Symptoms of COVID-19
| Part of a series on the |
| COVID-19 pandemic |
|---|
 |
|
|
|
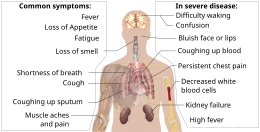
Symptoms of COVID-19 are variable, ranging from mild symptoms to severe illness.[1][2] Common symptoms include headache, loss of smell and taste, nasal congestion and runny nose, cough, muscle pain, sore throat, fever, diarrhea, and breathing difficulties.[3] People with the same infection may have different symptoms, and their symptoms may change over time. Three common clusters of symptoms have been identified: one respiratory symptom cluster with cough, sputum, shortness of breath, and fever; a musculoskeletal symptom cluster with muscle and joint pain, headache, and fatigue; a cluster of digestive symptoms with abdominal pain, vomiting, and diarrhea.[3] In people without prior ear, nose, and throat disorders, loss of taste combined with loss of smell is associated with COVID-19.[4]
Of people who show symptoms, 81% develop only mild to moderate symptoms (up to mild pneumonia), while 14% develop severe symptoms (dyspnea, hypoxia, or more than 50% lung involvement on imaging) and 5% of patients suffer critical symptoms (respiratory failure, shock, or multiorgan dysfunction).[5] At least a third of the people who are infected with the virus do not develop noticeable symptoms at any point in time.[6][7] These asymptomatic carriers tend not to get tested and can spread the disease.[7][8][9][10] Other infected people will develop symptoms later, called "pre-symptomatic", or have very mild symptoms and can also spread the virus.[10]
As is common with infections, there is a delay between the moment a person first becomes infected and the appearance of the first symptoms. The median delay for COVID-19 is four to five days.[11] Most symptomatic people experience symptoms within two to seven days after exposure, and almost all will experience at least one symptom within 12 days.[11][12]
Most people recover from the acute phase of the disease. However, some people – over half of a cohort of home-isolated young patients[13][14] – continue to experience a range of effects, such as fatigue, for months after recovery, a condition called long COVID; long-term damage to organs has been observed. Multi-year studies are underway to further investigate the long-term effects of the disease.[15]
Overview[]
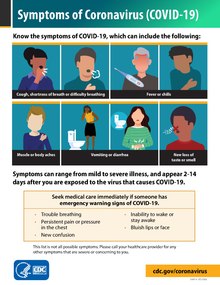
Some symptoms of COVID-19 can be relatively non-specific; the most common symptoms are fever, dry cough, and fatigue.[1][16] Among those who develop symptoms, approximately one in five may become more seriously ill and have difficulty in breathing. Emergency symptoms include difficulty in breathing, persistent chest pain or pressure, sudden confusion, difficulty walking, and bluish face or lips; immediate medical attention is advised if these symptoms are present.[1] Further development of the disease can lead to complications including pneumonia, acute respiratory distress syndrome, sepsis, septic shock, and kidney failure.
Some symptoms usually appear sooner than others. In August 2020, scientists at the University of Southern California reported the "likely" order of initial symptoms of the COVID-19 disease as a fever followed by a cough and muscle pain, and that nausea and vomiting usually appear before diarrhea.[17] This contrasts with the most common path for influenza where it is common to develop a cough first and fever later.[17] While health agency guidelines tend to recommend isolating for 14 days while watching for symptoms to develop,[18] there is limited evidence that symptoms may develop for some patients more than 14 days after initial exposure.[19]
Systemic[]
Typical systemic symptoms include fatigue, and muscle and joint pains. Some people have a sore throat.[1][2][16]
Fever[]
Fever is one of the most common symptoms in COVID-19 patients. However, its absence at an initial screening does not rule out COVID-19. Fever in the first week of a COVID-19 infection is part of the body's natural immune response; however, if the infections develop into a cytokine storm the fever is counterproductive. As of September 2020, little research had focused on relating fever intensity to outcomes.[20]
A June 2020 systematic review reported a 75–81% prevalence of fever.[2] As of July 2020, the European Centre for Disease Prevention and Control (ECDC) reported a prevalence rate of ~45% for fever.[3]
Pain[]
A June 2020 systematic review reported a 27–35% prevalence of fatigue, 14–19% for muscle pain, 10–14% for sore throat.[2] As of July 2020, the ECDC reported a prevalence rate of ~63% for muscle weakness (asthenia), ~63% for muscle pain (myalgia), and ~53% for sore throat.[3]
Respiratory[]
Cough is another typical symptom of COVID-19, which could be either dry or a productive cough.[2]
Some symptoms, such as difficulty breathing, are more common in patients who need hospital care.[1] Shortness of breath tends to develop later in the illness.
