show GABA A receptor positive modulatorsAlcohols
Butanol Chloralodol Chlorobutanol (cloretone) Ethanol (alcohol) (alcoholic drink )Ethchlorvynol Isobutanol Isopropanol Menthol Methanol Methylpentynol Pentanol Petrichloral Propanol tert -Butanol (2M2P)tert -Pentanol (2M2B)Tribromoethanol Trichloroethanol Triclofos Trifluoroethanol Barbiturates
Allobarbital Alphenal Amobarbital Aprobarbital Barbexaclone Barbital Benzobarbital Benzylbutylbarbiturate Brallobarbital Brophebarbital Butabarbital/Secbutabarbital Butalbital Buthalital Butobarbital Butallylonal Carbubarb Crotylbarbital Cyclobarbital Cyclopentobarbital Difebarbamate Enallylpropymal Ethallobarbital Eterobarb Febarbamate Heptabarb Heptobarbital Hexethal Hexobarbital Metharbital Methitural Methohexital Methylphenobarbital Narcobarbital Nealbarbital Pentobarbital Phenallymal Phenobarbital Phetharbital Primidone Probarbital Propallylonal Propylbarbital Proxibarbital Reposal Secobarbital Sigmodal Spirobarbital Talbutal Tetrabamate Tetrabarbital Thialbarbital Thiamylal Thiobarbital Thiobutabarbital Thiopental Thiotetrabarbital Valofane Vinbarbital Vinylbital Benzodiazepines Carbamates
Carisbamate Carisoprodol Clocental Cyclarbamate Difebarbamate Emylcamate Ethinamate Febarbamate Felbamate Hexapropymate Hydroxyphenamate Lorbamate Mebutamate Meprobamate Nisobamate Pentabamate Phenprobamate Procymate Styramate Tetrabamate Tybamate Flavonoids
Ampelopsin (dihydromyricetin) Apigenin Baicalein Baicalin Catechin EGC EGCG Hispidulin Luteolin Skullcap constituents (e.g., baicalin )Wogonin Imidazoles
Etomidate Metomidate Propoxate Kava constituents
Desmethoxyyangonin Kavain Methysticin Yangonin Monoureides
Acecarbromal Apronal (apronalide) Bromisoval Carbromal Neuroactive steroids
Acebrochol Allopregnanolone (brexanolone) Alfadolone Alfaxalone 3α-Androstanediol Androstenol Androsterone Certain anabolic-androgenic steroids
Cholesterol DHDOC 3α-DHP 5α-DHP 5β-DHP DHT Etiocholanolone Ganaxolone Hydroxydione Minaxolone ORG-20599 ORG-21465 P1-185 Pregnanolone (eltanolone) Progesterone Renanolone Testosterone THDOC Zuranolone Nonbenzodiazepines
Cyclopyrrolones Eszopiclone Pagoclone Pazinaclone Suproclone Suriclone Zopiclone Imidazopyridines Alpidem DS-1 Necopidem Saripidem Zolpidem Pyrazolopyrimidines Divaplon Fasiplon Indiplon Lorediplon Ocinaplon Panadiplon Taniplon Zaleplon Others : Adipiplon CGS-8216 CGS-9896 CGS-13767 CGS-20625 CL-218,872 CP-615,003 ELB-139 GBLD-345 Imepitoin JM-1232 L-838,417 Lirequinil (Ro41-3696) NS-2664 NS-2710 NS-11394 Pipequaline ROD-188 RWJ-51204 SB-205,384 SX-3228 TP-003 TPA-023 TP-13 U-89843A U-90042 Viqualine Y-23684 Phenols
Fospropofol Propofol Thymol Piperidinediones
Glutethimide Methyprylon Piperidione Pyrithyldione Pyrazolopyridines
Cartazolate Etazolate ICI-190,622 Tracazolate Quinazolinones
Afloqualone Cloroqualone Diproqualone Etaqualone Mebroqualone Mecloqualone Methaqualone Methylmethaqualone Nitromethaqualone SL-164 Volatiles /gases
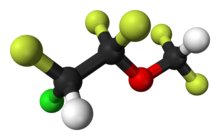
