CD19
B-lymphocyte antigen CD19, also known as CD19 molecule (Cluster of Differentiation 19), B-Lymphocyte Surface Antigen B4, T-Cell Surface Antigen Leu-12 and CVID3 is a transmembrane protein that in humans is encoded by the gene CD19.[5][6] In humans, CD19 is expressed in all B lineage cells.[7][8] Contrary to some early doubts, human plasma cells do express CD19,[9] as confirmed by others.[10] CD19 plays two major roles in human B cells: on the one hand, it acts as an adaptor protein to recruit cytoplasmic signaling proteins to the membrane; on the other, it works within the CD19/CD21 complex to decrease the threshold for B cell receptor signaling pathways. Due to its presence on all B cells, it is a biomarker for B lymphocyte development, lymphoma diagnosis and can be utilized as a target for leukemia immunotherapies.[8]
Structure[]
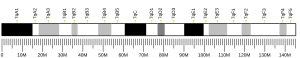
In humans, CD19 is encoded by the 7.41 kilobase CD19 gene located on the short arm of chromosome 16.[11][12] It contains at least fifteen exons, four that encode extracellular domain and nine that encode cytoplasmic domains, with a total of 556 amino acids.[12] Experiments show that there are multiple mRNA transcripts; however, only two have been isolated in vivo.[11]
CD19 is a 95 kd Type I transmembrane glycoprotein in the immunoglobulin superfamily (IgSF) with two extracellular C2-set Ig-like domains and a relatively large, 240 amino acid, cytoplasmic tail that is highly conserved among mammalian species.[11][13][14][15] The extracellular C2-type Ig-like domains are divided by a potential disulfide linked non-Ig-like domain and N-linked carbohydrate addition sites.[14][16] The cytoplasmic tail contains at least nine tyrosine residues near the C-terminus.[11][14] Within these residues, Y391, Y482, and Y513 have been shown to be essential to the biological functions of CD19.[17] Phenylalanine substitution for tyrosine at Y482 and Y513 leads to the inhibition of phosphorylation at the other tyrosines.[11][18]
Expression[]
CD19 is widely expressed during all phases of B cell development until terminal differentiation into plasma cells. During B cell lymphopoiesis, CD19 surface expression starts during immunoglobulin (Ig) gene rearrangement, which coincides during B lineage commitment from hematopoietic stem cell.[8] Throughout development, the surface density of CD19 is highly regulated.[11] CD19 expression in mature B cells is threefold higher than that in immature B cells.[11] CD19 is expressed on all normal, mitogen-stimulated, and malignant B cells, excluding plasma cells[inconsistent]. CD19 expression is even maintained in B lineage cells that undergo neoplastic transformation.[7][18] Because of its ubiquity on all B cells, it can function as a B cell marker and a target for immunotherapies targeting neoplastic lymphocytes.[8][11]
Function[]
Role in development & survival[]
Decisions to live, proliferate, differentiate, or die are continuously being made during B cell development.[19] These decisions are tightly regulated through BCR interactions and signaling. The presence of a functional BCR is necessary during antigen-dependent differentiation and for continued survival in the peripheral immune system.[14] Essential to the functionality of a BCR is the presence of CD19.[20] Experiments using CD19 knockout mice found that CD19 is essential for B cell differentiative events including the formation of B-1, germinal center, and marginal zone (MZ) B cells.[14][21][22] Analysis of mixed bone marrow chimeras suggest that prior to an initial antigen encounter, CD19 promotes the survival of naive recirculating B cells and increases the in vivo life span of B cells in the peripheral B cell compartment.[23] Ultimately, CD19 expression is integral to the propagation of BCR-induced survival signals and the maintenance of homeostasis through tonic signaling.
