Marburg virus
| Marburg virus | |
|---|---|

| |
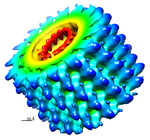
| Transmission electron micrograph of Marburg virus | |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Negarnaviricota |
| Class: | Monjiviricetes |
| Order: | Mononegavirales |
| Family: | Filoviridae |
| Genus: | Marburgvirus |
| Species: | Marburg marburgvirus
|
| Virus: | Marburg virus
|
Marburg virus[1] is a hemorrhagic fever virus of the Filoviridae family of viruses and a member of the species Marburg marburgvirus, genus Marburgvirus. Marburg virus (MARV) causes Marburg virus disease in humans and other primates, a form of viral hemorrhagic fever.[2] The virus is considered to be extremely dangerous. The World Health Organization (WHO) rates it as a Risk Group 4 Pathogen (requiring biosafety level 4-equivalent containment).[3] In the United States, the NIH/National Institute of Allergy and Infectious Diseases ranks it as a Category A Priority Pathogen[4] and the Centers for Disease Control and Prevention lists it as a Category A Bioterrorism Agent.[5] It is also listed as a biological agent for export control by the Australia Group.[6]
The virus can be transmitted by exposure to one species of fruit bats or it can be transmitted between people via body fluids through unprotected sex and broken skin. The disease can cause bleeding (haemorrhage), fever, and other symptoms similar to Ebola. However, Marburg virus is not the same as Ebola, although similar. Actual treatment of the virus after infection is not possible, but early, professional treatment of symptoms like dehydration considerably increases survival chances.[7]
In 2009, expanded clinical trials of an Ebola and Marburg vaccine began in Kampala, Uganda.[8][9]
History[]
Discovery[]
Marburg virus was first described in 1967.[11] It was discovered that year during a set of outbreaks of Marburg virus disease in the German cities of Marburg and Frankfurt and the Yugoslav capital Belgrade. Laboratory workers were exposed to tissues of infected grivet monkeys (the African green monkey, Chlorocebus aethiops) at the Behringwerke, a major industrial plant in Marburg which was then part of Hoechst, and later part of CSL Behring. During the outbreaks, thirty-one people became infected and seven of them died.[12]
Nomenclature[]
The virus is one of two members of the species Marburg marburgvirus, which is included in the genus Marburgvirus, family Filoviridae, and order Mononegavirales. The name Marburg virus is derived from Marburg (the city in Hesse, Germany, where the virus was first discovered) and the taxonomic suffix virus.[1]
Marburg virus was first introduced under this name in 1967.[11] The virus name was changed to Lake Victoria marburgvirus in 2005, confusingly making the only difference in distinguishing between a Marburg virus organism and its species as a whole italicization, as in Lake Victoria marburgvirus.[13][14][15] Still, most scientific articles continued to use the name Marburg virus. Consequently, in 2010, the name Marburg virus was reinstated and the species name changed.[1]
Virology[]
Genome[]

Like all mononegaviruses, marburgvirions contain non-infectious, linear nonsegmented, single-stranded RNA genomes of negative polarity that possess inverse-complementary 3' and 5' termini, do not possess a 5' cap, are not polyadenylated, and are not covalently linked to a protein.[16] Marburgvirus genomes are approximately 19 kbp long and contain seven genes in the order 3'-UTR-NP-VP35-VP40-GP-VP30-VP24-L-5'-UTR.[17]
Structure[]


Like all filoviruses, marburgvirions are filamentous particles that may appear in the shape of a shepherd's crook or in the shape of a "U" or a "6", and they may be coiled, toroid, or branched.[17] Marburgvirions are generally 80 nm in width, but vary somewhat in length. In general, the median particle length of marburgviruses ranges from 795 to 828 nm (in contrast to ebolavirions, whose median particle length was measured to be 974–1,086 nm ), but particles as long as 14,000 nm have been detected in tissue culture.[18]
Marburgvirions consist of seven structural proteins. At the center is the helical ribonucleocapsid, which consists of the genomic RNA wrapped around a polymer of nucleoproteins (NP). Associated with the ribonucleoprotein is the RNA-dependent RNA polymerase (L) with the polymerase cofactor (VP35) and a transcription activator (VP30). The ribonucleoprotein is embedded in a matrix, formed by the major (VP40) and minor (VP24) matrix proteins. These particles are surrounded by a lipid membrane derived from the host cell membrane. The membrane anchors a glycoprotein (GP1,2) that projects 7 to 10 nm spikes away from its surface. While nearly identical to ebolavirions in structure, marburgvirions are antigenically distinct.[citation needed]
Entry[]
Niemann–Pick C1 (NPC1) cholesterol transporter protein appears to be essential for infection with both Ebola and Marburg virus. Two independent studies reported in the same issue of Nature showed that Ebola virus cell entry and replication requires NPC1.[19][20] When cells from patients lacking NPC1 were exposed to Ebola virus in the laboratory, the cells survived and appeared immune to the virus, further indicating that Ebola relies on NPC1 to enter cells. This might imply that genetic mutations in the NPC1 gene in humans could make some people resistant to one of the deadliest known viruses affecting humans. The same studies described similar results with Marburg virus, showing that it also needs NPC1 to enter cells.[19][20] Furthermore, NPC1 was shown to be critical to filovirus entry because it mediates infection by binding directly to the viral envelope glycoprotein[20] and that the second lysosomal domain of NPC1 mediates this binding.[21]
In one of the original studies, a small molecule was shown to inhibit Ebola virus infection by preventing the virus glycoprotein from binding to NPC1.[20][22] In the other study, mice that were heterozygous for NPC1 were shown to be protected from lethal challenge with mouse-adapted Ebola virus.[19]
Replication[]

The Marburg virus life cycle begins with virion attachment to specific cell-surface receptors, followed by fusion of the virion envelope with cellular membranes and the concomitant release of the virus nucleocapsid into the cytosol.