Respiratory complications may include pneumonia and acute respiratory distress syndrome (ARDS).[21][22][23][24]
As of July 2020, the ECDC reported a prevalence rate of ~68% for nasal obstruction, ~63% for cough, ~60% for rhinorrhoea.[3] A June 2020 systematic review reported a 54–61% prevalence of dry cough and 22–28% for productive cough.[2]
Cardiovascular[]
This section needs expansion. You can help by . (March 2021) |
Cardiovascular complications may include heart failure, arrhythmias, heart inflammation, and blood clots.[25][26][27][28][29] They are common traits in severe COVID-19 patients.[30]
Hypertension seems to be the most prevalent risk factor for myocardial injury in COVID-19 disease. It was reported in 58% of individuals with cardiac injury in a recent meta-analysis.[31]
Several cases of acute myocarditis associated with COVID-19 have been described around the globe and are diagnosed in multiple ways. Taking into consideration serology, leukocytosis with neutrophilia and lymphopenia was found in many patients. Cardiac biomarkers troponin and N-terminal (NT)-prohormone BNP (NT-proBNP) were seen elevated. Similarly, the level of inflammation-related markers such as C-reactive protein (CRP), D-dimer, IL-6, procalcitonin was significantly increased, indicating an inflammatory process in the body. Electrocardiogram findings were variable and ranged from sinus tachycardia, ST-segment elevation, T-wave inversion and ST-depression.[32] In one case, viral particles were seen in the interstitial cell, and another case reported SARS-CoV-2 RT–PCR positivity in the cardiac tissue suggestive of direct viral injury to the myocardium.[33][34] Endomyocardial biopsy [EMB] remains the gold standard invasive technique in diagnosing myocarditis; however, due to the increased risk of infection, it is not done in COVID-19 patients.
The binding of the SARS-CoV-2 virus through ACE2 receptors present in heart tissue may be responsible for direct viral injury leading to myocarditis.[32]In a study done during the SARS outbreak, SARS virus RNA was ascertained in the autopsy of heart specimens in 35% of the patients who died due to SARS.[35] It was also observed that an already diseased heart has increased expression of ACE2 receptor contrasted to healthy individuals.[36] Hyperactive immune responses in COVID-19 Patients may lead to the initiation of the cytokine storm. This excess release of cytokines may lead to myocardial injury.[32]
Neurological[]
Patients with COVID-19 can present with neurological symptoms that can be broadly divided into central nervous system involvement, such as headache, dizziness, altered mental state, and disorientation, and peripheral nervous system involvement, such as anosmia and dysgeusia.[37] Some patients experience cognitive dysfunction called "COVID fog", or "COVID brain fog", involving memory loss, inattention, poor concentration or disorientation.[38][39] Other neurologic manifestations include seizures, strokes, encephalitis, and Guillain–Barré syndrome (which includes loss of motor functions).[40][41]
As of July 2020, the ECDC reported a prevalence rate of ~70% for headache.[3] A June 2020 systematic review reported a 10–16% prevalence of headache.[2]
Loss of smell[]
In some people, COVID-19 causes people to temporarily lose their sense of smell either partially or fully.[42][43]
This symptom, if it is present at all, often appears early in the illness.[42] Its onset is often reported to be sudden. Smell usually returns to normal within a month. However, for some patients it improves very slowly and is associated with odors being perceived as unpleasant or different than they originally did (parosmia), and for some people smell does not return for at least many months.[43] It is an unusual symptom for other respiratory diseases, so it is used for symptom-based screening.[42][43]
Loss of smell has several consequences. Loss of smell increases foodborne illness due to inability to detect spoiled food, and may increase fire hazards due to inability to detect smoke. It has also been linked to depression. If smell does not return, smell training is a potential option.[43]
It is sometimes the only symptom to be reported, implying that it has a neurological basis separate from nasal congestion. As of January 2021, it is believed that these symptoms are caused by infection of sustentacular cells that support and provide nutrients to sensory neurons in the nose, rather than infection of the neurons themselves. Sustentacular cells have many Angiotensin-converting enzyme 2 (ACE2) receptors on their surfaces, while olfactory sensory neurons do not. Loss of smell may also be the result of inflammation in the olfactory bulb.[43]