BCR-independent[]
Paired box transcription factor 5 (PAX5) plays a major role in B cell differentiation from pro B cell to mature B cell, the point at which the expression of non-B-lineage genes is permanently blocked.[23][24][25] Part of B cell differentiation is controlling c-MYC protein stability and steady-state levels through CD19, which acts as a PAX5 target and downstream effector of the PI3K-AKT-GSK3β axis. CD19 signaling, independent of BCR functions, increases c-MYC protein stability. Using a loss of function approach, researchers found reduced MYC levels in B cells of CD19 knockdown mice.[23] CD19 signaling involves the recruitment and activation of phosphoinositide 3-kinase (PI3K) and later downstream, the activation of protein kinase B (Akt). The Akt-GSK3β axis is necessary for MYC activation by CD19 in BCR-negative cells, with higher levels of Akt activation corresponding to higher levels of MYC.[23][26] CD19 is a crucial BCR-independent regulator of MYC-driven neoplastic growth in B cells since the CD19-MYC axis promotes cell expansion in vitro and in vivo.[23][26]
CD19/CD21 complex[]
On the cell surface, CD19 is the dominant signaling component of a multimolecular complex including CD21, a complement receptor, CD81, a tetraspanin membrane protein (TAPA-1), and CD225.[11][23] The CD19/CD21 complex arises from C3d binding to CD21; however, CD19 does not require CD21 for signal transduction. CD81, attached to CD19, is a part of the tetraspanin web, acts as a chaperone protein, and provides docking sites for molecules in various different signal transduction pathways.[11]
BCR-dependent[]
While colligated with the BCR, the CD19/CD21 complex bound to the antigen-complement complex can decrease the threshold for B cell activation. CD21, complement receptor 2, can bind fragments of C3 that have covalently attached to glycoconjugates by complement activation.[27] Recognition of an antigen by the complement system enables the CD19/CD21 complex and associated intracellular signaling molecules to crosslink to the BCR. This results in phosphorylation of the cytoplasmic tail of CD19 by BCR-associated tyrosine kinases, ensuing is the binding of additional Src-family kinases, augmentation of signaling through the BCR, and recruitment of PI3K. The localization of PI3K initiates another signaling pathway leading to Akt activation. Varying expression of CD19 on the cell surface modulates tyrosine phosphorylation and Akt kinase signaling and by extension, MHC class II mediated signaling.[11]
Activated spleen tyrosine kinase (Syk) leads to phosphorylation of the scaffold protein, BLNK, which provides multiple sites for tyrosine phosphorylation and recruits SH2-containing enzymes and adaptor proteins that can form various multiprotein signaling complexes. In this way, CD19 can modulate the threshold for B cell activation. This is important during primary immune response, prior to affinity maturation, amplifying the response of low affinity BCRs to low concentrations of antigen.[11][27]
Interactions[]
CD19 has been shown to interact with:
- CD81
- CD82
- Complement receptor 2
- VAV2
In disease[]
Autoimmunity & immunodeficiency[]
Mutations in CD19 are associated with severe immunodeficiency syndromes characterized by diminished antibody production.[28][29] Additionally, mutations in CD21 and CD81 can also underlie primary immunodeficiency due to their role in the CD19/CD21 complex formation.[30] These mutations can lead to hypogammaglobulinaemia as a result of poor response to antigen and defective immunological memory.[31] Researchers found changes in the constitution of B lymphocyte population and reduced amounts of switched memory B cells with high terminal differentiation potential in patients with Down Syndrome.[32] CD19 has also been implicated in autoimmune diseases, including rheumatoid arthritis and multiple sclerosis, and may be a useful treatment target.[13][16][33]