The virus RdRp partially uncoats the nucleocapsid and transcribes the genes into positive-stranded mRNAs, which are then translated into structural and nonstructural proteins. Marburgvirus L binds to a single promoter located at the 3' end of the genome. Transcription either terminates after a gene or continues to the next gene downstream. This means that genes close to the 3' end of the genome are transcribed in the greatest abundance, whereas those toward the 5' end are least likely to be transcribed. The gene order is therefore a simple but effective form of transcriptional regulation.
The most abundant protein produced is the nucleoprotein, whose concentration in the cell determines when L switches from gene transcription to genome replication. Replication results in full-length, positive-stranded antigenomes that are in turn transcribed into negative-stranded virus progeny genome copies. Newly synthesized structural proteins and genomes self-assemble and accumulate near the inside of the cell membrane. Virions bud off from the cell, gaining their envelopes from the cellular membrane they bud from. The mature progeny particles then infect other cells to repeat the cycle.[13]
Ecology[]

In 2009, the successful isolation of infectious MARV was reported from caught healthy Egyptian fruit bats (Rousettus aegyptiacus).[23] This isolation, together with the isolation of infectious RAVV,[23] strongly suggests that Old World fruit bats are involved in the natural maintenance of marburgviruses. Further studies are necessary to establish whether Egyptian rousettes are the actual hosts of MARV and RAVV or whether they get infected via contact with another animal and therefore serve only as intermediate hosts. In 2012 the first experimental infection study of Rousettus aegyptiacus with MARV provided further insight into the possible involvement of these bats in MARV ecology.[24] Experimentally infected bats developed relatively low viremia lasting at least 5 days, but remained healthy and did not develop any notable gross pathology. The virus also replicated to high titers in major organs (liver and spleen), and organs that might possibly be involved in virus transmission (lung, intestine, reproductive organs, salivary gland, kidney, bladder, and mammary gland). The relatively long period of viremia noted in this experiment could possibly also facilitate mechanical transmission by blood sucking arthropods in addition to infection of susceptible vertebrate hosts by direct contact with infected blood.[citation needed]
Evolution[]
The viral strains fall into two clades—Ravn virus and Marburg virus.[25] The Marburg strains can be divided into two—A and B. The A strains were isolated from Uganda (five from 1967), Kenya (1980) and Angola (2004–2005) while the B strains were from the Democratic Republic of the Congo epidemic (1999–2000) and a group of Ugandan isolates isolated in 2007–2009.[citation needed]
The mean evolutionary rate of the whole genome was 3.3 × 10−4 substitutions/site/year (credibility interval 2.0–4.8).The Marburg strains had a mean root time of the most recent common ancestor of 177.9 years ago (95% highest posterior density 87–284) suggesting an origin in the mid 19th century. In contrast, the Ravn strains origin dated back to a mean 33.8 years ago (the early 1980s). The most probable location of the Marburg virus ancestor was Uganda whereas that of the RAVV ancestor was Kenya.[citation needed]
Human disease[]
MARV is one of two Marburg viruses that causes Marburg virus disease (MVD) in humans (in the literature also often referred to as Marburg hemorrhagic fever, MHF). The other one is Ravn virus (RAVV). Both viruses fulfill the criteria for being a member of the species Marburg marburgvirus because their genomes diverge from the prototype Marburg marburgvirus or the Marburg virus variant Musoke (MARV/Mus) by <10% at the nucleotide level.[1]
Recorded outbreaks[]