Acetone Acetophenone Acetylglycinamide chloral hydrate Aliflurane Benzene Butane Butylene Centalun Chloral Chloral betaine Chloral hydrate Chloroform Cryofluorane Desflurane Dichloralphenazone Dichloromethane Diethyl ether Enflurane Ethyl chloride Ethylene Fluroxene Gasoline Halopropane Halothane Isoflurane Kerosine Methoxyflurane Methoxypropane Nitric oxide Nitrogen Nitrous oxide Norflurane Paraldehyde Propane Propylene Roflurane Sevoflurane Synthane Teflurane Toluene Trichloroethane (methyl chloroform) Trichloroethylene Vinyl ether Others/unsorted
3-Hydroxybutanal Avermectins (e.g., ivermectin )Bromide compounds (e.g., lithium bromide , potassium bromide , sodium bromide )Carbamazepine Chloralose Chlormezanone Clomethiazole DEABL Dihydroergolines (e.g., dihydroergocryptine , , dihydroergotamine , ergoloid (dihydroergotoxine) )Efavirenz Etazepine Etifoxine Fenamates (e.g., flufenamic acid , mefenamic acid , niflumic acid , tolfenamic acid )Fluoxetine Flupirtine Hopantenic acid Lanthanum Lavender oil Lignans (e.g., 4-O-methylhonokiol , honokiol , magnolol , obovatol )Loreclezole Menthyl isovalerate (validolum) Monastrol Niacin Niacinamide Org 25,435 Phenytoin Propanidid Retigabine (ezogabine) Safranal Seproxetine Stiripentol (e.g., sulfonmethane (sulfonal) , tetronal , trional )
Terpenoids (e.g., borneol )Topiramate Valerian constituents (e.g., isovaleric acid , isovaleramide , valerenic acid , )Unsorted benzodiazepine site positive modulators: α-Pinene See also: Receptor/signaling modulators • GABA receptor modulators • GABA metabolism/transport modulators
show Receptor (ligands )
GlyR
Agonists: β-Alanine β-ABA (BABA) Caesium D -AlanineD -SerineGABA Glycine Hypotaurine Ivermectin L -AlanineL -ProlineL -SerineL -ThreonineMilacemide Picolinic acid Propofol Quisqualamine Sarcosine Taurine Positive modulators: Alcohols (e.g., , chlorobutanol (chloretone) , ethanol (alcohol) , tert -butanol (2M2P)tribromoethanol , trichloroethanol , trifluoroethanol )Alkylbenzene sulfonate Anandamide Barbiturates (e.g., pentobarbital , sodium thiopental )Chlormethiazole Dihydropyridines (e.g., nicardipine )Etomidate Ginseng constituents (e.g., ginsenosides (e.g., ))Glutamic acid (glutamate) Ivermectin Ketamine Neuroactive steroids (e.g., alfaxolone , pregnenolone (eltanolone) , pregnenolone acetate , minaxolone , ORG-20599 )Nitrous oxide Penicillin G Propofol Tamoxifen Tetrahydrocannabinol Triclofos (e.g., atropine , bemesetron , cocaine , , tropisetron , zatosetron )
Volatiles /gases (e.g., chloral hydrate , chloroform , desflurane , diethyl ether (ether) , enflurane , halothane , isoflurane , methoxyflurane , sevoflurane , toluene , trichloroethane (methyl chloroform) , trichloroethylene )Xenon Zinc Antagonists: Bicuculline Brucine Cacotheline Caffeine Colchicine Colubrine Dendrobine Endocannabinoids (e.g., 2-AG , anandamide (AEA) )Gaboxadol (THIP) Gelsemine Isobutyric acid Isonipecotic acid Laudanosine Nipecotic acid Pitrazepin Quinolines (e.g., , , , , , )Sinomenine Strychnine Thiocolchicoside Tutin Negative modulators: Amiloride Benzodiazepines (e.g., bromazepam , clonazepam , diazepam , flunitrazepam , flurazepam )Daidzein Dihydropyridines (e.g., nicardipine , nifedipine , nitrendipine )Furosemide Genistein Ginkgo constituents (e.g., bilobalide , ginkgolides (e.g., , ginkgolide B , , , ))Imipramine NBQX Neuroactive steroids (e.g., , , deoxycorticosterone , DHEA sulfate , pregnenolone sulfate , progesterone )Opioids (e.g., codeine , dextromethorphan , dextrorphan , levomethadone , levorphanol , morphine , oripavine , pethidine , thebaine )Picrotoxin (i.e., picrotin and picrotoxinin )Riluzole (e.g., bemesetron , , tropisetron , zatosetron )
Verapamil Zinc NMDAR
Transporter (blockers )
See also
Receptor/signaling modulators GABA receptor modulators GABAA receptor positive modulators Ionotropic glutamate receptor modulators
show AMPAR
Antagonists: Becampanel Caroverine CNQX Dasolampanel DNQX Fanapanel (MPQX) Kaitocephalin Kynurenic acid Kynurenine Licostinel (ACEA-1021) NBQX Selurampanel Tezampanel Theanine Topiramate Zonampanel ; Negative allosteric modulators: Barbiturates (e.g., pentobarbital , sodium thiopental )Cyclopropane Enflurane Ethanol (alcohol) Evans blue GYKI-52466 Halothane Irampanel Isoflurane Perampanel Pregnenolone sulfate Sevoflurane Talampanel ; Unknown/unsorted antagonists: Minocycline KAR
Agonists: Main site agonists: 5-Iodowillardiine AMPA Domoic acid Glutamate Ibotenic acid Kainic acid Proline Quisqualic acid ; Positive allosteric modulators: Cyclothiazide
Diazoxide Enflurane Halothane Isoflurane Antagonists: CNQX Dasolampanel DNQX Kaitocephalin Kynurenic acid Licostinel (ACEA-1021) NBQX NS102 Selurampanel Tezampanel Theanine Topiramate UBP-302 ; Negative allosteric modulators: Barbiturates (e.g., pentobarbital , sodium thiopental )Enflurane Ethanol (alcohol) Evans blue Pregnenolone sulfate NMDAR
See also: Receptor/signaling modulators Metabotropic glutamate receptor modulators Glutamate metabolism/transport modulators
show 5-HT1
5-HT1A
Agonists: 8-OH-DPAT Adatanserin Amphetamine Antidepressants (e.g., etoperidone , hydroxynefazodone , nefazodone , trazodone , triazoledione , vilazodone , vortioxetine )Atypical antipsychotics (e.g., aripiprazole , asenapine , brexpiprazole , cariprazine , clozapine , lurasidone , quetiapine , ziprasidone )Azapirones (e.g., buspirone , eptapirone , gepirone , perospirone , tandospirone )Bay R 1531 Befiradol BMY-14802 Cannabidiol Dimemebfe Dopamine Ebalzotan Eltoprazine Enciprazine Ergolines (e.g., bromocriptine , cabergoline , dihydroergotamine , ergotamine , lisuride , LSD , methylergometrine (methylergonovine) , methysergide , pergolide )F-15063 F-15,599 Flesinoxan Flibanserin Flumexadol Lesopitron LY-293284 mCPP MKC-242 Naluzotan NBUMP Osemozotan Oxaflozane Pardoprunox Piclozotan Rauwolscine Repinotan Roxindole RU-24,969 S-14,506 S-14671 S-15535 Sarizotan Serotonin (5-HT) Sunepitron Tryptamines (e.g., 5-CT , 5-MeO-DMT , 5-MT , bufotenin , DMT , indorenate , N-Me-5-HT , psilocin , psilocybin )TGBA01AD U-92,016-A Urapidil Vilazodone Xaliproden Yohimbine