A June 2020 systematic review found a 29–54% prevalence of olfactory dysfunction for people with COVID-19,[42] while an August 2020 study using a smell-identification test reported that 96% of people with COVID-19 had some olfactory dysfunction, and 18% had total smell loss.[43] Another June 2020 systematic review reported a 4–55% prevalence of hyposmia.[2] As of July 2020, the ECDC reported a prevalence rate of ~70% for loss of smell.[3]
A disturbance in smell or taste is more commonly found in younger people, and perhaps because of this, it is correlated with a lower risk of medical complications.[42]
Loss of taste and chemesthesis[]
In some people, COVID-19 causes people to temporarily experience changes in how food tastes (dysgeusia or ageusia).[42][43] Changes to chemesthesis, which includes chemically triggered sensations such as spiciness, are also reported. As of January 2021, the mechanism for taste and chemesthesis symptoms were not well understood.[43]
A June 2020 systematic review found a 24–54% prevalence of gustatory dysfunction for people with COVID-19.[42] Another June 2020 systematic review reported a 1–8% prevalence of hypogeusia.[2] As of July 2020, the ECDC reported a prevalence rate of ~54% for gustatory dysfunction.[3]
Other neurological and psychiatric symptoms[]
Other neurological symptoms appear to be rare, but may affect half of patients who are hospitalized with severe COVID-19. Some reported symptoms include delirium, stroke, brain hemorrhage, memory loss, psychosis, peripheral nerve damage, anxiety, and post-traumatic stress disorder. Neurological symptoms in many cases are correlated with damage to the brain's blood supply or encephalitis, which can progress in some cases to acute disseminated encephalomyelitis. Strokes have been reported in younger people without conventional risk factors.[44]
As of September 2020, it was unclear whether these symptoms were due to direct infection of brain cells, or of overstimulation of the immune system.[44]
A June 2020 systematic review reported a 6–16% prevalence of vertigo or dizziness, 7–15% for confusion, and 0–2% for ataxia.[2]
Other[]
Other symptoms are less common among people with COVID-19. Some people experience gastrointestinal symptoms such as loss of appetite, diarrhea, nausea or vomiting.[1][45] A June 2020 systematic review reported a 8–12% prevalence of diarrhea, and 3–10% for nausea.[2]
Less common symptoms include chills, coughing out blood, diarrhea, and rash.[16] The so-called "COVID toes" are pink to violaceous papules arising on the hands and feet. These chilblain-like lesions often occur only in younger patients and do not appear until late in the disease or during convalescence.[46] Certain genetic polymorphisms (in the TREX1 gene) have been linked to susceptibility towards developing COVID-toe.[47] A June 2020 systematic review reported a 0–1% prevalence of rash in COVID-19 patients.[2]
Approximately 20–30% of people who present with COVID-19 have elevated liver enzymes, reflecting liver injury.[48][49]
Complications include multi-organ failure, septic shock, and death.[21][22][23][24]
Longer-term effects[]
Multisystem inflammatory syndrome in children[]
Following the infection, children may develop multisystem inflammatory syndrome, also called paediatric multisystem inflammatory syndrome. This has symptoms similar to Kawasaki disease, which can be fatal.[50][51][52]
Long COVID[]
Some early studies suggest that ten to twenty percent of people with COVID-19 will experience symptoms lasting longer than a month.[53][54] A majority of those who were admitted to hospital with severe disease report long-term problems, including fatigue and shortness of breath.[55] About 5–10% of patients admitted to hospital progress to severe or critical disease, including pneumonia and acute respiratory failure.[56]
By a variety of mechanisms, the lungs are the organs most affected in COVID-19.[57] In people requiring hospital admission, up to 98% of CT scans performed show lung abnormalities after 28 days of illness even if they had clinically improved.[58]
People with advanced age, severe disease, prolonged ICU stays, or who smoke are more likely to have long-lasting effects, including pulmonary fibrosis.[59] Overall, approximately one-third of those investigated after four weeks will have findings of pulmonary fibrosis or reduced lung function as measured by DLCO, even in asymptomatic people, but with the suggestion of continuing improvement with the passing of more time.[57]References[]
- ^ Jump up to: a b c d e f "Symptoms of Coronavirus". U.S. Centers for Disease Control and Prevention (CDC). 22 February 2021. Archived from the original on 4 March 2021. Retrieved 4 March 2021.