The Guinean government detected the case from a sample of patients who died on August 2, 2021, in the southern prefecture of Gueckedou near the country's borders with Sierra Leone and Liberia.[26]
| Year | Geographic location | Virus | Human cases | Human deaths | Case fatality rate | Notes |
|---|---|---|---|---|---|---|
| 1967 | Marburg and Frankfurt, West Germany, and Belgrade, Socialist Federal Republic of Yugoslavia | MARV | 31 | 7 | 23% | laboratory leak[27][11][28][29][30][31][32][33][34] |
| 1975 | Rhodesia and Johannesburg, South Africa | MARV | 3 | 1 | 33% | [35][36][37] |
| 1980 | Kenya | MARV | 2 | 1 | 50% | [38] |
| 1987 | Kenya | RAVV | 1 | 1 | 100% | [39][40] |
| 1988 | Koltsovo, Soviet Union | 1 | 1 | 100% | laboratory accident[41] | |
| 1990 | Koltsovo, Soviet Union | MARV | 1 | 1 | 100% | laboratory accident[42] |
| 1998–2000 | Durba and Watsa, Democratic Republic of the Congo | MARV & RAVV | 154 | 128 | 83% | Two different marburgviruses, MARV and Ravn virus (RAVV), cocirculated and caused disease. The number of cases and deaths due to MARV or RAVV infection have not been reported.[43][44][45] |
| 2004–2005 | Angola | MARV | 252 | 227 | 90% | [46][47][48][49][50][51][52] |
| 2007 | Uganda | MARV & RAVV | 4 | 1 | 25% | [23][53] |
| 2008 | Uganda, Netherlands, United States | MARV | 2 | 1 | 50% | [54] |
| 2012 | Uganda | MARV | 18 | 9 | 50% | [55] |
| 2014 | Uganda | MARV | 1 | 1 | 100% | [56][57] |
| 2017 | Uganda | MARV | 3 | 3 | 100% | [58] |
| 2021 | Guinea | MARV | 1 | 1 | 100% | [59][60] |
Prevention[]
The Public Health Agency of Canada has a candidate rVSV vaccine for Marburg virus (rVSV-MARV). Merck was developing it, but discontinued development.[61]
Biological weapon[]
The Soviet Union had an extensive offensive and defensive biological weapons program that included MARV.[62] At least three Soviet research institutes had MARV research programs during the Cold War: the Virology Center of the Scientific-Research Institute for Microbiology in Zagorsk (today Sergiev Posad), the Scientific-Production Association "Vektor" (today the State Research Center of Virology and Biotechnology "Vektor") in Koltsovo, and the Irkutsk Scientific-Research Anti-Plague Institute of Siberia and the Far East in Irkutsk. As most performed research was highly classified, it remains unclear how successful the MARV program was. However, Soviet defector Ken Alibek claimed that a weapon filled with MARV was tested at the Stepnogorsk Scientific Experimental and Production Base in Stepnogorsk, Kazakh Soviet Socialist Republic (today Kazakhstan),[62] suggesting that the development of a MARV biological weapon had reached advanced stages. Independent confirmation for this claim is lacking. At least one laboratory accident with MARV, resulting in the death of Koltsovo researcher Nikolai Ustinov, occurred during the Cold War in the Soviet Union and was first described in detail by Alibek.[62]
MARV is a select agent under US law.[63]
References[]
- ^ Jump up to: a b c d Kuhn, J. H.; Becker, S.; Ebihara, H.; Geisbert, T. W.; Johnson, K. M.; Kawaoka, Y.; Lipkin, W. I.; Negredo, A. I.; Netesov, S. V.; Nichol, S. T.; Palacios, G.; Peters, C. J.; Tenorio, A.; Volchkov, V. E.; Jahrling, P. B. (2010). "Proposal for a revised taxonomy of the family Filoviridae: Classification, names of taxa and viruses, and virus abbreviations". Archives of Virology. 155 (12): 2083–2103. doi:10.1007/s00705-010-0814-x. PMC 3074192. PMID 21046175.
- ^ Spickler, Anna. "Ebolavirus and Marburgvirus Infections" (PDF).
- ^ US Department of Health and Human Services. "Biosafety in Microbiological and Biomedical Laboratories (BMBL) 5th Edition". Retrieved 2011-10-16.
- ^ "Archived copy". Archived from the original on 2011-10-22. Retrieved 2011-10-16.CS1 maint: archived copy as title (link)
- ^ US Centers for Disease Control and Prevention (CDC). "Bioterrorism Agents/Diseases". Archived from the original on 2014-07-22. Retrieved 2011-10-16.
- ^ The Australia Group. "List of Biological Agents for Export Control". Archived from the original on 2011-08-06. Retrieved 2011-10-16.