Mouse model research shows that CD19 deficiency can lead to hyporesponsiveness to transmembrane signals and weak T cell dependent humoral response, that in turn leads to an overall impaired humoral immune response.[21][22] Additionally CD19 plays a role in modulating MHC Class II expression and signaling, which can be affected by mutations. CD19 deficient B cells exhibit selective growth disadvantage; therefore, it is rare for CD19 to be absent in neoplastic B cells, as it is essential for development.[23]
Cancer[]
Since CD19 is a marker of B cells, the protein has been used to diagnose cancers that arise from this type of cell - notably B cell lymphomas, acute lymphoblastic leukemia (ALL), and chronic lymphocytic leukemia (CLL).[8] The majority of B cell malignancies express normal to high levels of CD19. The most current experimental anti-CD19 immunotoxins in development work by exploiting the widespread presence of CD19 on B cells, with expression highly conserved in most neoplastic B cells, to direct treatment specifically towards B-cell cancers.[13][34] However, it is now emerging that the protein plays an active role in driving the growth of these cancers, most intriguingly by stabilizing the concentrations of the MYC oncoprotein. This suggests that CD19 and its downstream signaling may be a more attractive therapeutic target than initially suspected.[23][26]
CD19-targeted therapies based on T cells that express CD19-specific chimeric antigen receptors (CARs) have been utilized for their antitumor abilities in patients with CD19+ lymphoma and leukemia, first against Non-Hodgkin's Lymphoma (NHL), then against CLL in 2011, and then against ALL in 2013.[8][35][36][37] CAR-19 T cells are genetically modified T cells that express a targeting moiety on their surface that confers T cell receptor (TCR) specificity towards CD19+ cells. CD19 activates the TCR signaling cascade that leads to proliferation, cytokine production, and ultimately lysis of the target cells, which in this case are CD19+ B cells. CAR-19 T cells are more effective than anti-CD19 immunotoxins because they can proliferate and remain in the body for a longer period of time. This comes with a caveat since now CD19− immune escape facilitated by splice variants, point mutations, and lineage switching can form as a major form of therapeutic resistance for patients with ALL.[38]
References[]
- ^ a b c GRCh38: Ensembl release 89: ENSG00000177455 - Ensembl, May 2017
- ^ a b c GRCm38: Ensembl release 89: ENSMUSG00000030724 - Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ "Entrez Gene: CD19 CD19 molecule".
- ^ Tedder TF, Isaacs CM (July 1989). "Isolation of cDNAs encoding the CD19 antigen of human and mouse B lymphocytes. A new member of the immunoglobulin superfamily". Journal of Immunology. 143 (2): 712–7. PMID 2472450.
- ^ a b Schroeder HW, Rich RR (2013). "Chapter 4: Antigen receptor genes, gene products, and co-receptors". Clinical immunology: Principles and Practice (4th ed.). London. pp. 47–51. ISBN 978-0-7234-3691-1. OCLC 823736017.
- ^ a b c d e f Scheuermann RH, Racila E (August 1995). "CD19 antigen in leukemia and lymphoma diagnosis and immunotherapy". Leukemia & Lymphoma. 18 (5–6): 385–97. doi:10.3109/10428199509059636. PMID 8528044.
- ^ Merville P, Déchanet J, Desmoulière A, Durand I, de Bouteiller O, Garrone P, et al. (January 1996). "Bcl-2+ tonsillar plasma cells are rescued from apoptosis by bone marrow fibroblasts". The Journal of Experimental Medicine. 183 (1): 227–36. doi:10.1084/jem.183.1.227. PMC 2192413. PMID 8551226.
- ^ Martín P, Santón A, Bellas C (April 2004). "Neural cell adhesion molecule expression in plasma cells in bone marrow biopsies and aspirates allows discrimination between multiple myeloma, monoclonal gammopathy of uncertain significance and polyclonal plasmacytosis". Histopathology. 44 (4): 375–80. doi:10.1111/j.1365-2559.2004.01834.x. PMID 15049904. S2CID 45937555.
- ^ a b c d e f g h i j k l Wang K, Wei G, Liu D (November 2012). "CD19: a biomarker for B cell development, lymphoma diagnosis and therapy". Experimental Hematology & Oncology. 1 (1): 36. doi:10.1186/2162-3619-1-36. PMC 3520838. PMID 23210908.
- ^ a b Zhou LJ, Ord DC, Omori SA, Tedder TF (1992). "Structure of the genes encoding the CD19 antigen of human and mouse B lymphocytes". Immunogenetics. 35 (2): 102–11. doi:10.1007/bf00189519. PMID 1370948. S2CID 7182703.