- ^ Jump up to: a b c d e f g h i j k l Grant MC, Geoghegan L, Arbyn M, Mohammed Z, McGuinness L, Clarke EL, Wade RG (23 June 2020). "The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS-CoV-2; COVID-19): A systematic review and meta-analysis of 148 studies from 9 countries". PLOS ONE. 15 (6): e0234765. Bibcode:2020PLoSO..1534765G. doi:10.1371/journal.pone.0234765. PMC 7310678. PMID 32574165. S2CID 220046286.
- ^ Jump up to: a b c d e f g h "Clinical characteristics of COVID-19". European Centre for Disease Prevention and Control. Retrieved 29 December 2020.
- ^ Niazkar HR, Zibaee B, Nasimi A, Bahri N (July 2020). "The neurological manifestations of COVID-19: a review article". Neurological Sciences. 41 (7): 1667–1671. doi:10.1007/s10072-020-04486-3. PMC 7262683. PMID 32483687.
- ^ "Interim Clinical Guidance for Management of Patients with Confirmed Coronavirus Disease (COVID-19)". U.S. Centers for Disease Control and Prevention (CDC). 6 April 2020. Archived from the original on 2 March 2020. Retrieved 19 April 2020.
- ^ Multiple sources:
- Oran DP, Topol EJ (January 2021). "The Proportion of SARS-CoV-2 Infections That Are Asymptomatic : A Systematic Review". Annals of Internal Medicine. 174 (5): 655–662. doi:10.7326/M20-6976. PMC 7839426. PMID 33481642.
- "Transmission of COVID-19". European Centre for Disease Prevention and Control. Retrieved 6 December 2020.
- Nogrady B (November 2020). "What the data say about asymptomatic COVID infections". Nature. 587 (7835): 534–535. Bibcode:2020Natur.587..534N. doi:10.1038/d41586-020-03141-3. PMID 33214725.
- ^ Jump up to: a b Gao Z, Xu Y, Sun C, Wang X, Guo Y, Qiu S, Ma K (February 2021). "A systematic review of asymptomatic infections with COVID-19". Journal of Microbiology, Immunology, and Infection = Wei Mian Yu Gan Ran Za Zhi. 54 (1): 12–16. doi:10.1016/j.jmii.2020.05.001. PMC 7227597. PMID 32425996.
- ^ Oran, Daniel P., and Eric J. Topol. “Prevalence of Asymptomatic SARS-CoV-2 Infection : A Narrative Review.” Annals of Internal Medicine. vol. 173,5 (2020): 362-367. doi:10.7326/M20-3012 PMID 32491919 Retrieved 14 January 2021.
- ^ Lai CC, Liu YH, Wang CY, Wang YH, Hsueh SC, Yen MY, et al. (June 2020). "Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): Facts and myths". Journal of Microbiology, Immunology, and Infection = Wei Mian Yu Gan Ran Za Zhi. 53 (3): 404–412. doi:10.1016/j.jmii.2020.02.012. PMC 7128959. PMID 32173241.
- ^ Jump up to: a b Furukawa NW, Brooks JT, Sobel J (July 2020). "Evidence Supporting Transmission of Severe Acute Respiratory Syndrome Coronavirus 2 While Presymptomatic or Asymptomatic". Emerging Infectious Diseases. 26 (7). doi:10.3201/eid2607.201595. PMC 7323549. PMID 32364890.
- ^ Jump up to: a b Gandhi RT, Lynch JB, Del Rio C (October 2020). "Mild or Moderate Covid-19". The New England Journal of Medicine. 383 (18): 1757–1766. doi:10.1056/NEJMcp2009249. PMID 32329974.
- ^ Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC (August 2020). "Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review". JAMA. 324 (8): 782–793. doi:10.1001/jama.2020.12839. PMID 32648899. S2CID 220465311.