Antagonists: Atypical antipsychotics (e.g., iloperidone , risperidone , sertindole )Beta blockers (e.g., alprenolol , carteolol , cyanopindolol , iodocyanopindolol , isamoltane , oxprenolol , penbutolol , pindobind , pindolol , propranolol , tertatolol )BMY-7,378 CSP-2503 Dotarizine Ergolines (e.g., metergoline )Flopropione Isamoltane Lecozotan Mefway Metitepine (methiothepin) MIN-117 (WF-516) MPPF NAN-190 Robalzotan S-15535 SB-649,915 Spiperone Spiramide Spiroxatrine UH-301 WAY-100135 WAY-100635 Xylamidine
Unknown/unsorted: Acetryptine Ergolines (e.g., ergometrine (ergonovine) )
5-HT1B
Agonists: CGS-12066A CP-93129 CP-94253 CP-122,288 CP-135807 Eltoprazine Ergolines (e.g., bromocriptine , dihydroergotamine , ergotamine , methylergometrine (methylergonovine) , methysergide , pergolide )mCPP RU-24,969 Serotonin (5-HT) Triptans (e.g., avitriptan , donitriptan , eletriptan , sumatriptan , zolmitriptan )TFMPP Tryptamines (e.g., 5-BT , 5-CT , 5-MT , DMT )Vortioxetine
Antagonists: AR-A000002 Beta blockers (e.g., alprenolol , carteolol , isamoltane , oxprenolol , penbutolol , propranolol , tertatolol )Elzasonan Ergolines (e.g., metergoline )GR-127935 Isamoltane LY-393558 Metitepine (methiothepin) SB-216641 SB-236057 Yohimbine
Unknown/unsorted: Ergolines (e.g., cabergoline , ergometrine (ergonovine) , lisuride )
5-HT1D
Agonists: CP-122,288 CP-135807 Ergolines (e.g., bromocriptine , cabergoline , dihydroergotamine , ergotamine , LSD , methysergide )L-694247 mCPP PNU-142633 Serotonin (5-HT) TGBA01AD Triptans (e.g., almotriptan , avitriptan , donitriptan , eletriptan , frovatriptan , naratriptan , rizatriptan , sumatriptan , zolmitriptan )Tryptamines (e.g., 5-BT , 5-CT , 5-Et-DMT , 5-MT , 5-(nonyloxy)tryptamine , DMT )
Unknown/unsorted: Acetryptine Ergolines (e.g., lisuride , lysergol , pergolide )
5-HT1E
Agonists: BRL-54443 Ergolines (e.g., methysergide )Serotonin (5-HT) Triptans (e.g., eletriptan )Tryptamines (e.g., tryptamine )
Antagonists: Metitepine (methiothepin)
Unknown/unsorted: Ergolines (e.g., ergometrine (ergonovine) , lysergol , methylergometrine (methylergonovine)
5-HT1F
Agonists: BRL-54443 CP-122,288 Ergolines (e.g., bromocriptine , lysergol , methylergometrine (methylergonovine) methysergide )Lasmiditan LY-334370 Serotonin (5-HT) Triptans (e.g., eletriptan , naratriptan , sumatriptan )Tryptamines (e.g., 5-MT )
Antagonists: Mianserin Metitepine (methiothepin)
5-HT2
5-HT2A
Agonists: 25H/NB series (e.g., 25I-NBF , 25I-NBMD , 25I-NBOH , 25I-NBOMe , 25B-NBOMe , 25C-NBOMe , 25TFM-NBOMe , 2CBCB-NBOMe , 25CN-NBOH , 2CBFly-NBOMe )2Cs (e.g., 2C-B , 2C-E , 2C-I , 2C-T-2 , 2C-T-7 , 2C-T-21 )2C-B-FLY 2CB-Ind 5-Methoxytryptamines (5-MeO-DET , 5-MeO-DiPT , 5-MeO-DMT , 5-MeO-DPT , 5-MT )α-Alkyltryptamines (e.g., 5-Cl-αMT , 5-Fl-αMT , 5-MeO-αET , 5-MeO-αMT , α-Me-5-HT , αET , αMT )AL-34662 AL-37350A Bromo-DragonFLY Dimemebfe DMBMPP DOx (e.g., DOB , DOC , DOI , DOM )Efavirenz Ergolines (e.g., 1P-LSD , ALD-52 , bromocriptine , cabergoline , ergine (LSA) , ergometrine (ergonovine) , ergotamine , lisuride , LA-SS-Az , LSB , LSD , LSD-Pip , LSH , LSP , methylergometrine (methylergonovine) , pergolide )Flumexadol Jimscaline Lorcaserin MDxx (e.g., MDA (tenamfetamine) , MDMA (midomafetamine) , MDOH , MMDA )O-4310 Oxaflozane PHA-57378 PNU-22394 PNU-181731 RH-34 Phenethylamines (e.g., lophophine , mescaline )Piperazines (e.g., BZP , quipazine , TFMPP )Serotonin (5-HT) TCB-2 TFMFly Tryptamines (e.g., 5-BT , 5-CT , bufotenin , DET , DiPT , DMT , DPT , psilocin , psilocybin , tryptamine )