- ^ a b c Mei HE, Schmidt S, Dörner T (November 2012). "Rationale of anti-CD19 immunotherapy: an option to target autoreactive plasma cells in autoimmunity". Arthritis Research & Therapy. 14 Suppl 5 (5): S1. doi:10.1186/ar3909. PMC 3535716. PMID 23281743.
- ^ a b c d e Haas KM, Tedder TF (2005). Mechanisms of Lymphocyte Activation and Immune Regulation X. Advances in Experimental Medicine and Biology. Vol. 560. Springer, Boston, MA. pp. 125–139. doi:10.1007/0-387-24180-9_16. ISBN 978-0-387-24188-3. PMID 15934172.
- ^ Tedder TF, Isaacs CM (July 1989). "Isolation of cDNAs encoding the CD19 antigen of human and mouse B lymphocytes. A new member of the immunoglobulin superfamily". Journal of Immunology. 143 (2): 712–7. PMID 2472450.
- ^ a b Tedder TF (October 2009). "CD19: a promising B cell target for rheumatoid arthritis". Nature Reviews. Rheumatology. 5 (10): 572–7. doi:10.1038/nrrheum.2009.184. PMID 19798033. S2CID 6143992.
- ^ Del Nagro CJ, Otero DC, Anzelon AN, Omori SA, Kolla RV, Rickert RC (2005). "CD19 function in central and peripheral B-cell development". Immunologic Research. 31 (2): 119–31. doi:10.1385/IR:31:2:119. PMID 15778510. S2CID 45145420.
- ^ a b Carter RH, Wang Y, Brooks S (2002). "Role of CD19 signal transduction in B cell biology". Immunologic Research. 26 (1–3): 45–54. doi:10.1385/IR:26:1-3:045. PMID 12403344. S2CID 35818699.
- ^ Otero DC, Anzelon AN, Rickert RC (January 2003). "CD19 function in early and late B cell development: I. Maintenance of follicular and marginal zone B cells requires CD19-dependent survival signals". Journal of Immunology. 170 (1): 73–83. doi:10.4049/jimmunol.170.1.73. PMID 12496385.
- ^ Sato S (December 1999). "CD19 is a central response regulator of B lymphocyte signaling thresholds governing autoimmunity". Journal of Dermatological Science. 22 (1): 1–10. doi:10.1016/s0923-1811(99)00043-2. PMID 10651223.
- ^ a b Rickert RC, Rajewsky K, Roes J (July 1995). "Impairment of T-cell-dependent B-cell responses and B-1 cell development in CD19-deficient mice". Nature. 376 (6538): 352–5. Bibcode:1995Natur.376..352R. doi:10.1038/376352a0. PMID 7543183. S2CID 4337673.
- ^ a b Engel P, Zhou LJ, Ord DC, Sato S, Koller B, Tedder TF (July 1995). "Abnormal B lymphocyte development, activation, and differentiation in mice that lack or overexpress the CD19 signal transduction molecule". Immunity. 3 (1): 39–50. doi:10.1016/1074-7613(95)90157-4. PMID 7542548.
- ^ a b c d e f g h Chung EY, Psathas JN, Yu D, Li Y, Weiss MJ, Thomas-Tikhonenko A (June 2012). "CD19 is a major B cell receptor-independent activator of MYC-driven B-lymphomagenesis". The Journal of Clinical Investigation. 122 (6): 2257–66. doi:10.1172/jci45851. PMC 3366393. PMID 22546857.
- ^ Monroe JG (April 2006). "ITAM-mediated tonic signalling through pre-BCR and BCR complexes". Nature Reviews. Immunology. 6 (4): 283–94. doi:10.1038/nri1808. PMID 16557260. S2CID 28197010.
