (8): 434–45. doi:10.1038/nrneurol.2015.122. PMID 26215616. S2CID 22534190.
- ^ Jump up to: a b Carlos K, Prado GF, Teixeira CD, Conti C, de Oliveira MM, Prado LB, Carvalho LB (2017). "Benzodiazepines for restless legs syndrome". Cochrane Database Syst Rev. 3: CD006939. doi:10.1002/14651858.CD006939.pub2. PMC 6464545. PMID 28319266.
- ^ Garcia-Borreguero, D; Stillman, P; Benes, H; Buschmann, H; Chaudhuri, KR; Gonzalez Rodríguez, VM; Högl, B; Kohnen, R; Monti, GC; Stiasny-Kolster, K; Trenkwalder, C; Williams, AM; Zucconi, M (27 February 2011). "Algorithms for the diagnosis and treatment of restless legs syndrome in primary care". BMC Neurology. 11: 28. doi:10.1186/1471-2377-11-28. PMC 3056753. PMID 21352569.
- ^ "Qualaquin (quinine sulfate): New Risk Evaluation and Mitigation Strategy – Risk of serious hematological reactions". Archived from the original on 2010-07-16.
- ^ Jump up to: a b c d e "Restless Legs Syndrome Factsheet". National Institutes of Health. Archived from the original on January 4, 2015. Retrieved January 13, 2015.
- ^ Jump up to: a b c d e Gamaldo, C. E.; Earley, C. J. (2006). "Restless Legs Syndrome: A Clinical Update". Chest. 130 (5): 1596–604. doi:10.1378/chest.130.5.1596. PMID 17099042.
- ^ Allen, R. P.; Walters, AS; Montplaisir, J; Hening, W; Myers, A; Bell, TJ; Ferini-Strambi, L (2005). "Restless Legs Syndrome Prevalence and Impact: REST General Population Study". Archives of Internal Medicine. 165 (11): 1286–92. doi:10.1001/archinte.165.11.1286. PMID 15956009.
- ^ Berger, K.; Luedemann, J; Trenkwalder, C; John, U; Kessler, C (2004). "Sex and the Risk of Restless Legs Syndrome in the General Population". Archives of Internal Medicine. 164 (2): 196–202. doi:10.1001/archinte.164.2.196. PMID 14744844.
- ^ "Welcome – National Sleep Foundation". Archived from the original on 2007-07-28. Retrieved 2007-07-23.
- ^ Lee, Kathryn A.; Zaffke, Mary Ellen; Baratte-Beebe, Kathleen (2001). "Restless Legs Syndrome and Sleep Disturbance during Pregnancy: The Role of Folate and Iron". Journal of Women's Health & Gender-Based Medicine. 10 (4): 335–41. doi:10.1089/152460901750269652. PMID 11445024.
- ^ Trenkwalder, C; Allen, R; Högl, B; Paulus, W; Winkelmann, J (5 April 2016). "Restless legs syndrome associated with major diseases: A systematic review and new concept". Neurology. 86 (14): 1336–1343. doi:10.1212/WNL.0000000000002542. PMC 4826337. PMID 26944272.
- ^ "Sleeping By Trimesters: 3rd Trimester". National Sleep Foundation. Archived from the original on 2007-05-08.
- ^ Yeh, Paul; Walters, Arthur S.; Tsuang, John W. (1 December 2012). "Restless legs syndrome: a comprehensive overview on its epidemiology, risk factors, and treatment". Sleep & Breathing = Schlaf & Atmung. 16 (4): 987–1007. doi:10.1007/s11325-011-0606-x. ISSN 1522-1709. PMID 22038683. S2CID 24079411.
- ^ Hening, Wayne; Allen, Richard; Earley, Christopher; Kushida, Clete; Picchietti, Daniel; Silber, Michael (1999). "The Treatment of Restless Legs Syndrome and Periodic Limb Movement Disorder". Sleep. doi:10.1093/sleep/22.7.970.
- ^ Schormair, Barbara (November 2017). "Identification of novel risk loci for restless legs syndrome in genome-wide association studies in individuals of European ancestry: a meta-analysis". The Lancet Neurology. 16 (11): 898–907. doi:10.1016/S1474-4422(17)30327-7. PMC 5755468. PMID 29029846.
