Oxendolone
 | |
| Clinical data | |
|---|---|
| Trade names | Prostetin, Roxenone |
| Other names | TSAA-291; 16β-Ethyl-19-nortestosterone; 16β-Ethylestr-4-en-17β-ol-3-one |
| Routes of administration | Intramuscular injection[1][2][3][4] |
| Drug class | Steroidal antiandrogen; Progestogen; Progestin |
| Pharmacokinetic data | |
| Bioavailability | Oral: Very low (1% in dogs)[5] |
| Elimination half-life | IM: 5.0–6.6 days.[4][6] |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| CompTox Dashboard (EPA) | |
| Chemical and physical data | |
| Formula | C20H30O2 |
| Molar mass | 302.458 g·mol−1 |
| 3D model (JSmol) | |
SMILES
| |
InChI
| |
Oxendolone, sold under the brand names Prostetin and Roxenone, is an antiandrogen and progestin medication which is used in Japan in the treatment of enlarged prostate.[7][8][9][10][11] However, this use is controversial due to concerns about its clinical efficacy.[11] Oxendolone is not effective by mouth and must be given by injection into muscle.[5][1][2][3][4]
Oxendolone is an antiandrogen, and hence is an antagonist of the androgen receptor, the biological target of androgens like testosterone and dihydrotestosterone.[12][13][14][15][6] It is also a progestin, or a synthetic progestogen, and hence is an agonist of the progesterone receptor, the biological target of progestogens like progesterone.[12][13][14][15] Due to its progestogenic activity, oxendolone has antigonadotropic effects.[16][17] Oxendolone has no other important hormonal activity...
Oxendolone was introduced for medical use in 1981.[8] It is used only in Japan.[8][11]
Medical uses[]
Oxendolone is used in the treatment of benign prostatic hyperplasia (BPH) in Japan.[8][11] It has been used at a dosage of 200 mg once every 2 weeks via intramuscular injection.[17] Although it is approved for the treatment of BPH in Japan, concerns have been raised about its use for this condition due to poor efficacy seen in clinical trials.[11]
Side effects[]
Pharmacology[]
Pharmacodynamics[]
Oxendolone binds to the androgen receptor (Ki = 320 nM) and progesterone receptor (Ki = 20 nM) and acts as a weak but clinically relevant inhibitor of 5α-reductase (IC50 = 1.4 μM).[12][13][14][15] The relative binding affinity of oxendolone for the androgen receptor is 0.8 to 3.6% of that of metribolone.[18][19] Oxendolone is not a silent antagonist of the androgen receptor but is rather predominantly antagonistic with weak agonistic activity;[13] for this reason, it has been described as a selective androgen receptor modulator.[20] The medication has potent antigonadotropic effects via its progestogenic activity.[16] It has been found to suppress luteinizing hormone and testosterone levels to an equivalent extent as allylestrenol and chlormadinone acetate, which are two progestins that are similarly used at high doses to treat BPH.[17]
Pharmacokinetics[]
The oral bioavailability of oxendolone in dogs is extremely low, 1% at most.[5] Due to its low oral bioavailability, oxendolone is administered by intramuscular injection in humans.[1][2][3][4] Its elimination half-life via this route is 5.0 to 6.6 days.[4]
Chemistry[]
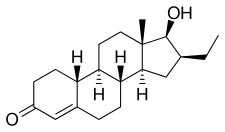
Oxendolone, also known as 16β-ethyl-19-nortestosterone or 16β-ethylestr-4-en-17β-ol-3-one, is a synthetic estrane steroid and a derivative of testosterone and 19-nortestosterone (nandrolone).[7][8]
The acetate ester of oxendolone is known as TSAA-328, while the caproate ester of oxendolone is known as TSAA-330.[21] They were never marketed.[21]
History[]
Oxendolone has been marketed in Japan by Takeda since 1981.[8]
Society and culture[]
Generic names[]
Oxendolone is the generic name of the drug and its INN, USAN, and JAN.[7][22] It is also known by its developmental code name TSAA-291.[7][22]
Brand names[]
Oxendolone is or has been sold under the brand names Prostetin and Roxenone.[7][22]
Availability[]
Oxendolone is marketed only in Japan.[22]
References[]
- ^ a b c Henkler G, Klotzbach M, Koch H, Müller W, Richter J (1982). "[Progress in the area of drug development. 15]". Pharmazie (in German). 37 (11): 753–65. PMID 6131442.
[Oxendolone] has been clinically tested in Japan (weekly intramuscular injection of 200-400 mg) in prostatic hypertrophy.
- ^ a b c Hikichi Y, Yamaoka M, Kusaka M, Hara T (2015). "Selective androgen receptor modulator activity of a steroidal antiandrogen TSAA-291 and its cofactor recruitment profile". Eur. J. Pharmacol. 765: 322–31. doi:10.1016/j.ejphar.2015.08.052. PMID 26335395.
According to the clinical data of TSAA-291, the plasma level of TSAA-291 after weekly intramuscular administration at 400 mg/kg for 12 weeks is approximately 100 nM (Drug Information).
- ^ a b c Ostri P, Swartz R, Meyhoff HH, Petersen JH, Lindgård G, Frimodt-Møller C, Andersson T, Nielsen MS (1989). "Antiandrogenic treatment of benign prostatic hyperplasia: a placebo controlled trial". Urol. Res. 17 (1): 29–33. doi:10.1007/bf00261046. PMID 2466359. S2CID 30551043.
Thirty patients were treated with weekly injections of oxendolone 200 mg during a 3 months' period, and 30 patients were allocated to placebo treatment.
- ^ a b c d e Midgley I, Fowkes AG, Darragh A, Lambe R, Chasseaud LF, Taylor T (1983). "The metabolic fate of the anti-androgenic agent, oxendolone, in man". Steroids. 41 (4): 521–36. doi:10.1016/0039-128x(83)90092-2. PMID 6419414. S2CID 41224726.