Antagonists: 5-I-R91150 5-MeO-NBpBrT Adatanserin Altanserin Antihistamines (e.g., cyproheptadine , hydroxyzine , ketotifen , perlapine )AMDA Atypical antipsychotics (e.g., amperozide , aripiprazole , asenapine , blonanserin , brexpiprazole , carpipramine , clocapramine , clorotepine , clozapine , fluperlapine , gevotroline , iloperidone , lurasidone , melperone , mosapramine , ocaperidone , olanzapine , paliperidone , quetiapine , risperidone , sertindole , zicronapine , ziprasidone , zotepine )Cinanserin CSP-2503 Deramciclane Dotarizine Eplivanserin Ergolines (e.g., amesergide , , LY-215,840 , mesulergine , metergoline , methysergide , sergolexole )Fananserin Flibanserin Glemanserin Ketanserin KML-010 LY-393558 mCPP Medifoxamine Metitepine (methiothepin) MIN-117 (WF-516) Naftidrofuryl Nantenine Nelotanserin Opiranserin (VVZ-149) Pelanserin Phenoxybenzamine Pimavanserin Pirenperone Pizotifen Pruvanserin Rauwolscine Ritanserin Roluperidone S-14671 Sarpogrelate Serotonin antagonists and reuptake inhibitors (e.g., etoperidone , hydroxynefazodone , lubazodone , mepiprazole , nefazodone , triazoledione , trazodone )TGBA01AD Teniloxazine Tetracyclic antidepressants (e.g., amoxapine , aptazapine , esmirtazapine , maprotiline , mianserin , mirtazapine )Tricyclic antidepressants (e.g., amitriptyline )Typical antipsychotics (e.g., chlorpromazine , fluphenazine , haloperidol , loxapine , perphenazine , pimozide , pipamperone , prochlorperazine , setoperone , spiperone , spiramide , thioridazine , thiothixene , trifluoperazine )Volinanserin Xylamidine Yohimbine
Unknown/unsorted: Ergolines (e.g., dihydroergotamine , nicergoline )
5-HT2B
Agonists: 4-Methylaminorex Aminorex Amphetamines (e.g., chlorphentermine , cloforex , dexfenfluramine , fenfluramine , levofenfluramine , norfenfluramine )BW-723C86 DOx (e.g., DOB , DOC , DOI , DOM )Ergolines (e.g., cabergoline , dihydroergocryptine , dihydroergotamine , ergotamine , methylergometrine (methylergonovine) , methysergide , pergolide )Lorcaserin MDxx (e.g., MDA (tenamfetamine) , MDMA (midomafetamine) , MDOH , MMDA )Piperazines (e.g., TFMPP )PNU-22394 Ro60-0175 Serotonin (5-HT) Tryptamines (e.g., 5-BT , 5-CT , 5-MT , α-Me-5-HT , bufotenin , DET , DiPT , DMT , DPT , psilocin , psilocybin , tryptamine )
Antagonists: Agomelatine Atypical antipsychotics (e.g., amisulpride , aripiprazole , asenapine , brexpiprazole , cariprazine , clozapine , , N-desmethylclozapine (norclozapine) , olanzapine , pipamperone , quetiapine , risperidone , ziprasidone )Cyproheptadine EGIS-7625 Ergolines (e.g., amesergide , bromocriptine , lisuride , , LY-272015 , mesulergine )Ketanserin LY-393558 mCPP Metadoxine Metitepine (methiothepin) Pirenperone Pizotifen Propranolol PRX-08066 Rauwolscine Ritanserin RS-127445 Sarpogrelate SB-200646 SB-204741 SB-206553 SB-215505 SB-228357 SDZ SER-082 Tegaserod Tetracyclic antidepressants (e.g., amoxapine , mianserin , mirtazapine )Trazodone Typical antipsychotics (e.g., chlorpromazine )TIK-301 Yohimbine