- ^ "Half of young adults with COVID-19 have persistent symptoms after 6 months". medicalxpress.com. Retrieved 10 July 2021.
- ^ Blomberg B, Mohn KG, Brokstad KA, Zhou F, Linchausen DW, Hansen BA, et al. (June 2021). "Long COVID in a prospective cohort of home-isolated patients". Nature Medicine: 1–7. doi:10.1038/s41591-021-01433-3. PMID 34163090. S2CID 235625772.
- ^ CDC (11 February 2020). "COVID-19 and Your Health". Centers for Disease Control and Prevention. Retrieved 23 January 2021.
- ^ Jump up to: a b c "Coronavirus". World Health Organization (WHO). Retrieved 4 May 2020.
- ^ Jump up to: a b Larsen JR, Martin MR, Martin JD, Kuhn P, Hicks JB (13 August 2020). "Modeling the Onset of Symptoms of COVID-19". Frontiers in Public Health. 8: 473. doi:10.3389/fpubh.2020.00473. PMC 7438535. PMID 32903584. S2CID 221105179.[non-primary source needed]
- ^ "Considerations for quarantine of contacts of COVID-19 cases". World Health Organization.
WHO recommends that all contacts of individuals with a confirmed or probable COVID-19 be quarantined in a designated facility or at home for 14 days from their last exposure.
- ^ Bikbov B, Bikbov A (2021). "Maximum incubation period for COVID-19 infection: Do we need to rethink the 14-day quarantine policy?". Travel Medicine and Infectious Disease. 40: 101976. doi:10.1016/j.tmaid.2021.101976. PMC 7816956. PMID 33476809.
Notably, these incubation periods longer than 14 days were registered not only in sporadic cases, but in a substantial proportion reaching... 5.0% out of 339, 7.7% out of 104... patients with traced contacts
- ^ Gul MH, Htun ZM, Inayat A (February 2021). "Role of fever and ambient temperature in COVID-19". Expert Review of Respiratory Medicine. 15 (2): 171–173. doi:10.1080/17476348.2020.1816172. PMC 7544962. PMID 32901576.
- ^ Jump up to: a b Hui DS, I Azhar E, Madani TA, Ntoumi F, Kock R, Dar O, et al. (February 2020). "The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health - The latest 2019 novel coronavirus outbreak in Wuhan, China". International Journal of Infectious Diseases. 91: 264–266. doi:10.1016/j.ijid.2020.01.009. PMC 7128332. PMID 31953166.
- ^ Jump up to: a b Murthy S, Gomersall CD, Fowler RA (April 2020). "Care for Critically Ill Patients With COVID-19". JAMA. 323 (15): 1499–1500. doi:10.1001/jama.2020.3633. PMID 32159735.
- ^ Jump up to: a b Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R (2020). "Features, Evaluation and Treatment Coronavirus (COVID-19)". StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 32150360. Retrieved 18 March 2020.
- ^ Jump up to: a b Heymann DL, Shindo N, et al. (WHO Scientific and Technical Advisory Group for Infectious Hazards) (February 2020). "COVID-19: what is next for public health?". Lancet. 395 (10224): 542–545. doi:10.1016/s0140-6736(20)30374-3. PMC 7138015. PMID 32061313.
- ^ Long B, Brady WJ, Koyfman A, Gottlieb M (July 2020). "Cardiovascular complications in COVID-19". The American Journal of Emergency Medicine. 38 (7): 1504–1507. doi:10.1016/j.ajem.2020.04.048. PMC 7165109. PMID 32317203.
- ^ Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, et al. (November 2020). "Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19)". JAMA Cardiology. 5 (11): 1265–1273. doi:10.1001/jamacardio.2020.3557. PMC 7385689. PMID 32730619. Lay summary.
- ^ Lindner D, Fitzek A, Bräuninger H, Aleshcheva G, Edler C, Meissner K, et al. (November 2020). "Association of Cardiac Infection With SARS-CoV-2 in Confirmed COVID-19 Autopsy Cases". JAMA Cardiology. 5 (11): 1281–1285. doi:10.1001/jamacardio.2020.3551. PMC 7385672. PMID 32730555. Lay summary.
- ^ Siripanthong B, Nazarian S, Muser D, Deo R, Santangeli P, Khanji MY, et al. (September 2020). "Recognizing COVID-19-related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management". Heart Rhythm. 17 (9): 1463–1471. doi:10.1016/j.hrthm.2020.05.001. PMC 7199677. PMID 32387246.