- ^ Marburg virus disease Fact sheet Updated October 2017 http://www.who.int/mediacentre/factsheets/fs_marburg/en/
- ^ Beth Skwarecki Ebola, Marburg DNA Vaccines Prove Safe in Phase 1 Trial Medscape Medical News, September 17, 2014
- ^ Evaluating an Ebola and a Marburg Vaccine in Uganda U.S. Department of Health & Human Services
- ^ Bharat, C.A.T; Riches, J. D.; Kolesnikova, L.; Welsch, S.; Krähling, V.; Davey, N.; Parsy, M. L.; Becker, S.; Briggs, J. A. G. (2011). Rey, Félix A (ed.). "Cryo-Electron Tomography of Marburg Virus Particles and Their Morphogenesis within Infected Cells". PLOS Biology. 9 (11): e1001196. doi:10.1371/journal.pbio.1001196. PMC 3217011. PMID 22110401.
- ^ Jump up to: a b c Siegert, R.; Shu, H. L.; Slenczka, W.; Peters, D.; Müller, G. (2009). "Zur Ätiologie einer unbekannten, von Affen ausgegangenen menschlichen Infektionskrankheit". Deutsche Medizinische Wochenschrift. 92 (51): 2341–3. doi:10.1055/s-0028-1106144. PMID 4294540.
- ^ Slenczka, Werner; Klenk, Hans Dieter (15 November 2007). "Forty Years of Marburg Virus". The Journal of Infectious Diseases. 196 (s2): S131–S135. doi:10.1086/520551. PMID 17940940.
- ^ Jump up to: a b Feldmann, H.; Geisbert, T. W.; Jahrling, P. B.; Klenk, H.-D.; Netesov, S. V.; Peters, C. J.; Sanchez, A.; Swanepoel, R.; et al. (2005). "Family Filoviridae". In Fauquet, C. M.; Mayo, M. A.; Maniloff, J.; Desselberger, U.; Ball, L. A. (eds.). Virus Taxonomy—Eighth Report of the International Committee on Taxonomy of Viruses. San Diego, US: Elsevier/Academic Press. pp. 645–653. ISBN 978-0-12-370200-5.
- ^ Mayo, M. A. (2002). "ICTV at the Paris ICV: results of the plenary session and the binomial ballot". Archives of Virology. 147 (11): 2254–60. doi:10.1007/s007050200052. S2CID 43887711.
- ^ Kuhn, Jens H.; Jahrling, Peter B. (April 2010). "Clarification and guidance on the proper usage of virus and virus species names". Archives of Virology. 155 (4): 445–453. doi:10.1007/s00705-010-0600-9. PMC 2878132. PMID 20204430.
- ^ Pringle, C. R. (2005). "Order Mononegavirales". In Fauquet, C. M.; Mayo, M. A.; Maniloff, J.; Desselberger, U.; Ball, L. A. (eds.). Virus Taxonomy—Eighth Report of the International Committee on Taxonomy of Viruses. San Diego, US: Elsevier/Academic Press. pp. 609–614. ISBN 978-0-12-370200-5.
- ^ Jump up to: a b Kiley, M. P.; Bowen, E. T.; Eddy, G. A.; Isaäcson, M.; Johnson, K. M.; McCormick, J. B.; Murphy, F. A.; Pattyn, S. R.; Peters, D.; Prozesky, O. W.; Regnery, R. L.; Simpson, D. I.; Slenczka, W.; Sureau, P.; Van Der Groen, G.; Webb, P. A.; Wulff, H. (1982). "Filoviridae: A taxonomic home for Marburg and Ebola viruses?". Intervirology. 18 (1–2): 24–32. doi:10.1159/000149300. PMID 7118520.
- ^ Geisbert, T. W.; Jahrling, P. B. (1995). "Differentiation of filoviruses by electron microscopy". Virus Research. 39 (2–3): 129–150. doi:10.1016/0168-1702(95)00080-1. PMID 8837880.
- ^ Jump up to: a b c Carette JE, Raaben M, Wong AC, Herbert AS, Obernosterer G, Mulherkar N, Kuehne AI, Kranzusch PJ, Griffin AM, Ruthel G, Dal Cin P, Dye JM, Whelan SP, Chandran K, Brummelkamp TR (September 2011). "Ebola virus entry requires the cholesterol transporter Niemann-Pick C1". Nature. 477 (7364): 340–3. Bibcode:2011Natur.477..340C. doi:10.1038/nature10348. PMC 3175325. PMID 21866103. Lay summary – New York Times.