After intramuscular administration of 16β-ethyl-17β-hydroxy-4-[4-14C] estren-3-one (14C-oxendolone; 300 mg) to 3 human subjects, [...]
- ^ a b c Michael J. Rathbone; Jonathan Hadgraft; Michael S. Roberts (7 November 2002). Modified-Release Drug Delivery Technology. CRC Press. pp. 368–. ISBN 978-0-8247-0869-6.
- ^ a b Gao, Wenqing; Bohl, Casey E.; Dalton, James T. (2005). "Chemistry and Structural Biology of Androgen Receptor". Chemical Reviews. 105 (9): 3352–3370. doi:10.1021/cr020456u. ISSN 0009-2665. PMC 2096617. PMID 16159155.
- ^ a b c d e J. Elks (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 914–. ISBN 978-1-4757-2085-3.
- ^ a b c d e f William Andrew Publishing (22 October 2013). Pharmaceutical Manufacturing Encyclopedia, 3rd Edition. Elsevier. pp. 2935–. ISBN 978-0-8155-1856-3.
- ^ Martin Negwer; Hans-Georg Scharnow (2001). Organic-chemical drugs and their synonyms: (an international survey). Wiley-VCH. p. 2023. ISBN 978-3-527-30247-5.
- ^ Tan, MH Eileen; Li, Jun; Xu, H Eric; Melcher, Karsten; Yong, Eu-leong (2014). "Androgen receptor: structure, role in prostate cancer and drug discovery". Acta Pharmacologica Sinica. 36 (1): 3–23. doi:10.1038/aps.2014.18. ISSN 1671-4083. PMC 4571323. PMID 24909511.
- ^ a b c d e Ishizuka, Osamu; Nishizawa, Osamu; Hirao, Yoshihiko; Ohshima, Shinichi (2002). "Evidence-based meta-analysis of pharmacotherapy for benign prostatic hypertrophy". International Journal of Urology. 9 (11): 607–612. doi:10.1046/j.1442-2042.2002.00539.x. ISSN 0919-8172. PMID 12534901.
- ^ a b c Annual Reports in Medicinal Chemistry. Academic Press. 8 September 1989. pp. 199–. ISBN 978-0-08-058368-6.
- ^ a b c d Annual report of Shionogi Research Laboratories. 1991. pp. 76–77.
- ^ a b c Kirby, RogerS.; Christmas, Timothy (1991). "The potential value of 5-alpha-reductase inhibition in the treatment of bladder outflow obstruction due to benign prostatic hyperplasia". World Journal of Urology. 9 (1). doi:10.1007/BF00184713. ISSN 0724-4983. S2CID 38790542.
- ^ a b c Bashirelahi, N.; Ganesan, S.; Ekiko, D.B.; Young, J.D.; Shida, K.; Yamanaka, H.; Takahashi, E. (1986). "Effect of 16β-ethyl-17β-hydroxy-4-estren-3-one (tsaa-291) on the binding of promegestone (r5020) and methyltrienolone (r1881) to hyperplastic and neoplastic human prostate". Journal of Steroid Biochemistry. 25 (3): 367–374. doi:10.1016/0022-4731(86)90249-9. ISSN 0022-4731. PMID 2430141.
- ^ a b Sudo, K.; Yamazaki, I.; Masuoka, M.; Nakayama, R. (1979). "IV. EFFECTS OF THE ANTI-ANDROGEN TSAA-291 (16β-ETHYL-17β-HYDROXY-4-OESTREN-3-ONE) ON THE SECRETION OF GONADOTROPHINS". European Journal of Endocrinology. 92 (3 Supplb): S53–S66. doi:10.1530/acta.0.092S053. ISSN 0804-4643. PMID 294107.
- ^ a b c Katayama T, Umeda K, Kazama T (November 1986). "[Hormonal environment and antiandrogenic treatment in benign prostatic hypertrophy]". Hinyokika Kiyo (in Japanese). 32 (11): 1584–9. PMID 2435122.
- ^ Dalton, James T.; Gao, Wenqing (2010). "Androgen Receptor". Nuclear Receptors: 143–182. doi:10.1007/978-90-481-3303-1_6. ISBN 978-90-481-3302-4.
- ^ Wakeling AE, Furr BJ, Glen AT, Hughes LR (December 1981). "Receptor binding and biological activity of steroidal and nonsteroidal antiandrogens". J. Steroid Biochem. 15: 355–9. doi:10.1016/0022-4731(81)90297-1. PMID 7339263.
- ^ Hikichi, Yukiko; Yamaoka, Masuo; Kusaka, Masami; Hara, Takahito (2015). "Selective androgen receptor modulator activity of a steroidal antiandrogen TSAA-291 and its cofactor recruitment profile". European Journal of Pharmacology. 765: 322–331. doi:10.1016/j.ejphar.2015.08.052. ISSN 0014-2999. PMID 26335395.
- ^ a b Masuoka M, Masaki T, Yamazaki I, Hori T, Nakayama R (1979). "Anti-androgen TSAA-291. III. Hormonal spectra of anti-androgen TSAA-291 (16 beta-ethyl-17 beta-hydroxy-4-oestren-3-one) and its derivatives". Acta Endocrinol Suppl (Copenh). 229: 36–52. doi:10.1530/acta.0.092s036. PMID 294106.
- ^ a b c d "Oxandrolone Uses, Side Effects & Warnings".
- 5α-Reductase inhibitors
- Secondary alcohols
- Antigonadotropins
- Drugs for benign prostatic hyperplasia
- Estranes
- Ketones
- Progestogens
- Steroidal antiandrogens