- ^ Basu-Ray I, Almaddah N, Adeboye A, Soos MP (2021). Cardiac Manifestations Of Coronavirus (COVID-19). StatPearls. Treasure Island (FL): StatPearls Publishing. PMID 32310612. Retrieved 5 March 2021.
- ^ Li, Xing; Wang, Ying; Agostinis, Patrizia; Rabson, Arnold; Melino, Gerry; Carafoli, Ernesto; Shi, Yufang; Sun, Erwei (July 2020). "Is hydroxychloroquine beneficial for COVID-19 patients?". Cell Death & Disease. 11 (7): 512. doi:10.1038/s41419-020-2721-8.
- ^ Zou F, Qian Z, Wang Y, Zhao Y, Bai J (September 2020). "Cardiac Injury and COVID-19: A Systematic Review and Meta-analysis". CJC Open. 2 (5): 386–394. doi:10.1016/j.cjco.2020.06.010. PMC 7308771. PMID 32838255.
- ^ Jump up to: a b c Rathore SS, Rojas GA, Sondhi M, Pothuru S, Pydi R, Kancherla N, et al. (July 2021). "Myocarditis associated with Covid-19 disease: A systematic review of published case reports and case series". International Journal of Clinical Practice. n/a (n/a): e14470. doi:10.1111/ijcp.14470. PMID 34235815.
- ^ Tavazzi G, Pellegrini C, Maurelli M, Belliato M, Sciutti F, Bottazzi A, et al. (May 2020). "Myocardial localization of coronavirus in COVID-19 cardiogenic shock". European Journal of Heart Failure. 22 (5): 911–915. doi:10.1002/ejhf.1828. PMC 7262276. PMID 32275347.
- ^ Kesici S, Aykan HH, Orhan D, Bayrakci B (August 2020). "Fulminant COVID-19-related myocarditis in an infant". European Heart Journal. 41 (31): 3021. doi:10.1093/eurheartj/ehaa515. PMC 7314020. PMID 32531024.
- ^ Oudit GY, Kassiri Z, Jiang C, Liu PP, Poutanen SM, Penninger JM, Butany J (July 2009). "SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS". European Journal of Clinical Investigation. 39 (7): 618–25. doi:10.1111/j.1365-2362.2009.02153.x. PMC 7163766. PMID 19453650.
- ^ Nicin L, Abplanalp WT, Mellentin H, Kattih B, Tombor L, John D, et al. (May 2020). "Cell type-specific expression of the putative SARS-CoV-2 receptor ACE2 in human hearts". European Heart Journal. 41 (19): 1804–1806. doi:10.1093/eurheartj/ehaa311. PMC 7184464. PMID 32293672.
- ^ Payus AO, Liew Sat Lin C, Mohd Noh M, Jeffree MS, Ali RA (August 2020). "SARS-CoV-2 infection of the nervous system: A review of the literature on neurological involvement in novel coronavirus disease-(COVID-19)". Bosnian Journal of Basic Medical Sciences. 20 (3): 283–292. doi:10.17305/bjbms.2020.4860. PMC 7416180. PMID 32530389.
- ^ Even Mild Cases Can Cause "COVID-19 Fog", Columbia University Irving Medical Center, 21 September 2020
- ^ Belluck P (11 October 2020), "How Brain Fog Plagues Covid-19 Survivors", The New York Times
- ^ Carod-Artal FJ (May 2020). "Neurological complications of coronavirus and COVID-19". Revista de Neurología. 70 (9): 311–322. doi:10.33588/rn.7009.2020179. PMID 32329044.
- ^ Toscano G, Palmerini F, Ravaglia S, Ruiz L, Invernizzi P, Cuzzoni MG, et al. (June 2020). "Guillain-Barré Syndrome Associated with SARS-CoV-2". The New England Journal of Medicine. 382 (26): 2574–2576. doi:10.1056/NEJMc2009191. PMC 7182017. PMID 32302082.
- ^ Jump up to: a b c d e f g Agyeman AA, Chin KL, Landersdorfer CB, Liew D, Ofori-Asenso R (August 2020). "Smell and Taste Dysfunction in Patients With COVID-19: A Systematic Review and Meta-analysis". Mayo Clinic Proceedings. 95 (8): 1621–1631. doi:10.1016/j.mayocp.2020.05.030. PMC 7275152. PMID 32753137.