- ^ Jump up to: a b c d Côté M, Misasi J, Ren T, Bruchez A, Lee K, Filone CM, Hensley L, Li Q, Ory D, Chandran K, Cunningham J (September 2011). "Small molecule inhibitors reveal Niemann-Pick C1 is essential for Ebola virus infection". Nature. 477 (7364): 344–8. Bibcode:2011Natur.477..344C. doi:10.1038/nature10380. PMC 3230319. PMID 21866101. Lay summary – New York Times.
- ^ Miller EH, Obernosterer G, Raaben M, Herbert AS, Deffieu MS, Krishnan A, Ndungo E, Sandesara RG, Carette JE, Kuehne AI, Ruthel G, Pfeffer SR, Dye JM, Whelan SP, Brummelkamp TR, Chandran K (March 2012). "Ebola virus entry requires the host-programmed recognition of an intracellular receptor". EMBO Journal. 31 (8): 1947–60. doi:10.1038/emboj.2012.53. PMC 3343336. PMID 22395071.
- ^ Flemming A (October 2011). "Achilles heel of Ebola viral entry". Nat Rev Drug Discov. 10 (10): 731. doi:10.1038/nrd3568. PMID 21959282. S2CID 26888076.
- ^ Jump up to: a b c Towner, J. S.; Amman, B. R.; Sealy, T. K.; Carroll, S. A. R.; Comer, J. A.; Kemp, A.; Swanepoel, R.; Paddock, C. D.; Balinandi, S.; Khristova, M. L.; Formenty, P. B.; Albarino, C. G.; Miller, D. M.; Reed, Z. D.; Kayiwa, J. T.; Mills, J. N.; Cannon, D. L.; Greer, P. W.; Byaruhanga, E.; Farnon, E. C.; Atimnedi, P.; Okware, S.; Katongole-Mbidde, E.; Downing, R.; Tappero, J. W.; Zaki, S. R.; Ksiazek, T. G.; Nichol, S. T.; Rollin, P. E. (2009). Fouchier, Ron A. M. (ed.). "Isolation of Genetically Diverse Marburg Viruses from Egyptian Fruit Bats". PLOS Pathogens. 5 (7): e1000536. doi:10.1371/journal.ppat.1000536. PMC 2713404. PMID 19649327.
- ^ Paweska, J. T.; Jansen Van Vuren, P.; Masumu, J.; Leman, P. A.; Grobbelaar, A. A.; Birkhead, M.; Clift, S.; Swanepoel, R.; Kemp, A. (2012). "Virological and Serological Findings in Rousettus aegyptiacus Experimentally Inoculated with Vero Cells-Adapted Hogan Strain of Marburg Virus". PLOS ONE. 7 (9): e45479. Bibcode:2012PLoSO...745479P. doi:10.1371/journal.pone.0045479. PMC 3444458. PMID 23029039.

- ^ Zehender G, Sorrentino C, Veo C, Fiaschi L, Gioffrè S, Ebranati E, Tanzi E, Ciccozzi M, Lai A, Galli M (2016). "Distribution of Marburg virus in Africa: An evolutionary approach". Infect. Genet. Evol. 44: 8–16. doi:10.1016/j.meegid.2016.06.014. hdl:2434/425196. PMID 27282469.
- ^ dimas (2021-08-10). "Marburg Virus, What Virus Is This?". drhealth. Retrieved 2021-08-10.
- ^ Crozier, Ian; Kuhn, Jens H. (13 May 2020). "A Forgotten Episode of Marburg Virus Disease: Belgrade, Yugoslavia, 1967". Microbiology and Molecular Biology Reviews. 84 (2): e00095-19. doi:10.1128/MMBR.00095-19. PMC 7233485. PMID 32404328.
- ^ Smith, C. E.; Simpson, D. I.; Bowen, E. T.; Zlotnik, I. (1967). "Fatal human disease from vervet monkeys". Lancet. 2 (7526): 1119–21. doi:10.1016/s0140-6736(67)90621-6. PMID 4168558.
- ^ Kissling, R. E.; Robinson, R. Q.; Murphy, F. A.; Whitfield, S. G. (1968). "Agent of disease contracted from green monkeys". Science. 160 (830): 888–890. Bibcode:1968Sci...160..888K. doi:10.1126/science.160.3830.888. PMID 4296724. S2CID 30252321.
- ^ Martini, G. A.; Knauff, H. G.; Schmidt, H. A.; Mayer, G.; Baltzer, G. (2009). "Über eine bisher unbekannte, von Affen eingeschleppte Infektionskrankheit: Marburg-Virus-Krankheit". Deutsche Medizinische Wochenschrift. 93 (12): 559–571. doi:10.1055/s-0028-1105098. PMID 4966280.