Unknown/unsorted: Ergolines (e.g., ergometrine (ergonovine) )
5-HT2C
Agonists: 2Cs (e.g., 2C-B , 2C-E , 2C-I , 2C-T-2 , 2C-T-7 , 2C-T-21 )5-Methoxytryptamines (5-MeO-DET , 5-MeO-DiPT , 5-MeO-DMT , 5-MeO-DPT , 5-MT )α-Alkyltryptamines (e.g., 5-Cl-αMT , 5-Fl-αMT , 5-MeO-αET , 5-MeO-αMT , α-Me-5-HT , αET , αMT )A-372159 AL-38022A Alstonine CP-809101 Dimemebfe DOx (e.g., DOB , DOC , DOI , DOM )Ergolines (e.g., ALD-52 , cabergoline , dihydroergotamine , ergine (LSA) , ergotamine , lisuride , LA-SS-Az , LSB , LSD , LSD-Pip , LSH , LSP , pergolide )Flumexadol Lorcaserin MDxx (e.g., MDA (tenamfetamine) , MDMA (midomafetamine) , MDOH , MMDA )MK-212 ORG-12962 ORG-37684 Oxaflozane PHA-57378 Phenethylamines (e.g., lophophine , mescaline )Piperazines (e.g., aripiprazole , BZP , mCPP , quipazine , TFMPP )PNU-22394 PNU-181731 Ro60-0175 Ro60-0213 Serotonin (5-HT) Tryptamines (e.g., 5-BT , 5-CT , bufotenin , DET , DiPT , DMT , DPT , psilocin , psilocybin , tryptamine )Vabicaserin WAY-629 WAY-161503 YM-348
Antagonists: Adatanserin Agomelatine Atypical antipsychotics (e.g., asenapine , clorotepine , clozapine , fluperlapine , iloperidone , melperone , olanzapine , paliperidone , quetiapine , risperidone , sertindole , ziprasidone , zotepine )Captodiame CEPC Cinanserin Cyproheptadine Deramciclane Desmetramadol Dotarizine Eltoprazine Ergolines (e.g., amesergide , bromocriptine , , LY-215,840 , mesulergine , metergoline , methysergide , sergolexole )Etoperidone Fluoxetine Ketanserin Ketotifen Latrepirdine (dimebolin) Medifoxamine Metitepine (methiothepin) Nefazodone Pirenperone Pizotifen Propranolol Ritanserin RS-102221 S-14671 SB-200646 SB-206553 SB-228357 SB-242084 SB-243213 SDZ SER-082 Tedatioxetine Tetracyclic antidepressants (e.g., amoxapine , aptazapine , esmirtazapine , maprotiline , mianserin , mirtazapine )TIK-301 Tramadol Trazodone Tricyclic antidepressants (e.g., amitriptyline , nortriptyline )Typical antipsychotics (e.g., chlorpromazine , loxapine , pimozide , pipamperone , thioridazine )Xylamidine
Unknown/unsorted: Efavirenz Ergolines (e.g., ergometrine (ergonovine) , methylergometrine (methylergonovine) )
5-HT3 –7
5-HT3
Agonists: Alcohols (e.g., butanol , ethanol (alcohol) , trichloroethanol )m-CPBG Phenylbiguanide Piperazines (e.g., BZP , mCPP , quipazine )RS-56812 Serotonin (5-HT) SR-57227 Tryptamines (e.g., 2-Me-5-HT , 5-CT , bufotenidine (5-HTQ) )Volatiles/gases (e.g., halothane , isoflurane , toluene , trichloroethane )YM-31636