- ^ Jump up to: a b Coccagna, G; Vetrugno, R; Lombardi, C; Provini, F (2004). "Restless legs syndrome: an historical note". Sleep Medicine. 5 (3): 279–83. doi:10.1016/j.sleep.2004.01.002. PMID 15165536.
- ^ Caleb Hillier PARRY (1815). Elements of Pathology and Therapeutics. Vol. 1 ... General Pathology. pp. 381 & 397. Archived from the original on 2017-09-08.
- ^ Konofal, Eric; Karroum, Elias; Montplaisir, Jacques; Derenne, Jean-Philippe; Arnulf, Isabelle (2009). "Two early descriptions of restless legs syndrome and periodic leg movements by Boissier de Sauvages (1763) and Gilles de la Tourette (1898)". Sleep Medicine. 10 (5): 586–91. doi:10.1016/j.sleep.2008.04.008. PMID 18752999.
- ^ Ekrbom, Karl-Axel (2009). "PREFACE". Acta Medica Scandinavica. 121: 1–123. doi:10.1111/j.0954-6820.1945.tb11970.x.
- ^ Teive, Hélio A.G.; Munhoz, Renato P.; Barbosa, Egberto Reis (2009). "Professor Karl-Axel Ekbom and restless legs syndrome". Parkinsonism & Related Disorders. 15 (4): 254–7. doi:10.1016/j.parkreldis.2008.07.011. PMID 18829374.
- ^ Ulfberg, J (2004). "The legacy of Karl-Axel Ekbom". Sleep Medicine. 5 (3): 223–4. doi:10.1016/j.sleep.2004.04.002. PMID 15165526.
- ^ Walters, Arthur S.; Aldrich, Michael S.; Allen, Richard; Ancoli-Israel, Sonia; Buchholz, David; Chokroverty, Sudhansu; Coccagna, Giorgio; Earley, Christopher; Ehrenberg, Bruce; Feest, T. G.; Hening, Wayne; Kavey, Neil; Lavigne, Gilles; Lipinski, Joseph; Lugaresi, Elio; Montagna, Pasquale; Montplaisir, Jacques; Mosko, Sarah S.; Oertel, Wolfgang; Picchietti, Daniel; Pollmächer, Thomas; Shafor, Renata; Smith, Robert C.; Telstad, Wenche; Trenkwalder, Claudia; Von Scheele, Christian; Walters, Arthur S.; Ware, J. Catesby; Zucconi, Marco (1995). "Toward a better definition of the restless legs syndrome". Movement Disorders. 10 (5): 634–42. doi:10.1002/mds.870100517. PMID 8552117. S2CID 22970514.
- ^ Jump up to: a b c "Restless Legs Syndrome Foundation is now the Willis–Ekbom Disease Foundation". 2013. Archived from the original on 2013-09-15.
- ^ Wittmaack–Ekbom syndrome at Who Named It?
- ^ Woloshin, Steven; Schwartz, Lisa M. (2006). "Giving Legs to Restless Legs: A Case Study of How the Media Helps Make People Sick". PLOS Medicine. 3 (4): e170. doi:10.1371/journal.pmed.0030170. PMC 1434499. PMID 16597175.
- ^ Templeton, Sarah-Kate (August 6, 2006). "Glaxo's cure for 'restless legs' was an unlicensed drug". Times Online. Times Newspapers Ltd. Archived from the original on February 11, 2007. Retrieved 2009-07-24.
- ^ Jump up to: a b c Aurora, R. Nisha; Kristo, David A.; Bista, Sabin R.; Rowley, James A.; Zak, Rochelle S.; Casey, Kenneth R.; Lamm, Carin I.; Tracy, Sharon L.; Rosenberg, Richard S. (August 2012). "Update to the AASM Clinical Practice Guideline: "The Treatment of Restless Legs Syndrome and Periodic Limb Movement Disorder in Adults—An Update for 2012: Practice Parameters with an Evidence-Based Systematic Review and Meta-Analyses"". Sleep. 35 (8): 1037. doi:10.5665/sleep.1986. PMC 3397810. PMID 22851800.
External links[]
| Wikimedia Commons has media related to Restless leg syndrome. |
| Look up restless legs syndrome in Wiktionary, the free dictionary. |
| Classification | |
|---|---|
| External resources |
- Extrapyramidal and movement disorders
- Psychiatric diagnosis
- Sleep disorders
- Syndromes