- ^ Stille, W.; Böhle, E.; Helm, E.; Van Rey, W.; Siede, W. (2009). "Über eine durch Cercopithecus aethiops übertragene Infektionskrankheit". Deutsche Medizinische Wochenschrift. 93 (12): 572–582. doi:10.1055/s-0028-1105099. PMID 4966281.
- ^ Bonin, O. (1969). "The Cercopithecus monkey disease in Marburg and Frankfurt (Main), 1967". Acta Zoologica et Pathologica Antverpiensia. 48: 319–331. PMID 5005859.
- ^ Jacob, H.; Solcher, H. (1968). "An infectious disease transmitted by Cercopithecus aethiops ("marbury disease") with glial nodule encephalitis". Acta Neuropathologica. 11 (1): 29–44. doi:10.1007/bf00692793. PMID 5748997. S2CID 12791113.
- ^ Stojkovic, L.; Bordjoski, M.; Gligic, A.; Stefanovic, Z. (1971). "Two Cases of Cercopithecus-Monkeys-Associated Haemorrhagic Fever". In Martini, G. A.; Siegert, R. (eds.). Marburg Virus Disease. Berlin, Germany: Springer-Verlag. pp. 24–33. ISBN 978-0-387-05199-4.
- ^ Gear, J. S.; Cassel, G. A.; Gear, A. J.; Trappler, B.; Clausen, L.; Meyers, A. M.; Kew, M. C.; Bothwell, T. H.; Sher, R.; Miller, G. B.; Schneider, J.; Koornhof, H. J.; Gomperts, E. D.; Isaäcson, M.; Gear, J. H. (1975). "Outbreake of Marburg virus disease in Johannesburg". British Medical Journal. 4 (5995): 489–493. doi:10.1136/bmj.4.5995.489. PMC 1675587. PMID 811315.
- ^ Gear, J. H. (1977). "Haemorrhagic fevers of Africa: An account of two recent outbreaks". Journal of the South African Veterinary Association. 48 (1): 5–8. PMID 406394.
- ^ Conrad, J. L.; Isaacson, M.; Smith, E. B.; Wulff, H.; Crees, M.; Geldenhuys, P.; Johnston, J. (1978). "Epidemiologic investigation of Marburg virus disease, Southern Africa, 1975". The American Journal of Tropical Medicine and Hygiene. 27 (6): 1210–5. doi:10.4269/ajtmh.1978.27.1210. PMID 569445.
- ^ Smith, D. H.; Johnson, B. K.; Isaacson, M.; Swanapoel, R.; Johnson, K. M.; Killey, M.; Bagshawe, A.; Siongok, T.; Keruga, W. K. (1982). "Marburg-virus disease in Kenya". Lancet. 1 (8276): 816–820. doi:10.1016/S0140-6736(82)91871-2. PMID 6122054. S2CID 42832324.
- ^ Marburg and Ebola viruses; Advances in Virus Research; Volume 47, 1996, Pages 1–52
- ^ Known Cases and Outbreaks of Marburg Hemorrhagic Fever, in Chronological Order
- ^ Beer, B.; Kurth, R.; Bukreyev, A. (1999). "Characteristics of Filoviridae: Marburg and Ebola viruses". Die Naturwissenschaften. 86 (1): 8–17. Bibcode:1999NW.....86....8B. doi:10.1007/s001140050562. PMID 10024977. S2CID 25789824.
- ^ Nikiforov, V. V.; Turovskiĭ, I.; Kalinin, P. P.; Akinfeeva, L. A.; Katkova, L. R.; Barmin, V. S.; Riabchikova, E. I.; Popkova, N. I.; Shestopalov, A. M.; Nazarov, V. P. (1994). "A case of a laboratory infection with Marburg fever". Zhurnal Mikrobiologii, Epidemiologii, I Immunobiologii (3): 104–6. PMID 7941853.
- ^ Bertherat, E.; Talarmin, A.; Zeller, H. (1999). "Democratic Republic of the Congo: Between civil war and the Marburg virus. International Committee of Technical and Scientific Coordination of the Durba Epidemic". Médecine Tropicale : Revue du Corps de Santé Colonial. 59 (2): 201–4. PMID 10546197.
- ^ Bausch, D. G.; Borchert, M.; Grein, T.; Roth, C.; Swanepoel, R.; Libande, M. L.; Talarmin, A.; Bertherat, E.; Muyembe-Tamfum, J. J.; Tugume, B.; Colebunders, R.; Kondé, K. M.; Pirad, P.; Olinda, L. L.; Rodier, G. R.; Campbell, P.; Tomori, O.; Ksiazek, T. G.; Rollin, P. E. (2003). "Risk Factors for Marburg Hemorrhagic Fever, Democratic Republic of the Congo". Emerging Infectious Diseases. 9 (12): 1531–7. doi:10.3201/eid0912.030355. PMC 3034318. PMID 14720391.