- ^ Maier H, Ostraat R, Parenti S, Fitzsimmons D, Abraham LJ, Garvie CW, Hagman J (October 2003). "Requirements for selective recruitment of Ets proteins and activation of mb-1/Ig-alpha gene transcription by Pax-5 (BSAP)". Nucleic Acids Research. 31 (19): 5483–9. doi:10.1093/nar/gkg785. PMC 206479. PMID 14500810.
- ^ a b c Poe JC, Minard-Colin V, Kountikov EI, Haas KM, Tedder TF (September 2012). "A c-Myc and surface CD19 signaling amplification loop promotes B cell lymphoma development and progression in mice". Journal of Immunology. 189 (5): 2318–25. doi:10.4049/jimmunol.1201000. PMC 3426298. PMID 22826319.
- ^ a b Morbach H, Schickel JN, Cunningham-Rundles C, Conley ME, Reisli I, Franco JL, Meffre E (March 2016). "CD19 controls Toll-like receptor 9 responses in human B cells". The Journal of Allergy and Clinical Immunology. 137 (3): 889–98.e6. doi:10.1016/j.jaci.2015.08.040. PMC 4783287. PMID 26478008.
- ^ Pesando JM, Bouchard LS, McMaster BE (December 1989). "CD19 is functionally and physically associated with surface immunoglobulin". The Journal of Experimental Medicine. 170 (6): 2159–64. doi:10.1084/jem.170.6.2159. PMC 2189531. PMID 2479707.
- ^ van Zelm MC, Reisli I, van der Burg M, Castaño D, van Noesel CJ, van Tol MJ, Woellner C, Grimbacher B, Patiño PJ, van Dongen JJ, Franco JL (May 2006). "An antibody-deficiency syndrome due to mutations in the CD19 gene". The New England Journal of Medicine. 354 (18): 1901–12. doi:10.1056/nejmoa051568. PMID 16672701.
- ^ Carsetti R, Valentini D, Marcellini V, Scarsella M, Marasco E, Giustini F, Bartuli A, Villani A, Ugazio AG (March 2015). "Reduced numbers of switched memory B cells with high terminal differentiation potential in Down syndrome". European Journal of Immunology. 45 (3): 903–14. doi:10.1002/eji.201445049. PMC 4674966. PMID 25472482.
- ^ Verstegen RH, Driessen GJ, Bartol SJ, van Noesel CJ, Boon L, van der Burg M, et al. (December 2014). "Defective B-cell memory in patients with Down syndrome". The Journal of Allergy and Clinical Immunology. 134 (6): 1346–1353.e9. doi:10.1016/j.jaci.2014.07.015. PMID 25159464.
- ^ Seckin AN, Ozdemir H, Ceylan A, Artac H (February 2018). "Age-related alterations of the CD19 complex and memory B cells in children with Down syndrome". Clinical and Experimental Medicine. 18 (1): 125–131. doi:10.1007/s10238-017-0457-2. PMID 28197808. S2CID 19318246.
- ^ Fujimoto M, Sato S (April 2007). "B cell signaling and autoimmune diseases: CD19/CD22 loop as a B cell signaling device to regulate the balance of autoimmunity". Journal of Dermatological Science. 46 (1): 1–9. doi:10.1016/j.jdermsci.2006.12.004. hdl:2297/3661. PMID 17223015.
- ^ Hiepe F, Dörner T, Hauser AE, Hoyer BF, Mei H, Radbruch A (March 2011). "Long-lived autoreactive plasma cells drive persistent autoimmune inflammation". Nature Reviews. Rheumatology. 7 (3): 170–8. doi:10.1038/nrrheum.2011.1. PMID 21283146. S2CID 43750896.
- ^ Porter DL, Levine BL, Kalos M, Bagg A, June CH (August 2011). "Chimeric antigen receptor-modified T cells in chronic lymphoid leukemia". The New England Journal of Medicine. 365 (8): 725–33. doi:10.1056/nejmoa1103849. PMC 3387277. PMID 21830940.
- ^ Sadelain M (December 2017). "CD19 CAR T Cells". Cell. 171 (7): 1471. doi:10.1016/j.cell.2017.12.002. PMID 29245005.