Antagonists: Alosetron AS-8112 Atypical antipsychotics (e.g., clozapine , olanzapine , quetiapine )Azasetron Batanopride Bemesetron (MDL-72222) Bupropion Cilansetron CSP-2503 Dazopride Dolasetron Galanolactone Granisetron Hydroxybupropion Lerisetron Memantine Ondansetron Palonosetron Ramosetron Renzapride Ricasetron Tedatioxetine Tetracyclic antidepressants (e.g., amoxapine , mianserin , mirtazapine )Thujone Tropanserin Tropisetron Typical antipsychotics (e.g., loxapine )Volatiles/gases (e.g., nitrous oxide , sevoflurane , xenon )Vortioxetine Zacopride Zatosetron
5-HT4
Agonists: 5-MT BIMU8 Capeserod Cinitapride Cisapride CJ-033466 Dazopride Metoclopramide Mosapride Prucalopride PRX-03140 Renzapride RS-67,333 Serotonin (5-HT) Tegaserod Velusetrag Zacopride
5-HT5A
Agonists: Ergolines (e.g., 2-Br-LSD (BOL-148) , ergotamine , LSD )Serotonin (5-HT) Tryptamines (e.g., 5-CT )Valerenic Acid
Unknown/unsorted: Ergolines (e.g., metergoline , methysergide )Piperazines (e.g., naphthylpiperazine )
5-HT6
Agonists: Ergolines (e.g., dihydroergocryptine , dihydroergotamine , ergotamine , lisuride , LSD , mesulergine , metergoline , methysergide )Serotonin (5-HT) Tryptamines (e.g., 2-Me-5-HT , 5-BT , 5-CT , 5-MT , Bufotenin , E-6801 , E-6837 , EMD-386088 , EMDT , , , tryptamine )WAY-181187 WAY-208466
Antagonists: Atypical antipsychotics (e.g., aripiprazole , asenapine , clorotepine , clozapine , fluperlapine , iloperidone , olanzapine , tiospirone )AVN-101 AVN-211 Cerlapirdine EGIS-12,233 Idalopirdine Ketanserin Latrepirdine (dimebolin) Metitepine (methiothepin) MS-245 PRX-07034 Ritanserin Ro 04-6790 SB-258585 SB-271046 SB-357134 SB-399885 SB-742457 Tetracyclic antidepressants (e.g., amoxapine , mianserin )Tricyclic antidepressants (e.g., amitriptyline , clomipramine , doxepin , nortriptyline )Typical antipsychotics (e.g., chlorpromazine , loxapine )
Unknown/unsorted: Ergolines (e.g., 2-Br-LSD (BOL-148) , bromocriptine , lergotrile , pergolide )Piperazines (e.g., naphthylpiperazine )
5-HT7
Agonists: 8-OH-DPAT AS-19 Bifeprunox E-55888 Ergolines (e.g., LSD )LP-12 LP-44 RU-24,969 Sarizotan Serotonin (5-HT) Triptans (e.g., frovatriptan )Tryptamines (e.g., 5-CT , 5-MT , bufotenin , N-Me-5-HT )
Antagonists: Atypical antipsychotics (e.g., amisulpride , aripiprazole , asenapine , brexpiprazole , clorotepine , clozapine , fluperlapine , olanzapine , risperidone , sertindole , tiospirone , ziprasidone , zotepine )Butaclamol DR-4485 EGIS-12,233 Ergolines (e.g., 2-Br-LSD (BOL-148) , amesergide , bromocriptine , cabergoline , dihydroergotamine , ergotamine , , LY-215,840 , mesulergine , metergoline , methysergide , sergolexole )JNJ-18038683 Ketanserin LY-215,840 Metitepine (methiothepin) Ritanserin SB-258719 SB-269970 Spiperone Tetracyclic antidepressants (e.g., amoxapine , maprotiline , mianserin , mirtazapine )Tricyclic antidepressants (e.g., amitriptyline , clomipramine , imipramine )Typical antipsychotics (e.g., acetophenazine , chlorpromazine , chlorprothixene , fluphenazine , loxapine , pimozide )Vortioxetine
Unknown/unsorted: Ergolines (e.g., lisuride , pergolide )Piperazines (e.g., naphthylpiperazine )
See also: Receptor/signaling modulators Adrenergics Dopaminergics Melatonergics Monoamine reuptake inhibitors and releasing agents Monoamine metabolism modulators Monoamine neurotoxins