- ^ Bausch, D. G.; Nichol, S. T.; Muyembe-Tamfum, J. J.; Borchert, M.; Rollin, P. E.; Sleurs, H.; Campbell, P.; Tshioko, F. K.; Roth, C.; Colebunders, R.; Pirard, P.; Mardel, S.; Olinda, L. A.; Zeller, H.; Tshomba, A.; Kulidri, A.; Libande, M. L.; Mulangu, S.; Formenty, P.; Grein, T.; Leirs, H.; Braack, L.; Ksiazek, T.; Zaki, S.; Bowen, M. D.; Smit, S. B.; Leman, P. A.; Burt, F. J.; Kemp, A.; Swanepoel, R. (2006). "Marburg Hemorrhagic Fever Associated with Multiple Genetic Lineages of Virus" (PDF). New England Journal of Medicine. 355 (9): 909–919. doi:10.1056/NEJMoa051465. PMID 16943403.
- ^ Hovette, P. (2005). "Epidemic of Marburg hemorrhagic fever in Angola". Médecine Tropicale: Revue du Corps de Santé Colonial. 65 (2): 127–8. PMID 16038348.
- ^ Ndayimirije, N.; Kindhauser, M. K. (2005). "Marburg Hemorrhagic Fever in Angola—Fighting Fear and a Lethal Pathogen". New England Journal of Medicine. 352 (21): 2155–7. doi:10.1056/NEJMp058115. PMID 15917379.
- ^ Towner, J. S.; Khristova, M. L.; Sealy, T. K.; Vincent, M. J.; Erickson, B. R.; Bawiec, D. A.; Hartman, A. L.; Comer, J. A.; Zaki, S. R.; Ströher, U.; Gomes Da Silva, F.; Del Castillo, F.; Rollin, P. E.; Ksiazek, T. G.; Nichol, S. T. (2006). "Marburgvirus Genomics and Association with a Large Hemorrhagic Fever Outbreak in Angola". Journal of Virology. 80 (13): 6497–6516. doi:10.1128/JVI.00069-06. PMC 1488971. PMID 16775337.
- ^ Jeffs, B.; Roddy, P.; Weatherill, D.; De La Rosa, O.; Dorion, C.; Iscla, M.; Grovas, I.; Palma, P. P.; Villa, L.; Bernal, O.; Rodriguez-Martinez, J.; Barcelo, B.; Pou, D.; Borchert, M. (2007). "The Médecins Sans Frontières Intervention in the Marburg Hemorrhagic Fever Epidemic, Uige, Angola, 2005. I. Lessons Learned in the Hospital" (PDF). The Journal of Infectious Diseases. 196: S154–S161. doi:10.1086/520548. PMID 17940944.
- ^ Roddy, P.; Weatherill, D.; Jeffs, B.; Abaakouk, Z.; Dorion, C.; Rodriguez-Martinez, J.; Palma, P. P.; De La Rosa, O.; Villa, L.; Grovas, I.; Borchert, M. (2007). "The Médecins Sans Frontières Intervention in the Marburg Hemorrhagic Fever Epidemic, Uige, Angola, 2005. II. Lessons Learned in the Community" (PDF). The Journal of Infectious Diseases. 196: S162–7. doi:10.1086/520544. PMID 17940945.
- ^ Roddy, P.; Marchiol, A.; Jeffs, B.; Palma, P. P.; Bernal, O.; De La Rosa, O.; Borchert, M. (2009). "Decreased peripheral health service utilisation during an outbreak of Marburg haemorrhagic fever, Uíge, Angola, 2005" (PDF). Transactions of the Royal Society of Tropical Medicine and Hygiene. 103 (2): 200–2. doi:10.1016/j.trstmh.2008.09.001. hdl:10144/41786. PMID 18838150.
- ^ Roddy, P.; Thomas, S. L.; Jeffs, B.; Nascimento Folo, P.; Pablo Palma, P.; Moco Henrique, B.; Villa, L.; Damiao Machado, F. P.; Bernal, O.; Jones, S. M.; Strong, J. E.; Feldmann, H.; Borchert, M. (2010). "Factors Associated with Marburg Hemorrhagic Fever: Analysis of Patient Data from Uige, Angola". The Journal of Infectious Diseases. 201 (12): 1909–18. doi:10.1086/652748. PMC 3407405. PMID 20441515.