- ^ Clinical trial number NCT01493453 for "A Phase I Study of CD19 Specific T Cells in CD19 Positive Malignancy" at ClinicalTrials.gov
- ^ Velasquez MP, Gottschalk S (January 2017). "Targeting CD19: the good, the bad, and CD81". Blood. 129 (1): 9–10. doi:10.1182/blood-2016-11-749143. PMC 5216268. PMID 28057672.
Further reading[]
- Goldsby, Richard A.; Kindt, Thomas J.; Osborne, Barbara A. (2006). Kuby Immunology. San Francisco: W. H. Freeman. ISBN 978-0-7167-8590-3.
- Ishikawa H, Tsuyama N, Mahmoud MS, Fujii R, Abroun S, Liu S, Li FJ, Kawano MM (March 2002). "CD19 expression and growth inhibition of tumours in human multiple myeloma". Leukemia & Lymphoma. 43 (3): 613–6. doi:10.1080/10428190290012146. PMID 12002767. S2CID 20765908.
- Zhou LJ, Ord DC, Omori SA, Tedder TF (1992). "Structure of the genes encoding the CD19 antigen of human and mouse B lymphocytes". Immunogenetics. 35 (2): 102–11. doi:10.1007/BF00189519. PMID 1370948. S2CID 7182703.
- Carter RH, Fearon DT (April 1992). "CD19: lowering the threshold for antigen receptor stimulation of B lymphocytes". Science. 256 (5053): 105–7. Bibcode:1992Sci...256..105C. doi:10.1126/science.1373518. PMID 1373518.
- Kozmik Z, Wang S, Dörfler P, Adams B, Busslinger M (June 1992). "The promoter of the CD19 gene is a target for the B-cell-specific transcription factor BSAP". Molecular and Cellular Biology. 12 (6): 2662–72. doi:10.1128/mcb.12.6.2662. PMC 364460. PMID 1375324.
- Bradbury LE, Kansas GS, Levy S, Evans RL, Tedder TF (November 1992). "The CD19/CD21 signal transducing complex of human B lymphocytes includes the target of antiproliferative antibody-1 and Leu-13 molecules". Journal of Immunology. 149 (9): 2841–50. PMID 1383329.
- Matsumoto AK, Kopicky-Burd J, Carter RH, Tuveson DA, Tedder TF, Fearon DT (January 1991). "Intersection of the complement and immune systems: a signal transduction complex of the B lymphocyte-containing complement receptor type 2 and CD19". The Journal of Experimental Medicine. 173 (1): 55–64. doi:10.1084/jem.173.1.55. PMC 2118751. PMID 1702139.
- Zhou LJ, Ord DC, Hughes AL, Tedder TF (August 1991). "Structure and domain organization of the CD19 antigen of human, mouse, and guinea pig B lymphocytes. Conservation of the extensive cytoplasmic domain". Journal of Immunology. 147 (4): 1424–32. PMID 1714482.
- Stamenkovic I, Seed B (September 1988). "CD19, the earliest differentiation antigen of the B cell lineage, bears three extracellular immunoglobulin-like domains and an Epstein-Barr virus-related cytoplasmic tail". The Journal of Experimental Medicine. 168 (3): 1205–10. doi:10.1084/jem.168.3.1205. PMC 2189043. PMID 2459292.
- Ord DC, Edelhoff S, Dushkin H, Zhou LJ, Beier DR, Disteche C, Tedder TF (1994). "CD19 maps to a region of conservation between human chromosome 16 and mouse chromosome 7". Immunogenetics. 39 (5): 322–8. doi:10.1007/BF00189228. PMID 7513297. S2CID 9336224.
- Weng WK, Jarvis L, LeBien TW (December 1994). "Signaling through CD19 activates Vav/mitogen-activated protein kinase pathway and induces formation of a CD19/Vav/phosphatidylinositol 3-kinase complex in human B cell precursors". The Journal of Biological Chemistry. 269 (51): 32514–21. doi:10.1016/S0021-9258(18)31664-8. PMID 7528218.