- ^ Jump up to: a b c d e f g h Marshall M (January 2021). "COVID's toll on smell and taste: what scientists do and don't know". Nature. 589 (7842): 342–343. Bibcode:2021Natur.589..342M. doi:10.1038/d41586-021-00055-6. PMID 33452511.
- ^ Jump up to: a b Marshall M (September 2020). "How COVID-19 can damage the brain". Nature. 585 (7825): 342–343. Bibcode:2020Natur.585..342M. doi:10.1038/d41586-020-02599-5. PMID 32934351.
- ^ Berlin DA, Gulick RM, Martinez FJ (December 2020). Solomon CG (ed.). "Severe Covid-19". The New England Journal of Medicine. 383 (25): 2451–2460. doi:10.1056/NEJMcp2009575. PMID 32412710. S2CID 218649520.
- ^ Massey PR, Jones KM (October 2020). "Going viral: A brief history of Chilblain-like skin lesions ("COVID toes") amidst the COVID-19 pandemic". Seminars in Oncology. 47 (5): 330–334. doi:10.1053/j.seminoncol.2020.05.012. PMC 7245293. PMID 32736881.
- ^ Jabalameli N, Rajabi F, Firooz A, Rezaei N (January 2021). "The Overlap between Genetic Susceptibility to COVID-19 and Skin Diseases". Immunological Investigations: 1–8. doi:10.1080/08820139.2021.1876086. PMID 33494631.
- ^ Xu L, Liu J, Lu M, Yang D, Zheng X (May 2020). "Liver injury during highly pathogenic human coronavirus infections". Liver International. 40 (5): 998–1004. doi:10.1111/liv.14435. PMC 7228361. PMID 32170806.
- ^ Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB (May 2020). "Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review". JAMA. 323 (18): 1824–1836. doi:10.1001/jama.2020.6019. PMID 32282022.
- ^ "Multisystem inflammatory syndrome in children and adolescents temporally related to COVID-19". World Health Organization (WHO). 15 May 2020. Retrieved 20 May 2020.
- ^ HAN Archive – 00432 (Report). U.S. Centers for Disease Control and Prevention (CDC). 15 May 2020. Retrieved 20 May 2020.
- ^ Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. (February 2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". Lancet. Elsevier. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. PMC 7159299. PMID 31986264.
- ^ "Living with Covid19". NIH Themed Review. National Institute for Health Research. 15 October 2020. doi:10.3310/themedreview_41169.
- ^ "How long does COVID-19 last?". UK COVID Symptom Study. 6 June 2020. Retrieved 15 October 2020.
- ^ "Summary of COVID-19 Long Term Health Effects: Emerging evidence and Ongoing Investigation" (PDF). University of Washington. 1 September 2020. Retrieved 15 October 2020.
- ^ Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. (February 2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". Lancet. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. PMC 7159299. PMID 31986264.
- ^ Jump up to: a b Torres-Castro R, Vasconcello-Castillo L, Alsina-Restoy X, Solis-Navarro L, Burgos F, Puppo H, Vilaró J (November 2020). "Respiratory function in patients post-infection by COVID-19: a systematic review and meta-analysis". Pulmonology. Elsevier BV. 27 (4): 328–337. doi:10.1016/j.pulmoe.2020.10.013. PMC 7687368. PMID 33262076. S2CID 227162748.
- ^ Shaw B, Daskareh M, Gholamrezanezhad A (January 2021). "The lingering manifestations of COVID-19 during and after convalescence: update on long-term pulmonary consequences of coronavirus disease 2019 (COVID-19)". La Radiologia Medica. 126 (1): 40–46. doi:10.1007/s11547-020-01295-8. PMC 7529085. PMID 33006087.
- ^ Zhao YM, Shang YM, Song WB, Li QQ, Xie H, Xu QF, et al. (August 2020). "Follow-up study of the pulmonary function and related physiological characteristics of COVID-19 survivors three months after recovery". EClinicalMedicine. 25: 100463. doi:10.1016/j.ijtb.2020.11.003. PMC 7654356. PMID 32838236.
- COVID-19 symptoms