- ^ Adjemian, J.; Farnon, E. C.; Tschioko, F.; Wamala, J. F.; Byaruhanga, E.; Bwire, G. S.; Kansiime, E.; Kagirita, A.; Ahimbisibwe, S.; Katunguka, F.; Jeffs, B.; Lutwama, J. J.; Downing, R.; Tappero, J. W.; Formenty, P.; Amman, B.; Manning, C.; Towner, J.; Nichol, S. T.; Rollin, P. E. (2011). "Outbreak of Marburg Hemorrhagic Fever Among Miners in Kamwenge and Ibanda Districts, Uganda, 2007". Journal of Infectious Diseases. 204 (Suppl 3): S796–9. doi:10.1093/infdis/jir312. PMC 3203392. PMID 21987753.
- ^ Timen, A.; Koopmans, M. P.; Vossen, A. C.; Van Doornum, G. J.; Günther, S.; Van Den Berkmortel, F.; Verduin, K. M.; Dittrich, S.; Emmerich, P.; Osterhaus, A. D. M. E.; Van Dissel, J. T.; Coutinho, R. A. (2009). "Response to Imported Case of Marburg Hemorrhagic Fever, the Netherlands". Emerging Infectious Diseases. 15 (8): 1171–5. doi:10.3201/eid1508.090015. PMC 2815969. PMID 19751577.
- ^ "Marburg hemorrhagic fever outbreak continues in Uganda". October 2012.
- ^ "1st LD-Writethru: Deadly Marburg hemorrhagic fever breaks out in Uganda". October 5, 2014.
- ^ Ntale, Samson (October 8, 2014). "99 in Uganda quarantined after Marburg virus death". CNN. Retrieved 2014-10-19.
- ^ "Marburg virus disease – Uganda Disease outbreak news". October 25, 2017.
- ^ "Guinea records probable case of Ebola-like Marburg virus". Reuters. 6 August 2021. Retrieved 7 August 2021.
- ^ "West Africa's first-ever case of Marburg virus disease confirmed in Guinea". ReliefWeb. Retrieved 8 August 2021.
- ^ "MSF's response to CEPI's policy regarding equitable access". Médecins Sans Frontières Access Campaign.
In vaccine development, access to know how is important. Knowledge and expertise including but not limited to purification techniques, cell lines, materials, software codes and their transfer of this to alternative manufacturers in the event the awardee discontinues development of a promising vaccine is critically important. The recent example of Merck abandoning the development of rVSV vaccines for Marburg (rVSV-MARV) and for Sudan-Ebola (rVSV-SUDV) is a case in point. Merck continues to retain vital know-how on the rVSV platform as it developed the rVSV vaccine for Zaire-Ebola (rVSV-ZEBOV) with funding support from GAVI. While it has transferred the rights on these vaccines back to Public Health Agency of Canada, there is no mechanism to share know how on the rVSV platform with other vaccine developers who would like to also use rVSV as a vector against other pathogens.
- ^ Jump up to: a b c Alibek, Steven; Handelman (1999). Biohazard: The Chilling True Story of the Largest Covert Biological Weapons Program in the World—Told from Inside by the Man Who Ran It. New York: Random House. ISBN 978-0-385-33496-9.
- ^ US Animal and Plant Health Inspection Service (APHIS) and US Centers for Disease Control and Prevention (CDC). "National Select Agent Registry (NSAR)". Retrieved 2011-10-16.
Further reading[]
- Klenk, Hans-Dieter (1999). Marburg and Ebola Viruses. Current Topics in Microbiology and Immunology. 235. Berlin, Germany: Springer-Verlag. ISBN 978-3-540-64729-4.
- Klenk, Hans-Dieter; Feldmann, Heinz (2004). Ebola and Marburg Viruses: Molecular and Cellular Biology. Wymondham, Norfolk, UK: Horizon Bioscience. ISBN 978-1-904933-49-6.
- Kuhn, Jens H. (2008). Filoviruses: A Compendium of 40 Years of Epidemiological, Clinical, and Laboratory Studies. Archives of Virology Supplement, vol. 20. Vienna, Austria: SpringerWienNewYork. ISBN 978-3-211-20670-6.
- Martini, G. A.; Siegert, R. (1971). Marburg Virus Disease. Berlin, Germany: Springer-Verlag. ISBN 978-0-387-05199-4.
- Ryabchikova, Elena I.; Price, Barbara B. (2004). Ebola and Marburg Viruses: A View of Infection Using Electron Microscopy. Columbus, Ohio, US: Battelle Press. ISBN 978-1-57477-131-2.
External links[]
| Wikimedia Commons has media related to Marburgvirus. |
- Marburgviruses
- Animal viral diseases
- Arthropod-borne viral fevers and viral haemorrhagic fevers
- Biological weapons
- Hemorrhagic fevers
- Tropical diseases
- Primate diseases
- Zoonoses
- Filoviridae