- Myers DE, Jun X, Waddick KG, Forsyth C, Chelstrom LM, Gunther RL, Tumer NE, Bolen J, Uckun FM (October 1995). "Membrane-associated CD19-LYN complex is an endogenous p53-independent and Bc1-2-independent regulator of apoptosis in human B-lineage lymphoma cells". Proceedings of the National Academy of Sciences of the United States of America. 92 (21): 9575–9. Bibcode:1995PNAS...92.9575M. doi:10.1073/pnas.92.21.9575. PMC 40844. PMID 7568175.
- Chalupny NJ, Aruffo A, Esselstyn JM, Chan PY, Bajorath J, Blake J, Gilliland LK, Ledbetter JA, Tepper MA (October 1995). "Specific binding of Fyn and phosphatidylinositol 3-kinase to the B cell surface glycoprotein CD19 through their src homology 2 domains". European Journal of Immunology. 25 (10): 2978–84. doi:10.1002/eji.1830251040. PMID 7589101. S2CID 9310907.
- Tuscano JM, Engel P, Tedder TF, Agarwal A, Kehrl JH (June 1996). "Involvement of p72syk kinase, p53/56lyn kinase and phosphatidyl inositol-3 kinase in signal transduction via the human B lymphocyte antigen CD22". European Journal of Immunology. 26 (6): 1246–52. doi:10.1002/eji.1830260610. PMID 8647200. S2CID 29471624.
- Carter RH, Doody GM, Bolen JB, Fearon DT (April 1997). "Membrane IgM-induced tyrosine phosphorylation of CD19 requires a CD19 domain that mediates association with components of the B cell antigen receptor complex". Journal of Immunology. 158 (7): 3062–9. PMID 9120258.
- Husson H, Mograbi B, Schmid-Antomarchi H, Fischer S, Rossi B (May 1997). "CSF-1 stimulation induces the formation of a multiprotein complex including CSF-1 receptor, c-Cbl, PI 3-kinase, Crk-II and Grb2". Oncogene. 14 (19): 2331–8. doi:10.1038/sj.onc.1201074. PMID 9178909.
- Khine AA, Firtel M, Lingwood CA (August 1998). "CD77-dependent retrograde transport of CD19 to the nuclear membrane: functional relationship between CD77 and CD19 during germinal center B-cell apoptosis". Journal of Cellular Physiology. 176 (2): 281–92. doi:10.1002/(SICI)1097-4652(199808)176:2<281::AID-JCP6>3.0.CO;2-K. PMID 9648915.
- Thunberg U, Gidlöf C, Bånghagen M, Sällström JF, Sundström C, Tötterman T (1998). "HpaII polymerase chain reaction restriction fragment length polymorphism in the human CD19 gene on 16p11". Human Heredity. 48 (4): 230–1. doi:10.1159/000022806. PMID 9694255. S2CID 32699676.
- Horváth G, Serru V, Clay D, Billard M, Boucheix C, Rubinstein E (November 1998). "CD19 is linked to the integrin-associated tetraspans CD9, CD81, and CD82". The Journal of Biological Chemistry. 273 (46): 30537–43. doi:10.1074/jbc.273.46.30537. PMID 9804823.
- Buhl AM, Cambier JC (April 1999). "Phosphorylation of CD19 Y484 and Y515, and linked activation of phosphatidylinositol 3-kinase, are required for B cell antigen receptor-mediated activation of Bruton's tyrosine kinase". Journal of Immunology. 162 (8): 4438–46. PMID 10201980.
External links[]
- Mouse CD Antigen Chart
- Human CD Antigen Chart
- Human CD19 genome location and CD19 gene details page in the UCSC Genome Browser.
This article incorporates text from the United States National Library of Medicine, which is in the public domain.
- Genes on human chromosome 16
- Clusters of differentiation
- Biomarkers